Translate this page into:
Comparing the efficacy of blind vs. ultrasound-guided injections in Lateral Epicondylitis: A prospective analysis
⁎Corresponding author. javidviqar@gmail.com (Sheikh Viqar Javid)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lateral epicondylitis is a relatively common non-traumatic elbow disorder. It is a painful musculoskeletal condition that usually follows forceful repetitive pronation and supination. The aim of this study was to evaluate the advantages of ultrasound-guided injection in patients of Lateral Epicondylitis in comparison to non-image-guided blind injections. This comparative observational study was conducted on sixty patients who had clinical diagnosis of Lateral Epicondylitis. They were divided into two groups of thirty each (randomization done on odd even manner), one group underwent US-guided injections and the other group underwent the blind procedure by a specialist. Pain relief using the Visual Analog Scale (VAS) {score of 0–10} was recorded before the procedure, immediately after the procedure, one-week post-procedure, and six weeks post-procedure. Demographic characteristics, chief complaints, duration of symptoms, previous treatment taken, and complications post-procedure were gathered and compared between the two groups. All patients in both groups finished the period of study. Significant improvement in pain score and tenderness was found in both groups immediately after the injection, one-week post-procedure, and after six weeks post-procedure when compared to the baseline value (p value < 0.05). The US-guided group showed a better reduction in VAS scores immediately after the procedure and one-week post-procedure as compared to patients who were given blind injections, however no statistical difference was found at six weeks follow up. This study shows that US-guided injection relatively improves elbow pain and functional activities early and more effectively than blind/non-image-guided injections, although such results fade as time passes by.
Keywords
Tennis Elbow
Visual Analog Scale
Lateral Epicondylitis
US guided injections
1 Introduction
Lateral Epicondylitis (LE) is a common non-traumatic elbow disorder that was first described by Runge in 1873. Since about half of tennis players, especially beginners learning the one-handed backhand, suffer from LE, it is also known as tennis elbow (Lenoir et al., 2019). Most musculoskeletal health care professionals will diagnose “tennis elbow” or, more accurately, lateral epicondylalgia as the provisional diagnosis when pain over the lateral humeral epicondyle occurs during activities requiring the hand to grip or manipulate an object, such as those required when lifting a tea cup or housework (Szeinuk et al., 2000). It is not only confined to tennis players but is a commonly diagnosed musculoskeletal condition of the upper extremity (Vicenzino, 2003) with an incidence of 1.3–3.0 % in the general population (Mizrahi, 2020). It usually affects 40–50-year-olds, equally in both men and women (Linaker et al., 1999). Lateral Epicondylitis presents with pain that is localized to the lateral region of the elbow, that is, the lateral epicondyle of the Humerus (Whaley and Baker, 2004). It can be intermittent, mild to continuous severe pain that may result in sleep disturb ance. Pain is typically exacerbated by wrist and hand movements and may radiate to the forearm impairing hand grip. As the disease progresses a bony prominence can be distinguished over the lateral epicondyle (Sconfienza et al., 2012). Sometimes atrophy of the skin and muscle is observed in patients with severe and chronic disease (Viola, 1998). Other symptoms and signs seen clinically are a burning sensation at the joint, poor or painful range of motion (ROM), stiffness, impaired hand grip, difficulty in lifting heavy objects, opening a jar, etc. In clinical tennis elbow situations, the existence or persistence of symptoms in some people may be associated with the sharp-edged bony excrescences. (Edelson et al., 2001). Lateral Epicondylitis, commonly known as tennis elbow, is typically diagnosed through a combination of patient history and clinical examination. To obtain a precise diagnosis and assess the severity of the condition, specific clinical tests can be employed. The most widely accepted tests for this purpose include Cozen's Test, as described by Karanasios et al. (2021). Mill's Test, as discussed by Saroja et al. (2014). Maudsley's Test, outlined by Pienimäki et al. (2002). In most instances, the need for imaging studies is not essential, but they may be used to ascertain the extent of tissue damage and rule out other potential causes of symptoms. Specialized X-ray techniques, such as coronal reconstructions using computed axial tomography (CT), have revealed that a significant proportion (around 60 %) of patients experiencing tennis elbow symptoms exhibit bone abnormalities, as reported by Levin et al. (2005).
