Translate this page into:
Worldwide incidence of suicidal thoughts, attempts, and mortality in systemic lupus erythematosus
*Corresponding author: E-mail address: akp.bt@buodisha.edu.in (A. Panda), shhaque@jazanu.edu.sa (S. Haque)
-
Received: ,
Accepted: ,
Abstract
The presence of suicidal thoughts, attempts, and fatalities in people with systemic lupus erythematosus (SLE) has been reported in various populations, with different studies showing varying rates. This meta-analysis aims to assess the global prevalence of suicidal thoughts, attempts, and deaths among individuals diagnosed with SLE. A comprehensive search of articles was conducted across several literature databases, such as PubMed, Scopus, and ScienceDirect, to identify relevant studies. The literature search was completed on December 6, 2023. The presence of publication bias was assessed using Egger’s regression analysis along with funnel plots, while Cochrane Q statistics and I square (I2) values were utilized to analyze heterogeneity. All statistical evaluations were performed using the Comprehensive Meta-Analysis Software version 4. According to the inclusion and exclusion criteria, eleven studies encompassing 1,515 SLE patients were analyzed to assess the prevalence of systemic inflammation (SI). The analysis revealed a 16.8 percent prevalence in the studied populations. Similarly, a total of four and six studies enrolled 3196 and 4134 SLE patients for the calculation of SA and actual suicide frequency in SLE patients, respectively, and the analysis revealed a 2.7 percent and 0.9 percent prevalence of SA and suicidal death, respectively. The current meta-analysis indicates that nearly 17% of SLE patients experience suicidal thoughts, 3% have attempted suicide, and about 1% of SLE patients have died by suicide. To prevent suicidal attempts among SLE patients, clinicians must screen their patients for suicidal ideation and refer them to the appropriate mental health providers.
Keywords
Attempts
Ideation
Meta-analysis
Sensitivity analysis
Suicide
Systemic lupus erythematosus
1. Introduction
Systemic lupus erythematosus (SLE) is marked by the development of autoantibodies that affect multiple organ systems, leading to a wide range of organ dysfunction. Patients with SLE exhibit diverse clinical manifestations, with neuropsychiatric SLE (NPSLE) occurring in 6% to 91% of cases (Sarwar et al., 2021). Depression and anxiety are among the primary psychiatric symptoms observed in NPSLE (Zhang et al., 2017; Moustafa et al., 2020). While suicidal tendencies are not recognized as a clinical manifestation of NPSLE, some SLE patients may experience suicidal thoughts or have a background of attempting suicide (Parperis et al., 2022). This may affect mental well-being and enhance the likelihood of suicidal thoughts in individuals with SLE (Lau and Mak 2009).
Annually, more than 7 lakh people worldwide die by suicide, making it the fourth most common cause of mortality among individuals in the age group of 15-29 years (WHO 2021). The impact of suicide extends beyond individuals to families, communities, and nations. In 2019, economically developing countries accounted for 77% of suicides worldwide. SLE patients often experience a lower quality of life due to chronic pain, fatigue, and organ impairment (Franco et al., 2014; Kawka et al., 2021). The persistent nature of SLE and its impact on daily life can lead to frustration, hopelessness, and despair (Somers et al., 2012). Psychiatric comorbidities, especially major depressive episodes, are commonly linked to SLE and significantly enhance the risk of suicidal ideation (Somers et al., 2012). Approximately one-third of SLE patients are treated with glucocorticoids (Ruiz-Irastorza et al., 2020) that have been associated with mental health issues (Judd et al., 2014; Yatomi et al., 2020; Kazi and Hoque 2021). The prevalence of depression in SLE patients ranges from approximately 20% to 46% across different studies (Dehghan et al., 2023; Hasan et al., 2024) and is a significant contributing factor to suicide risk (Bachmann 2018). Nevertheless, there is a scarcity of evidence that specifically addresses suicidal behaviors in patients with SLE (Palagini et al., 2013; Hajduk et al., 2016). Although the exact frequency of suicides among this group is not clearly defined, research suggests that individuals with SLE face a higher risk of suicide relative to both the general public and those with other long-term health issues (Li et al., 2018; Parperis et al., 2022).
The incidence of suicidal thoughts, attempts, and deaths among individuals with SLE is unclear and varies across studies. Many epidemiological studies do not include information on suicidal intentions, attempts, or the count of recorded suicides within the duration of the study. The variations in the prevalence of suicidal ideation may be attributed to the use of different diagnostic criteria across studies. Additionally, genetic factors are known to significantly influence suicidal behavior, and these factors vary across different populations and ethnicities. Meta-analysis is a robust procedure that systematically integrates data from prior studies with comparable findings, calculates the combined results, and draws firm conclusions with increased statistical power. This study aims to address the gap in understanding the global prevalence and patterns of suicidal behaviors among patients with SLE. By conducting a thorough meta-analysis of existing literature, this research seeks to provide accurate estimates of suicidal ideation, attempts, and completed suicides on a global scale. It will synthesize data from various geographical regions and clinical settings, creating a more comprehensive overview of suicidal behaviors in SLE patients and identifying potential risk factors. This information may serve as a basis for developing psychological interventions for SLE patients.
2. Materials and methods
2.1 Literature search
The systematic review adhered to PRISMA guidelines (Panda 2024). Literature searches were performed across multiple databases, including Google Scholar, PubMed, Scopus, and ScienceDirect, using keywords such as “Suicidal ideation in Systemic Lupus Erythematosus,” “Suicidal ideation in SLE,” “Suicide and Systemic Lupus Erythematosus,” “Suicide and SLE,” “Suicidal attempt and Systemic Lupus Erythematosus,” and “Suicidal attempt and SLE”. Two independent researchers reviewed the titles and abstracts of potential studies, and eligible papers meeting the criteria were downloaded for data extraction. The final search concluded on December 30, 2023.
2.2 Inclusion and exclusion criteria
Stringent inclusion and exclusion criteria were established to maintain the data’s relevance. The inclusion criteria specified that studies must focus on SLE patients and offer information regarding suicidal thoughts, attempts, or fatalities, with evaluations carried out using validated techniques. Exclusion criteria included data specific to other diseases or presented only in abstracts or conference proceedings, resulting in the exclusion of those data. The research plan has been registered in the PROSPERO database under the registration number CRD42023488976.
2.3 Data abstraction
Data extraction was conducted independently by two authors and included information on suicidal ideation, attempts, and deaths, as well as patient demographics such as age (mean ± standard deviation or median with range in years) and disease duration (mean ± standard deviation or median with range in years). The diagnostic criteria for both SLE and suicidal thoughts were also documented. Subsequently, the studies were categorized into three groups: the occurrence of suicidal ideation, the incidence of suicide attempts, and the rate of suicide fatalities among SLE patients.
2.4 Quality assessment
Two researchers independently assessed the risk of bias utilizing the Joanna Briggs Institute checklist 21 for cross-sectional studies, as detailed in Supplementary Table S1a. The quality of non-randomized trials, cohort studies, and case-control studies was evaluated using the Newcastle-Ottawa Scale (NOS) (Wells et al., 2000), as shown in Supplementary Table S1b,c. Additionally, a NOS modified version was utilized in earlier reviews to assess the quality of uncontrolled studies (Murad et al., 2018), as shown in Supplementary Tables S1d and S2. The NOS assessment was conducted under three main categories: i) subject selection (0-4 stars), ii) subject comparison (0-2 stars), and iii) clinical outcomes (0-3 stars) (Wells et al., 2000). Qualitative scores were indicated by stars, and a report with a total score of five or more stars was considered high quality according to NOS guidelines. When there were differences in the NOS score for a specific study between the two authors, they addressed it through discussion.
2.5 Statistical analysis
The statistical analyses of the data were done using Comprehensive Meta-Analysis software (CMA) v4 by Biostat Inc. USA. Publication bias was examined by Egger’s regression analysis and funnel plots. Study heterogeneity was evaluated with Cochrane Q and I square (I2) statistics, guiding the choice between fixed-effect and random-effect models. Prevalence figures of suicidal ideation, attempts, and deaths were calculated with a cumulative event rate and 95% confidence interval. A sensitivity analysis was also conducted by excluding individual studies to test the accuracy of the results.
3. Results
3.1 Literature search and eligible reports
Searching the various databases using predefined keywords till December 6, 2023, yielded 3310 articles (PubMed=1195, Scopus=859, Science Direct=1256). We found 18 eligible articles, (Kellum and Haserick 1964; Dubois et al., 1974; Wallace et al., 1981; Swaak et al., 1989; Cohen and Li 1992; Ishikura et al., 2001; Karassa et al., 2003; Li-Yu and Navarra 2007; Jarpa et al., 2011; Xie et al., 2012; Zakeri et al., 2012; Mok et al., 2014; Raafat et al., 2015; Tang et al., 2015; Hajduk et al., 2016; Jalenques et al., 2017; Buji et al., 2018; Grover et al., 2023), for inclusion in the current meta-analysis after careful screening using predefined inclusion criteria. Fig. 1 depicts the search strategies in detail. Out of the 18 articles reviewed, 11 provided data on suicidal ideation (Ishikura et al., 2001; Li-Yu and Navarra 2007; Jarpa et al., 2011; Xie et al., 2012; Zakeri et al., 2012; Mok et al., 2014; Raafat et al., 2015; Hajduk et al., 2016; Jalenques et al., 2017; Buji et al., 2018; Grover et al., 2023), four reported suicide attempts (Karassa et al., 2003; Mok et al., 2014; Tang et al., 2015; Jalenques et al., 2017), and six included information on suicide-related deaths among SLE patients (Kellum and Haserick 1964; Dubois et al., 1974; Wallace et al., 1981; Swaak et al., 1989; Cohen and Li 1992; Li-Yu and Navarra 2007) (Table 1). Two studies contained data on both suicidal ideation and attempts (Mok et al., 2014; Jalenques et al., 2017), while one study covered both suicidal ideation and deaths due to suicide in SLE patients (Li-Yu and Navarra 2007). All studies were assessed using NOS, and only those scoring five or more stars were included in the meta-analysis.