Tennis elbow is managed by a variety of treatment modalities, the aim is to achieve pain control, improve grip strength, preserve the range of motion (ROM), restore normal function, and prevent further complications. Most cases only need simple analgesics as treatment because it is typically self-limiting. Various treatments are available for patients who have severe or enduring symptoms. Conservative treatment options for this condition encompass a range of therapies such as acupuncture, topical nitrates, elbow straps, physiotherapy, eccentric exercises, shock-wave therapy, laser therapy, shock-wave treatment, corticosteroid injections, botulinum toxin, autologous blood, and platelet-rich plasma injections. In situations where these methods fail to yield results, various surgical techniques, including both open and arthroscopic procedures, have been documented as potential interventions (Ahmad et al., 2013; Lin et al., 2012). First-line therapy is non-operative and includes patient education, pain control with the help of painkillers (NSAIDs), ice application, immobolization of the upper limb, and physiotherapy (Ma and Wang, 2020). Among the many treatment modalities, ultrasound-guided administration of injection in patients with tennis elbow is a technique to relieve the pain by administering a fixed dose of a medication usually a corticosteroid under ultrasound guidance rather than blindly. It prevents accidental injuries to nerves and vessels around the elbow that are common with blind methods. Ultrasound (US) imaging has established itself as a useful technique for making a precise diagnosis and as a practical tool for directing therapies. (Mezian et al., 2021). A transducer is placed over the targeted area and an anatomical landmark is identified on the monitor, after confirmation a needle is inserted to inject the appropriate drug (Narouze and Peng, 2010). It potentially increases clinical effectiveness by ensuring the delivery of injection at the desired anatomical landmark. (McAuliffe et al., 2016).
Fewer studies have been carried out to make a comparison between ultrasound guided injection versus non-image guided injection in tennis elbow management. So, we undertook a comparative observational study to determine the benefits of ultrasound-guided injection versus non-image-guided blind injections in patients with LE. The purpose and goals of this study were to assess the benefits of using ultrasound guidance for injections in patients with lateral epicondylitis compared to the conventional method of blindly administering injections without image guidance.
2 Materials and methods
This observational comparative study took place at the Department of Radiology and Imaging at the Sher-I-Kashmir Institute of Medical Sciences, in partnership with the Department of Orthopaedics at SKIMS Medical College Bemina, Srinagar. It was a prospective study that received approval from the institutional ethical committee under the reference number SIMS 131/IEC-SKIMS/2022–283. A total of 60 patients were included in our study. The patients were assigned into two groups in an odd and even manner. Out of these 30 were subjected to USG- guided injection (Group I) and 30 to blind palpation guided injection (Group II) in odd and even fashion (as shown in Figs. 1 and 2). The study was carried out using High Resolution linear probe (12 Hz), Logic p5 GE premium ultrasound machine (GE healthcare, Germany). The patients were assigned a number on a VAS ranging from 0 to 10 by a pain specialist with 0 being no symptoms and 10 being the most severe symptoms (Heller et al., 2016). The patients with a score equal to or greater than 4 were subjected to local corticosteroid injection either by blind method or under ultrasound guidance in odd and even manner. They were then followed up regularly to check for improvement in symptoms using the Visual Analogue Scale (VAS). The materials used were:
-
High frequency 12 MHz Linear Array Transducer.
-
Local Anesthesia.
-
Corticosteroid (2–3 ml of 40 mg/ml Methylprednisolone).
-
Local Disinfectants.