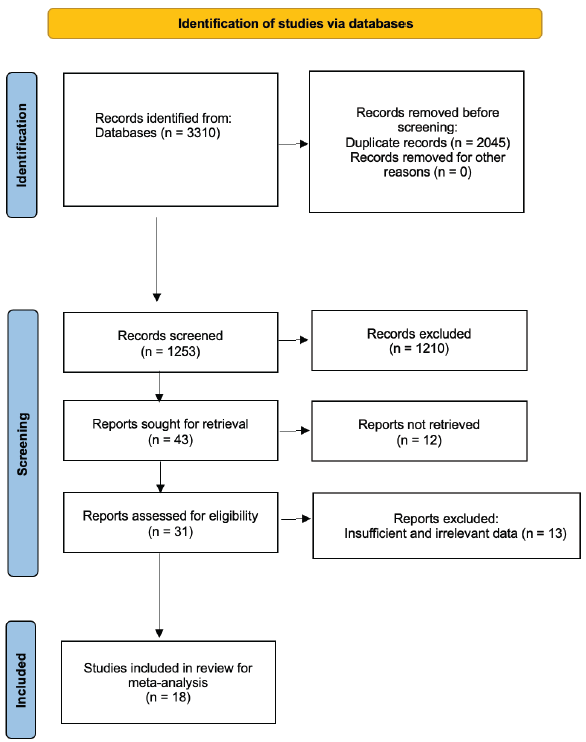
- PRISMA flow diagram outlining the selection of studies included in this meta-analysis.
| Principal author’s name & year | Nation | Study type | Total number of SLE patients | Male | Female | Mean age ± SD/ median (IQR) years | Disease duration ± SD/ median (IQR) years | Count of patients with suicidal ideation | Count of patients with suicidal attempts | Count of patients suicide (follow-up periods) | SI/SA diagnosis criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Grover et al. 2023 | India | Cross sectional | 79 | 9 | 70 | 30.1 ± 11.2 | 3.89 ± 3.2 | 35 | NR | NR | ICD-10 and PHQ-9 |
| Buji et al. 2017 | Malaysia | Cross sectional | 130 | 8 | 122 | 37 (18-73) | NR | 7 | NR | NR | Columbia-Suicidal Severity Rating Scale |
| Jalenques et al. 2017 | France | Case-control | 60 | 13 | 47 | 46.8 ± 13.9 | 9.7 ± 7.8 | 12 | 4 | NR | Mini International Neuropsychiatric Interview (MINI 5.0.0) |
| Hajduk et al. 2015 | Poland | Cross sectional | 53 | 5 | 48 | 43.79 ± 11.66 | 11.23 ± 7.74 | 14 | NR | NR | Neuropsychiatric Questionnaire (NP-Q) |
| Raafat et al. 2015 | Egypt | Case-control | 50 | 0 | 50 | 27.9 ± 6.28 | 5.5 ± 4.5 | 10 | NR | NR | Beck Suicidal Ideation Scale (BSI) |
| Tang et al. 2015 | Taiwan | Case series | 2469 | NR | NR | NR | NR | NR | 8 | NR | NR |
| Mok et al. 2014 | Hong Kong | Cross sectional | 367 | 18 | 349 | 40.2 ± 13 | 9.3 ± 7.2 | 44 | 45 | NR | Beck Scale for Suicidal Ideation (BSSI) |
| Xie et al. 2012 | China | Cross sectional | 285 | 18 | 267 | 33.98 ± 12.98 | 1.33 (0.21 to 4.96) | 98 | NR | NR | Beck Depression Inventory (BDI) |
| Zakeri et al. 2012 | Iran | Cross sectional | 85 | 8 | 77 | NR | NR | 9 | NR | NR | Beck’s Depression Inventory (BDI) |
| Jarpa et al. 2011 | Chile | Cross sectional | 83 | 7 | 76 | 39 (range 16-72) | 5 (0.1 to 40) | 8 | NR | NR | Mini-Mental State Examination (MMSE) scale |
| Li-Yu et al. 2007 | Philippines | Cross sectional | 275 | 0 | 275 | 32.57 ± 12.26 | 5.82 ± 4.98 | 42 | NR | 2 (5 months) | Beck Depression Inventory (BDI) II |
| Karassa et al. 2003 | United Kingdom | Case series | 300 | NR | NR | NR | NR | NR | 5 | NR | Medical Record Documentation |
| Ishikura et al. 2001 | Japan | Cross sectional | 84 | 0 | 84 | 43.1 ± 12.1 | 10.9 ± 6.8 | 7 | NR | NR | Cornell Medical Index (CMI) Health Questionnaire |
| Cohen et al. 1992 | Hong Kong | Retrospective cohort | 123 | NR | NR | NR | 3.1 (0.12 to 15.83) | NR | NR | 2 (4 years) | NR |
| Swaak et al. 1989 | Netherland | Prospective cohort | 110 | 16 | 94 | NR | NR | NR | NR | 1 (10 years) | NR |
| Wallace et al. 1981 | Los Angeles | Prospective cohort | 609 | NR | NR | NR | NR | NR | NR | 4 (30 years) | NR |
| Dubois et al. 1974 | USA | Case series | 249 | NR | NR | NR | NR | NR | NR | 3 (28 years) | NR |
| Kellum et al. 1964 | USA | Prospective cohort | 299 | NR | NR | NR | NR | NR | NR | 2 (11 years) | NR |
Note: Data are presented in number. SD: standard deviation, IQR: inter quartile range, NR: Not reported, SLE: Systemic lupus erythematosus, SI: Suicidal ideation, SA: Suicidal attempts, ICD: International Classification of Diseases, PHQ: Patient health questionnaire.
3.2 Publication bias
Funnel plots (Fig. 2) and Egger’s regression analysis were utilized to assess publication bias in this study. The results indicated no evidence of publication bias for the prevalence of suicidal ideation (intercept: -3.56, 95%CI= -8.83 to 1.70, p=0.16), suicide attempts (intercept: -7.45, 95%CI= -31.76 to 16.86, p=0.31), or completed suicides (intercept: 0.57, 95%CI= -2.89 to 4.04, p=0.66).
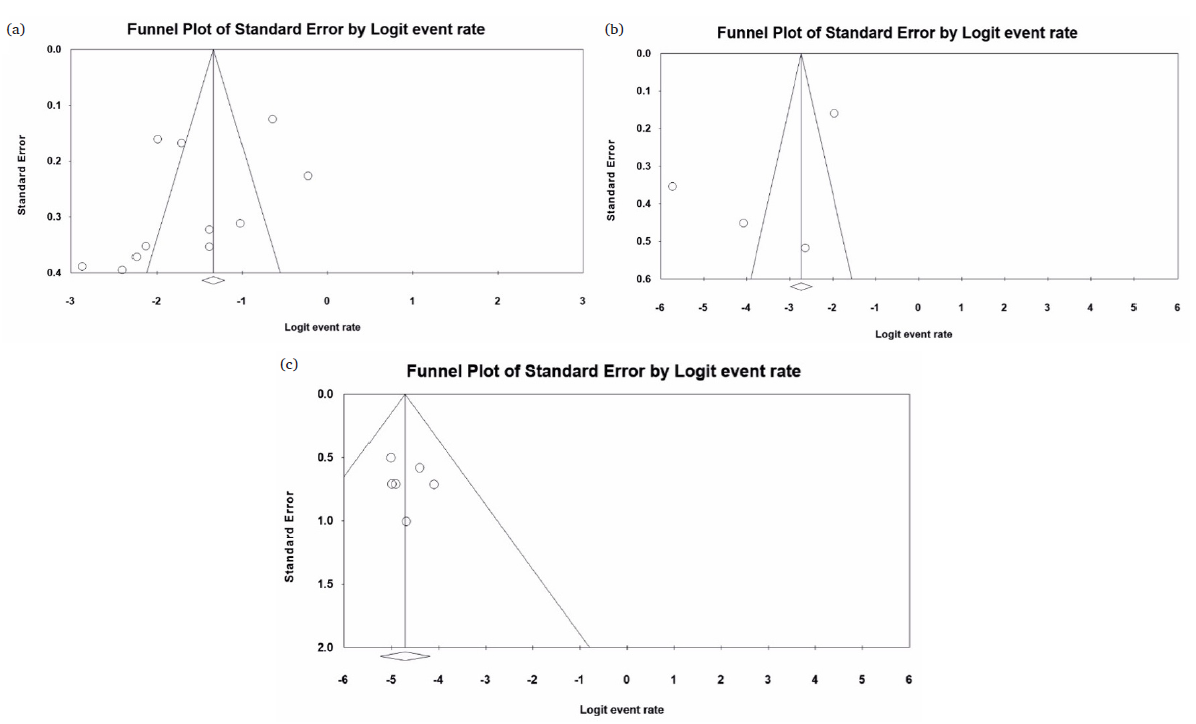
- Funnel plots assessing publication bias in the included studies. The publication bias for the prevalence of (a) suicidal ideation, (b) suicide attempts, and (c) suicide death rates in SLE patients was analyzed using CMA v3. The plots indicated no publication bias in the studies included in the global assessment of suicidal ideation, attempts, and mortality in SLE patients.
3.3 Heterogeneity analysis
The heterogeneity of the included studies was assessed using Cochrane Q and I-square (I2) statistics. Both suicidal ideation and suicide attempts demonstrated significant heterogeneity (Suicidal ideation: Cochrane Q=111.09, Pheterogeneity=0.00, I2=90.00; Suicidal attempts: Cochrane Q=103.60, Pheterogeneity=0.00, I2=97.10), leading to the application of a random-effects model for meta-analysis. Conversely, data on the prevalence of completed suicides exhibited homogeneity (Cochrane Q=1.62, Pheterogeneity=0.89, I2=0.00), supporting the use of a fixed-effects model for the analysis.