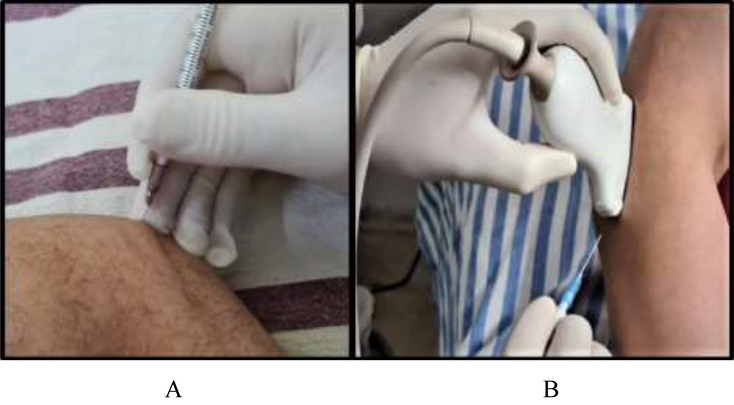
- A. blind injection is carried out B. guided injection is being done.
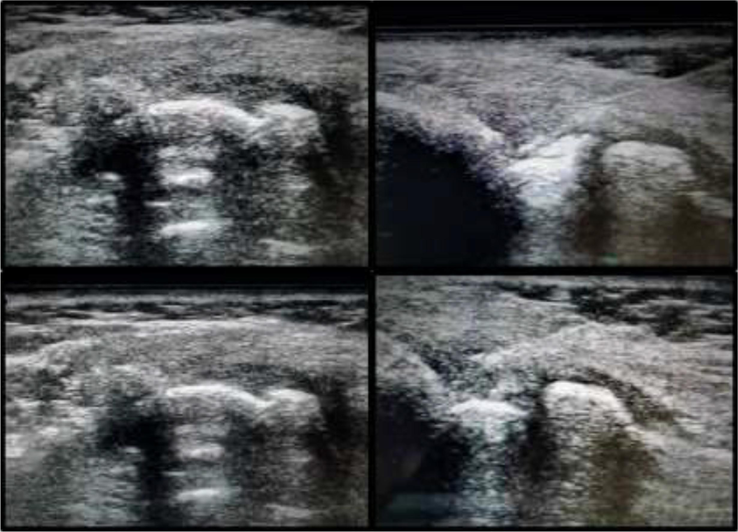
- Depicting US-images of patient treated with local steroid injection: The images on the left side are prior to the injection while as those on the right side are while carrying out the procedure (NEEDLE CAN BE SEEN IN RIGHT IMAGES).
Only the patients with symptomatic LE who had not responded to conservative treatment, irrespective of age and sex, and who gave informed consent were included in this study. Patients with inflammatory diseases, neck or shoulder pain, Local Anaesthetic (LA) allergy, local infection, undergoing any other modality of treatment were excluded. After the treatment was given the data was collected and statistical testing was con-ducted using the statistical package for SPSS 2.0. Continuous variables were presented as mean ± SD and categorical variables as absolute numbers and percentages. For statistical significance, the p-value of < 0.05 was considered significant.
3 Results
The study involved 60 patients of which 43 were males and 17 females of which Group I included 23 males and 7 females whereas Group II had 20 males and 10 females. Most of the patients were in the age group of 41–50 years (38.3 %) followed by 21–30 years (16.7 %) and 51–60 years (13.3 %). The mean age was 40.86 ± 9.92 years. The mean age of Group I patients was 41.8 ± 9.92 years whereas that of Group II was 39.3 ± 8.62 years. (Table 1, Table 2 and Fig. 3). In our study, most of the subjects were from the urban area with Group I including 76.6 % urban subjects and Group II had 70 % of the subjects from the urban area. The remaining were from the rural area, that is, 23.3 % and 30.0 % in Groups I and II respectively. Furthermore, in our study most of the patients in Group I and II had involvement of the right elbow, that is, 70.0 % and 73.33 % respectively. Whereas only 30 0.0 % in Group I and 26.6 % in Group II had involvement of the left side elbow (Fig. 4 and Table 3).
Age (In years)
Number
Percentage
21–30
10
16.7
31–40
19
31.7
41–50
23
38.3
51–60
8
13.3
Total
60
100
Gender
USG Guided
(Group 1)Non-USG Guided (Group 2)
Male
23 (76.66 %)
20 (66.66 %)
Female
7 (23.33 %)
10 (33.33 %)
Total
30(100 %)
30 (100 %)
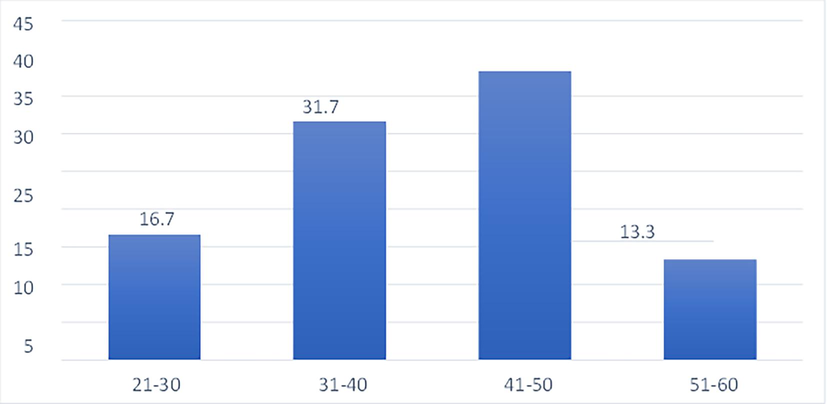
Age distribution.
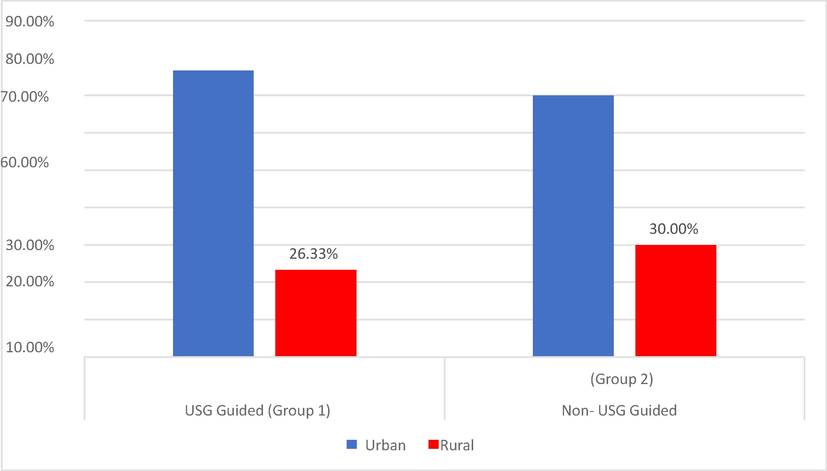
Depicting distribution of patients, being of either urban or rural locality.
Side Involved
USG Guided
(Group 1)Non-USG Guided
(Group 2)
Right
21(70 %)
22(73.33 %)
Left
9(30 %)
8(26.66 %)
Total
30(100 %)
30(100 %)
4 Discussion
The elbow joint is a non-weight-bearing, mobile joint that is affected by various pathological conditions. The pathological conditions may affect medial aspect of elbow resultant medial epicondylitis or lateral aspect of elbow with resultant lateral epicondylitis. Furthermore it has been found that a number of other pathological conditions can affect this joint including biceps tendinosis/ tear, triceps tendinosis/ tear, olecranon bursitis, snapping triceps syndrome, cubital tunnel syndrome etc. (Panta et al., 2023). Lateral Epicondylitis is a degenerative condition of the elbow joint. It causes pain around the elbow and is generally caused by repetitive use of forearm extensor muscles. Tennis elbow can be brought on by any activity that requires frequent wrist twisting. This includes playing racquet sports like tennis or golf, swimming, or using a screwdriver, hammer, or computer. A muscle's tendon is where it connects to the bone. The outer elbow bone is where the forearm muscles are attached. The extensor carpi radialis brevis (ECRB) muscle in the forearm is frequently the cause of tennis elbow Microtears in the ECRB muscular tendon at the location where it joins to the outside of the elbow result from repetitive tension, which weakens the muscle. Pain and inflammation are caused by these tears. Tennis elbow is thought to be caused by a variety of factors, including playing experience, skill level, and racket type, according to clinical investigations. Inexperienced players are more likely to mishit the ball and have poor stroke mechanics, which puts extra mechanical stress on the elbow joint (Khan, 2014; Lin et al., 2012). Patients with epicondylitis manifest point tenderness along the lateral epicondyle, occasional swelling on the out-side of the elbow, pain & difficulty in lifting objects and during joint movements (Nag and Nag, 2019). Injection therapy for tennis elbow is a common modality of treatment. During injection administration in the lateral elbow, the exact location of administration has a great role in the clinical outcome. According to a study, tennis elbow treatment can be guided by ultrasound (US) imaging, which is a useful way for determining a precise diagnosis. Although corticosteroids were historically the most used medication, recent research on their harmful long-term effects suggests that their use may be declining. The development of innovative medicines, such as platelet-rich plasma (PRP), autologous blood (AB), botulinum toxin, glycosaminoglycan polysulphate, sodium hyaluronic acid, or prolotherapy, continues to raise interest in injectable therapy, though. (Evans et al., 2018). The use of ultrasound to perform elbow examinations and interventions has gained prevalence due to the absence of exposure to radiation, accessibility, reduced cost, and ease of use and handling as compared to other radiological modalities. To prevent injecting corticosteroids directly into tendon material or subcutaneous tissue, which could result in subcutaneous fatty atrophy and skin depigmentation, ultrasound can be used to guide the needle during injection. For the treatment of tendon or ligament anomalies in the elbow, ultrasound-guided therapeutic injections have been utilized extensively, particularly in patients who have failed to respond to more conventional therapies such rest, nonsteroidal anti-inflammatory medications, splinting, and physical therapy. At the location where the common extensor tendons insert, tendinopathy or enthesopathy are frequent findings in lateral epicondylitis. The effectiveness of corticosteroid peritendinous injection in reducing lateral epicondylitis pain temporarily has been demonstrated (Gutierrez et al., 2016).