3.4 Prevalence of suicidal ideation
A total of 11 reports were found to be eligible for investigating the prevalence of suicidal ideation, comprising data from 1551 SLE patients. The prevalence of suicidal ideation ranges from 5.3%28 to 44%31. The combined prevalence of suicidal ideation revealed a worldwide frequency of 16.8% with a 95% confidence interval from 11% to 24.5% (Fig. 3a).
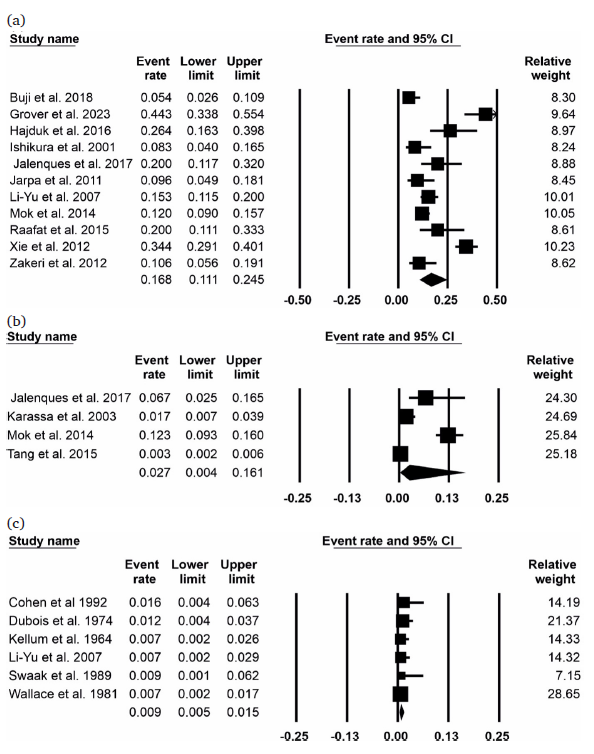
- Forest plots showing the prevalence of suicidal behaviors and death in SLE patients. The pooled event rate and 95% confidence interval were determined for (a) suicidal ideation, (b) attempts, and (c) suicide deaths, with meta-analysis conducted using CMA v3.
3.5 Frequency of suicidal attempts in SLE patients
The present analysis considered data from four studies involving 3196 patients with lupus to investigate the occurrence of suicide attempts. A meta-analysis conducted using a random-effects model estimated the overall prevalence of suicide attempts at 2.7%, with a 95% confidence interval ranging from 0.4% to 16.1% (as shown in Fig. 3b).
3.6 The Complete suicide rate in SLE patients
Six eligible reports on complete suicide data during the follow-up period were considered to evaluate the prevalence of complete suicide rate among 4,134 SLE patients. Using a fixed-effects model, the meta-analysis determined that the overall prevalence of completed suicides was 0.9%, with a 95% confidence interval of 0.5% to 1.5% (as shown in Fig. 3c).
3.7 Sensitivity analysis
Sensitivity analysis was conducted to evaluate the stability of the meta-analysis by systematic exclusion of one study at a time and comparison of outcomes to the original results. Significant deviations in the sensitivity analysis findings from primary meta-analysis could indicate weaker conclusions. However, as depicted in Fig. 4, the analyses for the prevalence of suicidal ideation, attempts, and completed suicides showed minimal variations, confirming the robustness of the results.
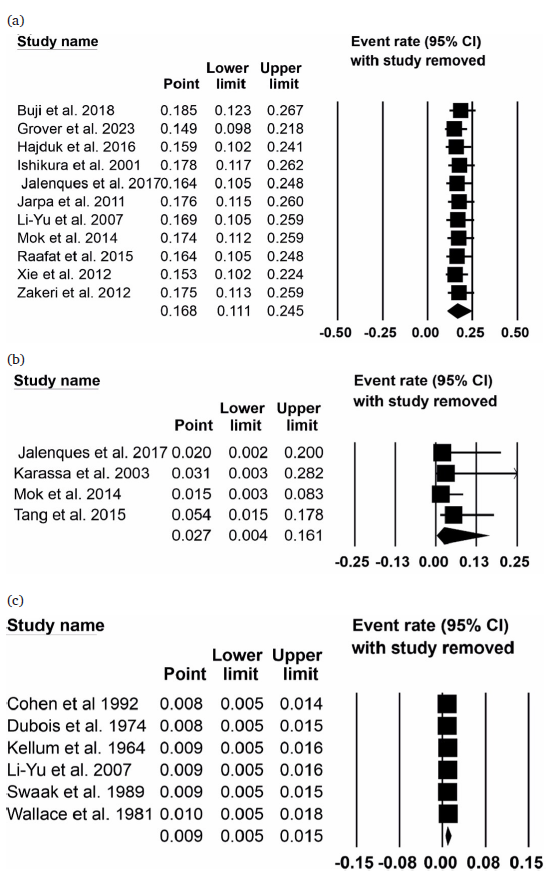
- Sensitivity analysis for suicidal behaviors and death prevalence in SLE patients. The analysis was conducted by sequentially excluding one study at a time and recalculating the meta-analysis. The results demonstrated the robustness of the findings for (a) suicidal ideation, (b) attempts, and (c) suicide death rates.
4. Discussion
The present study explored the worldwide prevalence of suicide ideation, attempts, and actual suicidal death in SLE patients using earlier published articles. It observed about 17% of SLE patients had suicidal ideation, 2.7% had a history of suicidal attempts, and 1% committed suicide during the follow-up period of the investigations. A previous cross-sectional study conducted across 17 countries in the general population found 9.2 percent suicidal ideation and 2.7 percent suicidal attempts (Nock et al., 2008). Although the general population’s rate of suicide attempts is comparable to that of SLE patients, suicidal ideation is more common in SLE patients. In addition, a recent report from the World Health Organization showed that 7,03,000 people worldwide attempted suicide in 2019 (WHO 2021), which represents 0.009 percent of the world’s population. According to the current analysis, SLE patients have a suicidal death rate that is approximately 100 times higher than the general population. To the best of our knowledge, this research is the first to examine the occurrence of three main types of suicidal behaviors in patients with SLE by utilizing a suitable statistical method.
The specific cause for the increased occurrence of suicidal thoughts in patients with SLE is not known. However, several factors have been attributed to the development of suicidal behaviors in patients. The neuropsychiatric side effects of glucocorticoid administration include psychosis, dementia, mood swings, anxiety, and insomnia (Kazi and Hoque 2021). As glucocorticoids are typically used to treat SLE (Luijten et al., 2013; Porta et al., 2020), patients may experience psychosis and mood disorders, which could increase the likelihood of suicidal thoughts. Additionally, a connection has been noted between suicidal thoughts in patients with SLE and the activity of the disease in the years leading up to it (Mok et al., 2014). Chronic inflammation may contribute to suicidal behavior through elevated pro-inflammatory cytokines and activation of the kynurenine pathway. Psychosocial stressors like unemployment and social isolation, along with disease-related factors such as organ damage and uncertainty about prognosis, further increase risk. In addition, suicidal behavior was more common in SLE patients who had depression, anxiety, unemployment, a history of psychiatric disorders, or significant life events in the previous months (Mok et al., 2014).
The current meta-analysis has several advantages over previous reports, including considering more reports with more significant patient numbers and considering three crucial parameters: suicidal ideation, attempts, and death during follow-up. An earlier meta-analysis published in 2018 included data on suicidal ideation from nine reports involving 1354 patients with SLE (Li et al., 2018). Although Parperis et al. (2022) considered all three important suicidal parameters, the authors presented their data in a systematic review format. They reported an average prevalence of suicidal ideation (15.7%) and suicidal death (2.3%). However, in the current meta-analysis, we observed a lower number of suicidal deaths (0.9%). The calculation of average prevalence has several drawbacks, and the results are not robust. By integrating findings from multiple reports, meta-analysis overcomes the limitations of individual studies (Curran and Hussong 2009). It provides a more comprehensive and robust assessment of the research question using an appropriate statistical approach (Curran and Hussong 2009). When observational studies merge various designs, methodologies, and characteristics of populations, it can lead to the introduction of errors and biases (Bencko and Chen 2014). Meta-analysis can mitigate those issues using a standardized data collection and analysis approach across multiple reports (Bencko and Chen 2014).
The heightened likelihood of suicidal thoughts among patients with SLE is a critical concern that healthcare professionals need to tackle. Methods to help SLE patients’ mental and physical health include routine screenings, easy access to counselling and therapy, and working with interdisciplinary teams (Hanly et al., 2010). By addressing the mental health aspects of SLE, healthcare providers can minimize the suicidal rate and help patients improve their overall well-being and quality of life.
While the present study successfully highlighted the global prevalence of suicidal thoughts, attempts, and completed suicides among individuals with SLE, it also has various limitations that need to be considered. To begin with, the amount of research included in this analysis was somewhat limited due to insufficient data. Second, due to the unavailability of information in the reports considered for the analysis, confounding factors for suicidal behavior in patients with SLE were not considered. Third, the criteria for diagnosing suicidal behavior varied between reports. Fourth, the data used to calculate the prevalence of suicidal ideation and attempts showed heterogeneity, which could be attributed to the adaptation of differential diagnosis criteria for scoring suicidal behaviors, as well as bias in patient selection.
5. Conclusions
The current investigation reveals that 17% of SLE patients experience suicidal ideation, 3% have attempted suicide, and 1% have completed suicide during treatment, highlighting the need for targeted interventions. Healthcare providers should conduct regular mental health assessments for all SLE patients using validated screening tools for suicidal ideation and depression in chronic illness populations. Collaborative care models involving rheumatologists, psychiatrists, and psychologists should be established, with clear referral pathways for at-risk patients. Psychoeducation on the increased risk of suicidal behaviors in SLE should be provided to patients and families. Evidence-based psychotherapies, such as cognitive-behavioral therapy, and pharmacological treatments for depression should be considered, with careful monitoring for interactions with SLE medications. Special attention should be given to patients with risk factors like active disease, unemployment, or a history of psychiatric disorders. Implementing these recommendations can help reduce suicidal behaviors and improve the mental health and quality of life for SLE patients.
Acknowledgements
The authors would like to acknowledge their respective institutes for providing the necessary support for the work. The authors gratefully acknowledge the funding of the Deanship of Graduate Studies and Scientific Research, Jazan University, Saudi Arabia, through project number: RG24-L06.
CRediT authorship contribution statement
Darin Mansor Mathkor: Literature search, data analysis, Shovit Ranjan: Literature search, data analysis, Tapan Kumar Singh Nayak: Literature search, data analysis, Aditya K Panda: Concept, design, manuscript editing, manuscript review, Ashjan Saeed Babegi: Data analysis, manuscript preparation, Raju K. Mandal: Data analysis, manuscript preparation, Shafiul Haque: Concept, design, manuscript editing, manuscript review.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Declaration of Generative AI and AI-assisted technologies in the writing process
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary data
Supplementary data to this article can be found online at https://dx.doi.org/10.25259/JKSUS_47_2024
References
- Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public Health. 2018;15:1425. https://doi.org/10.3390/ijerph15071425
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiological data and cancer risk assessment: Cessation LAG and lingering effect concepts. Cent. Eur. J. Public Health. 2014;22:197-200. https://doi.org/10.21101/cejph.a3940
- [CrossRef] [PubMed] [Google Scholar]
- Suicidal ideation in systemic lupus erythematosus: NR2A gene polymorphism, clinical and psychosocial factors. Lupus. 2018;27:744-752. https://doi.org/10.1177/0961203317742711
- [CrossRef] [PubMed] [Google Scholar]
- Mortality in systemic lupus erythematosus: Active disease is the most important factor. Australian and New Zealand Journal of Medicine. 1992;22:5-8. https://doi.org/10.1111/j.1445-5994.1992.tb01700.x
- [CrossRef] [PubMed] [Google Scholar]
- Integrative data analysis: The simultaneous analysis of multiple data sets. Psychol. Methods. 2009;14:81-100. https://doi.org/10.1037/a0015914
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Depression, anxiety, and quality of life in patients with systemic lupus erythematosus. Reumatologia. 2023;61:368-374. https://doi.org/10.5114/reum/168396
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Duration and death in systemic lupus erythematosus. JAMA. 1974;227:1399. https://doi.org/10.1001/jama.1974.03230250023021
- [CrossRef] [PubMed] [Google Scholar]
- Pain and systemic lupus erythematosus. Reumatismo. 2014;66:33-38. https://doi.org/10.4081/reumatismo.2014.762
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric comorbidities in patients suffering from systemic lupus erythematosus admitted to a tertiary care hospital in northern India. Lupus. 2023;32:1008-1018. https://doi.org/10.1177/09612033231177737
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and correlates of suicidal thoughts in patients with neuropsychiatric lupus. Lupus. 2016;25:185-192. https://doi.org/10.1177/0961203315603136
- [CrossRef] [PubMed] [Google Scholar]
- Prospective analysis of neuropsychiatric events in an international disease inception cohort of patients with systemic lupus erythematosus. Ann. Rheum. Dis.. 2010;69:529-535. https://doi.org/10.1136/ard.2008.106351
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Anxiety and depression and associated risk factors among outpatients with systemic lupus erythematosus: Eastern province, Saudi arabia. Clin Pract. 2024;14:486-497. https://doi.org/10.3390/clinpract14020037
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors associated with anxiety, depression and suicide ideation in female outpatients with SLE in Japan. Clin. Rheumatol.. 2001;20:394-400. https://doi.org/10.1007/s100670170002
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of personality disorders in skin-restricted lupus patients. Acta Derm. Venereol.. 2017;97:941-946. https://doi.org/10.2340/00015555-2691
- [CrossRef] [PubMed] [Google Scholar]
- Common mental disorders and psychological distress in systemic lupus erythematosus are not associated with disease activity. Lupus. 2011;20:58-66. https://doi.org/10.1177/0961203310381773
- [CrossRef] [PubMed] [Google Scholar]
- Adverse consequences of glucocorticoid medication: Psychological, cognitive, and behavioral effects. Am. J. Psychiatry. 2014;171:1045-1051. https://doi.org/10.1176/appi.ajp.2014.13091264
- [CrossRef] [PubMed] [Google Scholar]
- Suicide attempts in patients with systemic lupus erythematosus. Ann. Rheum. Dis.. 2003;62:58-60. https://doi.org/10.1136/ard.62.1.58
- [CrossRef] [PubMed] [Google Scholar]
- Fatigue in systemic lupus erythematosus: An update on its impact, determinants and therapeutic management. J Clin Med. 2021;10:3996. https://doi.org/10.3390/jcm10173996
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute psychosis following corticosteroid administration. Cureus. 2021;13:e18093. https://doi.org/10.7759/cureus.18093
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Systemic lupus erythematosus. Arch. Intern. Med.. 1964;113:200. https://doi.org/10.1001/archinte.1964.00280080036008
- [CrossRef] [PubMed] [Google Scholar]
- The socioeconomic burden of SLE. Nat. Rev. Rheumatol.. 2009;5:400-404. https://doi.org/10.1038/nrrheum.2009.106
- [CrossRef] [PubMed] [Google Scholar]
- A survey of psychosocial attributes of filipino patients with systemic lupus erythematosus. APLAR Journal of Rheumatology. 2007;10:107-111. https://doi.org/10.1111/j.1479-8077.2007.00269.x
- [CrossRef] [Google Scholar]
- The prevalence of suicidal ideation and suicide attempt in patients with rheumatic diseases: A systematic review and meta-analysis. Psychology 2018:Health & Medicine 23, 1025-1036. https://doi.org/10.1080/13548506.2018.1476724
- [CrossRef] [PubMed] [Google Scholar]
- The use of glucocorticoids in systemic lupus erythematosus After 60 years still more an art than science. Autoimmun. Rev.. 2013;12:617-628. https://doi.org/10.1016/j.autrev.2012.12.001
- [CrossRef] [PubMed] [Google Scholar]
- Suicidal ideation in patients with systemic lupus erythematosus: Incidence and risk factors. Rheumatology (Oxford). 2014;53:714-721. https://doi.org/10.1093/rheumatology/ket404
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and metric of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. Elsevier: Seminars in arthritis and rheumatism; 2020.
- Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60-63. https://doi.org/10.1136/bmjebm-2017-110853
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry. 2008;192:98-105. https://doi.org/10.1192/bjp.bp.107.040113
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Depression and systemic lupus erythematosus: A systematic review. Lupus. 2013;22:409-416. https://doi.org/10.1177/0961203313477227
- [CrossRef] [PubMed] [Google Scholar]
- Maintaining ethics, integrity, and accountability: Best practices for reporting a meta-analysis. Account. Res. 2024:1-3. https://doi.org/10.1080/08989621.2024.2334722
- [CrossRef] [Google Scholar]
- Suicidal behavior in patients with systematic lupus erythematosus: Systematic literature review and genetic linkage disequilibrium analysis. Semin. Arthritis Rheum.. 2022;54:151997. https://doi.org/10.1016/j.semarthrit.2022.151997
- [CrossRef] [PubMed] [Google Scholar]
- Glucocorticoids in systemic lupus erythematosus Ten questions and some issues. J Clin Med. 2020;9:2709. https://doi.org/10.3390/jcm9092709
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Major depression and disease activity among systemic lupus erythematosus egyptian females. The Egyptian Rheumatologist. 2015;37:S1-S6. https://doi.org/10.1016/j.ejr.2015.09.007
- [CrossRef] [Google Scholar]
- Seventy years after hench’s nobel prize: Revisiting the use of glucocorticoids in systemic lupus erythematosus. Lupus. 2020;29:1155-1167. https://doi.org/10.1177/0961203320930099
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychiatric systemic lupus erythematosus: A 2021 update on diagnosis, management, and current challenges. Cureus. 2021;13:e17969. https://doi.org/10.7759/cureus.17969
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Self-efficacy and pain catastrophizing in systemic lupus erythematosus: Relationship to pain, stiffness, fatigue, and psychological distress. Arthritis Care Res (Hoboken). 2012;64:1334-1340. https://doi.org/10.1002/acr.21686
- [CrossRef] [PubMed] [Google Scholar]
- Systemic lupus erythematosus I outcome and survival: Dutch experience with 110 patients studied prospectively. Ann. Rheum. Dis.. 1989;48:447-454. https://doi.org/10.1136/ard.48.6.447
- [CrossRef] [PubMed] [Google Scholar]
- Suicide attempts in patients with systemic lupus erythematosus: A single-center experience and literature review. Psychosomatics. 2015;56:190-195. https://doi.org/10.1016/j.psym.2014.05.020
- [CrossRef] [PubMed] [Google Scholar]
- Systemic lupus erythematosus-Survival patterns. JAMA. 1981;245:934. https://doi.org/10.1001/jama.1981.03310340024021
- [CrossRef] [PubMed] [Google Scholar]
- The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- Suicide worldwide in 2019: global health estimates.
- Prevalence and correlates of suicidal ideation in SLE inpatients: Chinese experience. Rheumatol. Int.. 2012;32:2707-2714. https://doi.org/10.1007/s00296-011-2043-3
- [CrossRef] [PubMed] [Google Scholar]
- Prescription patterns of psychotropics in patients receiving synthetic glucocorticoids. Acta Psychiatr. Scand.. 2020;142:242-248. https://doi.org/10.1111/acps.13217
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of depression and depressive symptoms in patients with systemic lupus erythematosus: Iranian experience. Rheumatol. Int.. 2012;32:1179-1187. https://doi.org/10.1007/s00296-010-1791-9
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of depression and anxiety in systemic lupus erythematosus: A systematic review and meta-analysis. BMC Psychiatry. 2017;17 https://doi.org/10.1186/s12888-017-1234-1
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