Various research findings supported that ultrasound-guided injections are more accurate strategies for joint, tendon, and soft tissue administrations The use of US-guided injections (USGI) ensures that the needle is inserted correctly, increasing effectiveness while minimizing side effects. To further increase safety during the procedures, US guided injection may prevent direct contact with the needle, nerves, tendons, and blood vessels. Various studies have shown that US guided injection has superior clinical outcomes and is more accurate. But the majority of them have evaluated effectiveness in intra-articular targets. As with the tenosynovitis that is usually present in chronic arthritis, there are currently no randomized studies examining the clinical result at the peri-articular level (Connell et al., 2006). Thus, the present study was done to determine the benefits of ultrasound-guided injection in comparison to non-image-guided blind injections in patients of chronic lateral epicondylitis.
The current study's findings indicate that in Group I, the Visual Analog Scale (VAS) pain score decreased from an initial value of 6.36 ± 1.15 to 2.66 ± 0.92 right after the injection, and further dropped to 2.03 ± 1.21 one week after the procedure. At the six-week mark post-procedure, the VAS score decreased even more to 1.4 ± 1.22. In Group II, the VAS pain score decreased from the baseline score of 6.46 ± 1.30 to 2.96 ± 1.13 immediately following the injection, and to 2.46 ± 1.19 one week later. At the six-week post-procedure point, the VAS score was 1.86 ± 1.04. There was no statistically significant difference in VAS scores between the two groups before the procedure. However, both groups showed a statistically significant reduction in VAS scores immediately after the injection and at the six-week follow-up when compared to their initial baseline values (P < 0.05). Additionally, six weeks after the injection, the VAS scores between the two groups were statistically similar. Group I exhibited significant improvement right after the injection when compared to Group II. Both groups showed a decrease in tenderness immediately after the procedure, as well as at one week and six weeks post-procedure. Our results agree with a study conducted by Connell et al. (2006) that found a significant decrease in VAS scores after sonographically guided injection in patients with tennis elbow (Connell et al., 2006). George et al. (2018) also stated that the pain score in the interventional group was significantly decreased after the administration of injection (Pang et al., 2018). Another study conducted by Saglam et al. (2022) reported that in palpation guided group baseline VAS score was 7.2 ± 1.8, 6.3 ± 0.8 in 1st month after administration, 2.8 ± 1.9 after 3rd month of injection and 2.3 ± 0.7 after 6th month and in ultrasound-guided group VAS score was 7.3 ± 1.5 at baseline, 6.0 ± 0.8 at 1st month after administration, 2.1 ± 1.25 after 3rd month of injection and 1.9 ± 1.2 after 6th month. Moreover, the study noted that there was no statistically significant disparity in VAS scores between the two groups prior to the procedure. Furthermore, there was a substantial decrease in VAS scores in both groups immediately after the injection and at the six-week follow-up, and this reduction was deemed statistically significant (p < 0.001) in comparison to the baseline values in both groups (Sağlam and Alişar, 2023).
Regarding post-procedure complications, in Group I, stiffness was reported in 01 (3.33 %) patients, and severe pain in the extensor region was also reported in 01 (3.33 %) patients. In Group II, 02 (6.66 %) patients reported stiffness whereas hematoma, severe pain in the extensor region, and vascular puncture were reported in 01 (3.33 %) patients each. The results of our study align with those of Gulabi et al. (2017), who conducted a single-blinded, randomized controlled clinical trial to assess the clinical therapeutic outcomes of blind and ultrasound-guided corticosteroid injection therapy in lateral epicondylitis. They reported that there were no systemic or local complications observed during the treatment (Gulabi et al., 2017). However, our study had certain limitations, including a relatively short follow-up duration and a smaller sample size. Additionally, another potential limitation was the variations in injection techniques between blind and ultrasound-guided procedures and differences in operator expertise.
5 Conclusions
The study indicates that USG-guided injections offer greater precision and effectiveness in reducing elbow discomfort and improving functional activities when compared to non-image-guided injections. These findings were observed during a six-week follow-up period, during which the improvements in pain reduction and functional out-comes were sustained without any significant problems. However, to thoroughly analyze the long-term effects of pain alleviation and functional outcomes in lateral epicondylitis (also known as tennis elbow), further research is needed. Specifically, long-er-term follow-up studies involving a larger population of patients would provide more comprehensive and reliable data. Such studies would enable researchers to assess the durability of the observed improvements and evaluate the treatment's effectiveness over an extended period. By conducting studies with a larger sample size, researchers can increase the statistical power of their analysis, enhancing the generalizability and reliability of the results. Additionally, longer follow-up periods allow for a better understanding of the treatment's long-term effects and potential complications that may arise over time. Overall, while the initial findings of the study suggest that USG-guided injections are beneficial for reducing elbow discomfort and improving functional activities in lateral epicondylitis, it is important to conduct more extensive research with a larger patient population and longer follow-up durations to obtain a more conclusive understanding of the treatment's long-term effects. Future aspects of the study can be using larger sample size and comparing different agents using US-guidance for treatment of lateral epicondylitis.
Institutional review board statement
This study was conducted in accordance with the Declaration of Helsinki and approved by Institutional Ethical Committee ((SIMS 131/IEC-SKIMS/2022–283).
Data availability statement
The data are available upon request from the corresponding author.
Acknowledgement
This work was funded by Researchers Supporting Project Number (RSP2023R26), King Saud University, Riyadh, Saudi Arabia.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Lateral epicondylitis: a review of pathology and management. Bone Joint J.. 2013;95(9):1158-1164.
- [Google Scholar]
- Ultrasound-guided autologous blood injection for tennis elbow. Skeletal Radiol.. 2006;35:371-377.
- [Google Scholar]
- Bony changes at the lateral epicondyle of possible significance in tennis elbow syndrome. J. Shoulder Elbow Surg.. 2001;10(2):158-163.
- [Google Scholar]
- The spread of Injectate after ultrasound-guided lateral elbow injection–a cadaveric study. J. Experimental Orthopaedics. 2018;5:1-8.
- [Google Scholar]
- USG-guided injection of corticosteroid for lateral epicondylitis does not improve clinical outcomes: a prospective randomised study. Arch. Orthop. Trauma Surg.. 2017;137:601-606.
- [Google Scholar]
- Short-term efficacy to conventional blind injection versus ultrasound-guided injection of local corticosteroids in tenosynovitis in patients with inflammatory chronic arthritis: a randomized comparative study. Joint Bone Spine. 2016;83(2):161-166.
- [Google Scholar]
- How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand. J. Pain. 2016;13(1):67-75.
- [Google Scholar]
- Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)–A systematic review. J. Hand Ther. 2021
- [Google Scholar]
- Effectiveness of autologous blood injection in patients with lateral Epicondylitis (Tennis Elbow) Ophthalmology. 2014;12(2):159.
- [Google Scholar]
- Management of lateral epicondylitis. Orthop. Traumatol. Surg. Res.. 2019;105(8):S241-S246.
- [Google Scholar]
- Sonographic detection of lateral epicondylitis of the elbow. Radiology. 2005;237:230-234.
- [Google Scholar]
- Application of ultrasound and ultrasound-guided intervention for evaluating elbow joint pathologies. J. Med. Ultrasound. 2012;20(2):87-95.
- [Google Scholar]
- Frequency and impact of regional musculoskeletal disorders. Best Pract. Res. Clin. Rheumatol.. 1999;13(2):197-215.
- [Google Scholar]
- Management of lateral epicondylitis: a narrative literature review. Pain Res. Manage. 2020
- [Google Scholar]
- Evidence for accuracy and effectiveness of musculoskeletal ultrasound-guided compared with landmark-guided procedures. Curr. Phys. Med. Rehabil. Rep.. 2016;4:5-11.
- [Google Scholar]
- Ultrasound-guided procedures in common tendinopathies at the elbow: from Image to Needle. Appl. Sci.. 2021;11(8):3431.
- [Google Scholar]
- Neuro-mechanical aspects of playing-related mobility disorders in orchestra violinists and upper strings players: a review. Eur. J. Transl. Myol.. 2020;30(3)
- [Google Scholar]
- Musculoskeletal disorders: Office menace. Office Build.: Health Saf. Environ. 2019:105-126.
- [Google Scholar]
- Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures: part ii: axial structures. Reg. Anesth. Pain Med.. 2010;35(4):386-396.
- [Google Scholar]
- Baicalin downregulates RLRs signaling pathway to control influenza A virus infection and improve the prognosis. Evidence-Based Complement. Alternat. Med. 2018
- [Google Scholar]
- Calcium pyrophosphate dihydrate deposition disease of elbow with ulnar nerve neuropathy: a case report. J. Chitwan Medical College. 2023;13(1):102-104.
- [Google Scholar]
- Associations between pain, grip strength, and manual tests in the treatment evaluation of chronic tennis elbow. Clin. J. Pain. 2002;18(3):164-170.
- [Google Scholar]
- Ultrasound-guided versus palpation-guided platelet-rich plasma injection for the treatment of chronic lateral epicondylitis: a prospective, randomized study. Arch. Rheumatol.. 2023;38(1):67.
- [Google Scholar]
- Diagnostic accuracy of provocative tests in lateral epicondylitis. Int. J. Physiother. Res.. 2014;2(6):815-823.
- [Google Scholar]
- Sconfienza L.M., Serafini G., Silvestri E., eds. Ultrasound-guided musculoskeletal procedures: the upper Limb. Springer Science & Business Media; 2012.
- Lateral epicondylalgia: a musculoskeletal physiotherapy perspective. Man. Ther.. 2003;8(2):66-79.
- [Google Scholar]
- A critical review of the current conservative therapies for tennis elbow (lateral epicondylitis) Aust. Chiropractic Osteopathy. 1998;7(2):53.
- [Google Scholar]
Appendix A
Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jksus.2023.103026.
Appendix A
Supplementary material
The following are the Supplementary data to this article:







