Translate this page into:
Acupuncture in the treatment of stable chronic obstructive pulmonary disease: A systematic review of randomised controlled trials
⁎Correspondence author. Department of Traditional Chinese Medicine, Chengdu Fifth People’s Hospital, Chengdu, Sichuan, CN 611130, China. xxzaihuaxi@163.com (Yan Wang)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Objective
To systematically evaluate the clinical efficacy and safety of acupuncture in the treatment of chronic obstructive pulmonary disease (COPD).
Methods
Randomised controlled trials (RCTs) of acupuncture and/or transcutaneous electrical nerve stimulation over acupoints (acu-TENS) in the treatment of the stable COPD were searched in PubMed, Embase, The Cochrane Library, WanFang Data, VIP, CNKI and CBM databases from the respective inception to January 2019. Literature screening and data extraction were independently performed by two researchers and methodological quality was assessed using the Cochrane Collaboration Risk of Bias Tool. Outcome measures included treatment efficiency, quality of life, lung function, activity tolerance and adverse events were evaluated.
Results
Eleven RCTs involving 709 patients were included. The results showed that the treatments of COPD, acupuncture and/or acu-TENS could improve the treatment efficiency compared with the control group [RR = 1.11, 95%CI (1.02 to 1.21), P = 0.02], improve the quality of life [MD = −3.66, 95%CI (−5.56 to −1.76), P = 0.0002], increased percentage of forced expiratory volume in 1 s (FEV1%) [MD = 8.75, 95%CI (0.98 to 16.51), P = 0.03], increased predicted forced vital capacity (FVC%) value [MD = 7.93, 95%CI (1.83 to 14.03), P = 0.01], increased FVC(L) [MD = 0.16, 95%CI (0.01 to 0.30), P = 0.04] and decreased Borg score [MD = -3.00, 95%CI (-3.99 to −2.01), P = 0.00001]. Only 3 cases reported mild contusion and pain.
Conclusions
Our systematic review shows that the combination of acupuncture with medications and/or rehabilitation exercise may increase efficacy in stable COPD treatment by alleviating the clinical symptoms and improving the quality of life.
Keywords
Acupuncture
Chronic obstructive pulmonary disease
Transcutaneous electrical nerve stimulation over acupoints
Systematic review
1 Background
Chronic obstructive pulmonary disease (COPD) is a disease characterized by persistent respiratory symptoms and airflow limitations attributed to highly exposures to poisonous air particles (Singh et al., 2019). Besides causing social and economic burden, COPD has high morbidity and mortality rate worldwide with 3,000,000 dead recorded in 2005 (Shino et al., 2013; Sikich, 2012; Wright et al., 2005). WHO predicts that the mortality rate of COPD will continue to rise by 2030.
Based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, the COPD patients should receive medications, undergo pulmonary rehabilitation, and have appropriate exercise to improve the lung functions and boost the activity tolerance. However, some patients who received adequate treatments did not show positive outcomes (Singh et al., 2019). In addition, treating COPD with oral hormones, aminophylline and bronchodilators may cause adverse effects in patients. For instance, inhalation of steroids increased the risk of pneumonia and myasthenia in COPD patients (Ni et al., 2014). These inevitable consequences have prompted the exploration of alternative treatments to treat COPD.
Acupuncture had been widely reported to relieve the symptoms of dyspnea in cancer (Cohen et al., 2005; Pan et al., 2000) and respiratory diseases (Davis et al., 2001; Jobst et al., 1986; Lewith et al., 2004). The hallmarks of COPD are chronic inflammatory and immune responses (Brusselle et al., 2011). Acupunture therapy, for instance, stimulation on ST36 (Zusanli) has been shown regulate inflammation in mice (Lim et al., 2016) and studies have reported that acupuncture may help relieve pulmonary diseases by diminishing bronchial immune-mediated inflammation (Carneiro et al., 2005; Zijlstra et al., 2003). Clinical studies have reported that acupuncture alleviated the COPD in patients (Jobst, 1995) by reducing the breathlessness symptoms and improving 6-minute walk distance (6MWD) performance (Suzuki et al., 2012; Suzuki et al., 2008). Hence, acupuncture is a potential alternative in treating COPD.
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive method to stimulate the human body through a low-frequency pulse current. Started in 1970s, it was mainly applied to relieve pain and provide functional recovery. Numerous studies showed that TENS was beneficial in rehabilitation of COPD (Bourjeily-Habr et al., 2002; Neder et al., 2002). By applying TENS on acupuncture points (acu-TENS), studies demonstrated improved lung functions in COPD patients (Lau and Jones, 2008; Meglic et al., 2011; Ngai et al., 2010). Lau et al. found that a single session of treatment with acu-TENs on EX-B-1(Dingchuan) could increase predicted FEV1% value and reduced the severity of breathlessness (Lau et al., 2008). Ngai et al. found that multi-sessions of acu-TENS stimulation on EX-B-1 could improve physiological functions in COPD patients (Ngai et al., 2010). At present, the mechanisms of acu-TENS treatment to COPD remains unclear. However, studies had demonstrated the breathlessness-relieving effect of the acu-TENS treatment could have been attributed to the stimulation of hypothalamus that promotes the release of β-endorphin that relaxes the airway (Jones et al., 2011; Ngai et al., 2010). Being a noninvasive treatment that is applied to specific acupoints, TENS can achieve similar therapeutic effects of acupuncture and moxibustion (Grant et al., 1999; Kerr et al., 2003). Acu-TENS is constantly being studied in combination with acupuncture for their effects on COPD as it shares the same mechanism and efficacy as acupuncture.
In this review, we aim to evaluate the clinical efficacy and safety of acupuncture for COPD. This review will give a better understanding of acupuncture and its combinational therapy in providing health benefits to COPD patients.
2 Methods
2.1 Search strategy
Literatures about acupuncture and/or acu-TENS for COPD were searched from database. English and Chinese database including Embase, PubMed, The Cochrane Library, wer VIP, WanFang Data, CNKI and CBM were searched from their dates of inception until June 2016. Only controlled studies were included. The following terms were applied to literature searching: (1) Chronic obstructive pulmonary disease (2) COPD, (3) 1 OR 2, (4) acupuncture, (5) acupoint, (6) transcutaneous electrical nerve stimulation, (7) TENS, (8) acu – TENS, (9) 4 OR 5 OR 6 OR 7 OR 8, (10) 3 AND 9. The same terms in Chinese were also searched in Chinese database. Two reviewers selected and evaluated the articles based on the search terms, databases, inclusion and exclusion criteria.
2.2 Eligibility criteria
Randomized controlled trials of acupuncture and/or acu-TENS on COPD, with or without blinding were included. The participants were patients with COPD diagnosed based on GOLD guidelines (Singh et al., 2019), Traditional Chinese Medicine Diagnostic and Therapeutic Protocols for 105 Diseases in 24 Disciplines (The State Administration of Traditional Chinese Medicine, 2011) or Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine (The State Administration of Traditional Chinese Medicine, 2002). The interventions included acupuncture and/or acu-TENS combined with either TCM, western medicine or rehabilitation exercise were evaluated comprehensively. These were not limited to the choice of acupoints, treatment sessions, western medicine treatments, TCM treatments, treatment courses and rehabilitation exercise programs.
The comparison between all acupuncture-related therapies were summarized as below:
-
(1)
The treatment group was the patients receiving acupuncture or acu-TENS alone, while the control group was the patients receiving western medicine alone.
-
(2)
The treatment group was the patients receiving acupuncture or acu-TENS combined with western medicine, while the control group was the patients receiving western medicine alone.
-
(3)
The treatment group was the patients receiving acupuncture alone or acu-TENS, while the control group was the patients receiving nothing (blank) or placebo.
-
(4)
The treatment group was the patients receiving acupuncture or acu-TENS combined with TCM, while the control group was the patients receiving TCM alone.
-
(5)
The treatment group was the patients receiving acupuncture or acu-TENS combined with rehabilitation exercise, while the control group was the patients receiving single rehabilitation exercise.
2.3 Exclusion criteria
Literatures with following criteria were excluded from this study: (1) COPD with severe cardiovascular and cerebrovascular diseases, liver, kidney, lung and other important organ dysfunction in patients. (2) Studies which experimental design were not standardized with no clear diagnosis and outcome assessment criteria. (3) Studies with unextractable data.
2.4 Data extraction
All data were extracted from studies independently by two authors and any disagreement was resolved by a third author. The following information was extracted: (1) The basic information of the research including research topic, first author, publication of the journal and time of publication; (2) The baseline characteristics of the research object including the number of samples in each group, age, gender and disease status of patients; (3) specific details of the interventions, follow-up period, etc; (4) the outcome measurements.
3 Types of outcome measurement
3.1 Primary outcomes
-
(1)
Clinical efficacy. According to the Guiding Principle of Clinical Research on New Drugs of Traditional Chinese Medicine (Zheng, 2002) , the clinical efficacy, also known as reduction rate of syndrome points (n), is calculated as follows: (total score before treatment - total score after treatment) / total score before treatment × 100%. As the standard, to determine the comprehensive effect. Clinical control for n ≥ 90%, markedly effective for 70%≤n < 90%, effective 30%≤n < 70%, ineffective for n ≤ 30%. Total effective rate = (clinical control + effective + effective)/total number × 100%.
-
(2)
The quality of life was assessed based on St George's Respiratory Questionnaire (SGRQ), COPD assessment test (CAT) and modified Medical Research Council (mMRC). A lower score indicates a higher quality of life and vice versa.
3.2 Secondary outcomes
-
(1)
Lung function: The forced expiratory volume in 1 s (FEV1) and FEV1% predicted; forced vital capacity (FVC) and FVC% predicted.
-
(2)
The number of acute exacerbations.
-
(3)
(3) 6-min walk distance (6MWD) test.
-
(4)
Borg score, using a modified 10-point Borg category scale (Borg, 1982), in which the levels of dyspnea with 0 signifying “Nothing at all, barely breathless” and 10 signifying “Very strong, severely breathless” were evaluated. The higher the Borg score, the lower the patient's tolerance to the activity, and vice versa.
-
(5)
Adverse effects.
3.3 Quality assessment
The quality of each study was assessed using the Cochrane risk-of-bias assessment tool. Consolidated standards of reporting trials (CONSORT) (Schulz et al., 2010) statement was used to identify the changes in quality of reporting for acupuncture trials over time. Using scale entry, the score entry for each experiment was recorded as 0 points (no report or high risk of bias), 0.5 point (partial report or bias possible), 1 point (reportable or low risk of bias). The Standards for reporting Interventions in Clinical Trials of Acupuncture (STRICTA) Evaluation Table (MacPherson and Altman, 2009) was used to evaluate the status of each experimental interventions with the entry of ‘yes’ or ‘no’.
3.4 Statistical analysis
The Cochrane Collaboration software program RevMan 5.3 was used for meta-analysis. As the effect analysis statistic, the continuous variable is the mean difference (MD) while the categorical variable is the relative risk (RR). The 95% CI and P value of each effect were given. Heterogeneity was analyzed using χ2 test analysis (test level α = 0.1) combined with the I2 statistics with values > 50% indicating strong heterogeneity. If the heterogeneity is low in the analyses (P ≥ 0.1 and I2 < 50%), a fixed-effect model is used for meta-analysis. If heterogeneity exist (P < 0.1 and/or I2 ≥ 50%), a random-effect model was used after the significant clinical heterogeneity was excluded. Sensitivity analysis was used to test the stability of the estimates. For the treatment measures to take different combinations of data, subgroup analysis was carried out based on different treatment programs.
4 Results
4.1 Study characteristics
4.1.1 Characteristics of the eligible studies
The flow of the publication’s selection was summarized in Fig. 1. A total of 167 publications were identified through the literature database search. After the further selection and screening, 50 full-text articles were assessed for eligibility. Subsequently, 11 articles were selected for systemic reviews. Among these, three articles involving acupuncture versus (vs) seretide (Gao et al., 2011; Lu et al., 2016; Xie and Yu, 2014), two articles involving acupuncture + western medicine vs western medicine (Suzuki et al., 2012; Suzuki et al., 2008), two articles involving acupuncture + rehabilitation exercise vs placebo + rehabilitation exercise (Guo et al., 2013; Tong et al., 2014), two articles involving acu-TENS + western medicine vs placebo + western medicine (Lau et al., 2008; Liu et al., 2014), one article involving acupuncture + TCM vs TCM (Wan et al., 2009) and one article involving acupuncture + Seretide vs Seretide (Liu et al., 2015) were selected.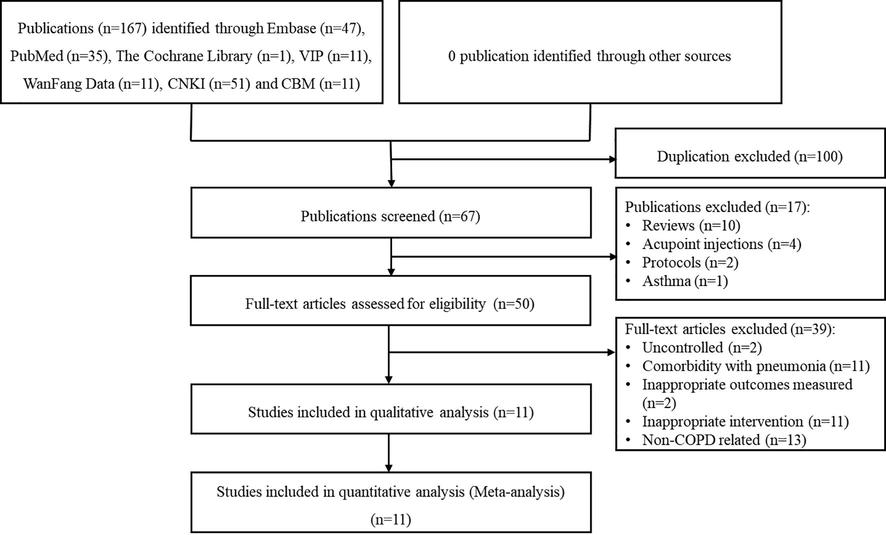
Flowchart for the selection of studies for meta-analysis.
4.1.2 Patient characteristics
Based on Table 1, a total of 709 COPD patients were enrolled from 11 publications in which the sample size of each study ranged from 30 to 150. Except for the study by Gao et al. (2011), the gender composition of 10 studies were reported as 439 males and 218 females. Besides, the age of most studies was above 60-year-old, excluding the studies by Lu et al. (2016) and Liu et al. (2015). Regarding lung function, study by Lau et al. (2008) showed lung function was GOLD I/II with no specified function reported. The other studies recorded that the lung function GOLD I/II/III/IV were 0/77/124/80 respectively. The lung functions were not reported in the studies by Gao et al. (2011), Lu et al. (2016) and Wan et al. (2009) (Table 1 and Supplementary Table 1). Exp, experimental group; Con, control group; M/F, male/female; biw, biweekly; HZ, Hertz; qod, every other day; qw, once a week; qd, once a day; W, week; M, month; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Literature
N(exp)
samples
N(con)
sample
Acupoint
Practice
Session
Control
Adverse effect
Gao J 2011
30
Outpatients, age 64.87 ± 8.73
30
Outpatients, age 65.25 ± 10.66
EX-B-1(Dingchuan), BL-13(Feishu), ST-36(Zusanli)
Warm needle, 2 moxa cones, needle 30 min
qod for 8 W
Seretide50/250
No report
Lu H 2016
45
Inpatients, M/F 24/21, age 54.2 ± 2.3
45
Inpatients, M/F 27/18, age 57.4 ± 3.6
EX-B-1(Dingchuan), BL-13(Feishu), ST-36(Zusanli)
Warm needle, needle 20 min
qod for 2 M
Seretide50/250
No report
Wan WR 2009
75
Outpatients and inpatients, M/F 47/28, age 62.4 ± 8.56
75
Outpatients and inpatients, M/F 45/30, age 61.8 ± 10.1
DU-14(Dazhui), BL-13(Feishu), RN-17(Danzhong), RN-4(Guanyuan), SJ-6(Zhigou), LU-7(Lieque), LI-6(Pianli) + TCM
Common needle, mild reinforcing-reducing method, 10 min
qd for 12d, 3 session
TCM
No report
Tong J 2014
16
Outpatients, M/F 15/1, age 64 ± 6, GOLDI/II/III/IV 0/5/6/5
14
Outpatients, M/F 12/2, age 67 ± 6, GOLDI/II/III/IV 0/4/5/5
RN-17(Danzhong), ST-18(Rugen), RN-4(Guanyuan), RN-12(Zhongwan), ST-25(Tianshu), ST-16(Yingchuang) + exercise
Electric acupuncture, 1-2HZ, 30 min
2–3 times per week for 5 W
placebo + exercise
No report
Guo YM 2013
17
Outpatients, M/F 17/1, age 65.28 ± 5.73, GOLDI/II/III/IV 0/5/6/7
14
Outpatients, M/F 13/2, age 66.6 ± 6.06, GOLDI/II/III/IV 0/4/5/6
RN-17(Danzhong), ST-18(Rugen)、RN-4(Guanyuan), RN-12(Zhongwan), ST-25(Tianshu), ST-16(Yingchuang) + exercise
Electric acupuncture, frequency 100/min, 30 min
qod, 7 times in a session, total 2 sessions
placebo + exercise
No report
Xie JH 2014
40
Inpatients, M/F 22/18, age 68.9 ± 8.7
40
Inpatients, M/F 18/22, age 68.5 ± 9.6
ST-36(Zusanli), BL-13(Feishu), EX-B-1(Dingchuan), BL-43(Gaohuang), BL-15(Xinshu), DU-14(Dazhui), BL-12(Fengmen)
Warm needle, 2 moxa cones, 30 min
qod for 8 W
Seretide50/250
No report
Liu LJ 2015
40
Outpatients, M/F 24/16, age 58.3 ± 12.4, GOLDIII/IV 27/13
40
Outpatients, M/F 26/14, age 63.2 ± 10.7, GOLDIII/IV 29/1
BL-13(Feishu), BL-23(Shenshu), RN-6(Qihai), RN-4(Guanyuan), EX-B-1(Dingchuan), RN-17(Danzhong), ST-36(Zusanli) + Seretide
Common needle, needle 10 min
biw for 3 M
seretid 50/250
No report
Suzuki M 2008
15
Outpatients, M/F 15/0, age 71.2 ± 3.7, GOLDI/II/III/IV 0/8/4/3
15
Outpatients, M/F 15/0, age 71.4 ± 3.9 GOLDI/II/III/IV 0/8/5/2
LU-1(Zhongfu), LU-5(Chize), LU-9(Taiyuan), RN-4(Guanyuan), RN-12(Zhongwan), KI-3(Taixi), BL-13(Feishu), BL-23(Shenshu) + conventional medicine
Common needle, needle 15 min
qw for 10 W
conventional medicine
3 mild contusion and pain
Suzuki M 2012
34
Ambulatory outpatients, M/F 31/3, age 72.7 ± 6.8, GOLDI/II/III/IV 0/6/16/12
34
Ambulatory outpatients, M/F 32/2, age 72.5 ± 7.4, GOLDI/II/III/IV 0/13/8/13
LU-1(Zhongfu), LU-9(Taiyuan), RN-4(Guanyuan), RN-12(Zhongwan), KI-3(Taixi), BL-13(Feishu), BL-23(Shenshu), BL-20(Pishu), LI-18(Futu), SI-4(Wangu), ST-36(Zusanli) + conventional medicine
Common needle, needle 50 min
qw for 12 W
conventional medicine
No report
Liu XM 2014
25
Ambulatory outpatients, M/F 10/15, age 66.04 ± 8.815, GOLDI/II/III/IV 0/13/6/6
25
Ambulatory outpatients., M/F 15/10, age 66.48 ± 9.368, GOLD I/II/III/IV 0/11/7/7
EX-B-1(Dingchuan), BL-13(Feishu), BL-23(Shenshu), ST-36(Zusanli) + conventional medicine
acu-TENS, 2HZ, 40 min
qod for 4 W
placebo + conventional medicine
No adverse effect
Lau KSL 2008
23
Ambulatory outpatients, M/F 19/4, age 77.5 ± 6.5, GOLD I/II
23
Ambulatory outpatients, M/F 12/11, age 73.7 ± 6.8, GOLD I/II
EX-B-1(Dingchuan) + conventional medicine
acu-TENS, 4HZ, 45 min
single session of 45 min
placebo + conventional medicine
No adverse effect
4.1.3 Study designs and treatment intervention characteristics
All 11 studies were RCTs including one matched-pair parallel control study (Suzuki et al., 2008), four single-blinded studies (Guo et al., 2013; Lau et al., 2008; Liu et al., 2014; Suzuki et al., 2012) and one double-blinded study (Tong et al., 2014) whereas the experimental design of other five studies were not mentioned. The treatment intervention details for the experimental and control groups, such as the practice of acupuncture, acupoints, treatment period, drug treatments were illustrated in Table 1.
4.1.4 Quality of design
According to CONSORT terms, the quality of randomized controlled trials (RCTs) designs were analyzed. Based on Supplementary Table 2, there were many reported factors affect the quality of experiments. Most commonly, the characteristics of study such as the blinding of study and randomized trials were not described in seven studies (Gao et al., 2011; Guo et al., 2013; Liu et al., 2015; Lu et al., 2016; Suzuki et al., 2008; Wan et al., 2009; Xie et al., 2014). Lack of description of ethics committee approval, blind implementation, side effects record and details on experimental procedures were also found some studies. Besides, STRICTA method was implemented to evaluate the intervention details on acupuncture. Based on Supplementary Table 3, there were some information regarding the acupuncture were underreported. For instance, the basis and historical context of acupuncture, acupuncture needle depth and the qualification of acupuncturist. Compiling the items from CONSORT, Cochrane Risk of Bias and STRICTA, the quality of the studies was rated as “very good”, “good”, “poor” and “very poor” (Supplementary Table 4). In short, five publications were rated as ”very good“ while one publication was rated ”good“. Nevertheless, three publications were rated ”poor“. Lastly, two publications were rated as ”very poor“ (Supplementary Table 5). The publication bias was illustrated in a funnel plot (Supplementary Fig. 1), indicated that there might be publication bias in the incorporated literatures.
4.1.5 Risk of bias in individual studies
The risk of bias was assessed using the Cochrane risk-of-bias assessment tool. Four studies (Lau et al., 2008; Liu et al., 2014; Suzuki et al., 2012; Tong et al., 2014) were reported in detail. Thus, the risk of bias was low and the quality of these studies was high. Other studies had different degree of risk of bias. The most significant risk of bias in the included trials was the randomized methods, sampling procedures and concealment of assignments (Fig. 2).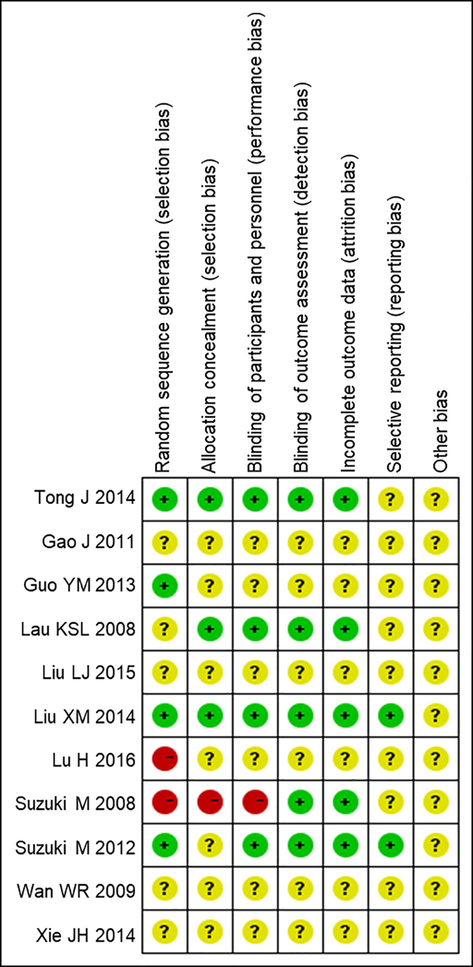
Cochrane risk-of-bias. Review authors’ judgement about each risk of item for each included study. Green circle, low risk of bias; yellow circle, unclear risk of bias; red circle, high risk of bias.
4.2 Effects of interventions
4.2.1 The total efficiency
The treatment efficacy was reported in two RCTs (Wan et al., 2009; Xie et al., 2014) (Fig. 3). In calculating the effective rate at the end of treatment, we considered the significant as “effective”, ineffective were considered as “invalid” in the clinical control group and thus converted to dichotomous variables to calculate the effective rate of the combined effect risk ratio (RR) and 95% confidence intervals (CI). The results of these two RCTs showed no statistical heterogeneity (P = 0.32, I2 = 0%). The fixed effect model was used to analyze the effect of treatment. The effective rate of the experimental group after treatment was significantly higher than that of the control group (Mean Difference (MD) = 1.11, 95% CI 1.02–1.21, P = 0.02). In relative to the control group, acupuncture combined with TCM and acupuncture combined with western medicine could improve clinical efficacy. However, more experiments are needed to verify the results due to little RCTs.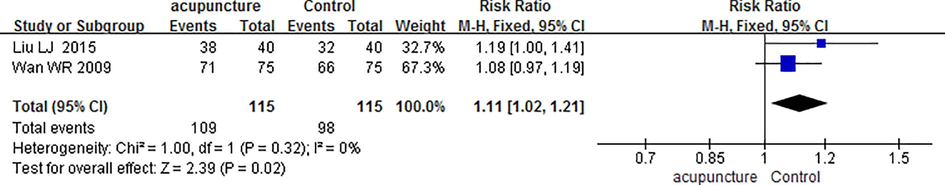
Forest plot of risk ratio of the total efficiency on different studies.
4.2.2 Quality of life
Four RCTs (Gao et al., 2011; Lu et al., 2016; Suzuki et al., 2012; Tong et al., 2014) reported SGRQ score (Fig. 4). The results showed that there was a low statistical heterogeneity in SGRQ score (P = 0.23, I2 = 31%). The fixed effect model was used to analyze the SGRQ score of the experimental group after treatment, which was significantly lower than that of the control group (MD = −3.66, 95% CI 5.56–1.76, P = 0.0002). One RCT (Liu et al., 2014) reported the COPD assessment test (CAT) score (Fig. 5). The results showed that CAT score of acu-TENS combined with western medicine group was lower than that of placebo needle combined with western medicine group although no significant difference was reported (MD = −1.90, 95% CI −5.23–1.43, P = 0.26). One RCT (Suzuki et al., 2012) reported a significantly lower mMRC score on experimental group (acupuncture + conventional western medicine) than control group (conventional western medicine) (MD = −0.50, 95% CI −1.08–0.08, P = 0.09) (Fig. 6). Besides, there were no exacerbations reported in these RCTs. Nevertheless, a few mild adverse effects, such as mild contusion and pain, were reported in study by (Suzuki et al., 2008). These results indicated that acupuncture could improve the quality of life of patients as compared to control group.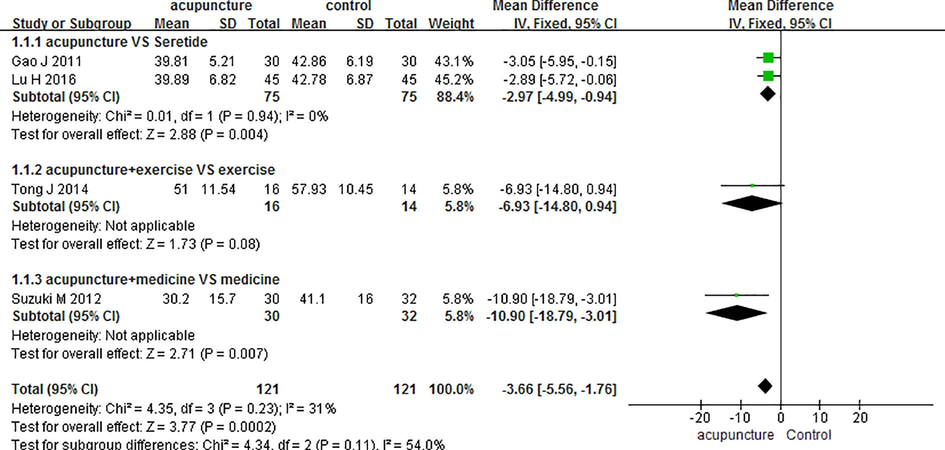
Forest plot of mean difference of the SGRQ scores on different studies. SGRQ scores, St George's Respiratory Questionnaire (SGRQ) score.
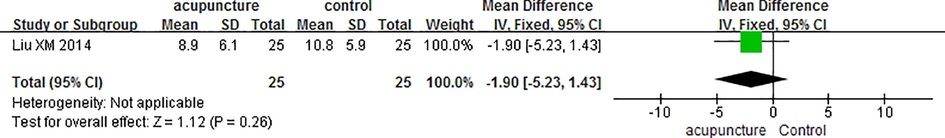
Forest plot of mean difference of the CAT score on different studies. CAT, COPD assessment test.
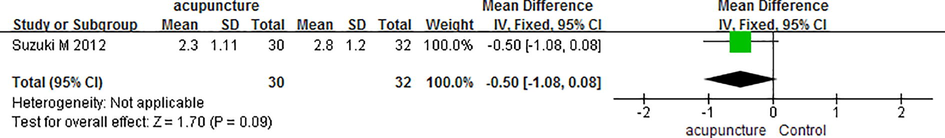
Forest plot of mean difference of mMRC score on different studies. mMRC, modified British medical research council.
4.3 Lung function
4.3.1 FeV1
FEV1 was reported in seven RCTs (Gao et al., 2011; Lau et al., 2008; Lu et al., 2016; Suzuki et al., 2012; Suzuki et al., 2008; Wan et al., 2009; Xie et al., 2014) and showed a large heterogeneity (P < 0.00001, I2 = 83%). After excluding the study by Wan et al. (2009), the other six studies showed a low heterogeneity (P = 0.16, I2 = 37%) and high sensitivity. Subgroup analysis was performed on FEV1 with different treatment intervention of acupuncture. The difference in three RCTs (Gao et al., 2011; Lu et al., 2016; Xie et al., 2014) involving acupuncture vs Seretide were statistically significant (MD = −0.19, 95% CI 0.32–0.06, P = 0.004), suggesting acupuncture alone was less effective than Seretide alone. Despite that, other RCTs showed that FEV1 in the group experiencing acupuncture combined with other interventions was lower than the group experiencing monotherapy without acupuncture. For instance, one RCT subgroup (Wan et al., 2009) showed that the FEV1 in the experimental group (acupuncture + TCM) was significantly higher than that in the control group (TCM only) after the treatment (MD = 0.41, 95% CI 0.25 to 0.57, P < 0.00001). Nonetheless, experimental groups showed not significant lowered FEV1 value as compared to the control group in the studies by two RCT subgroups (Suzuki et al., 2012; Suzuki et al., 2008) (MD = 0.07, 95% CI 0.16 to 0.30, P = 0.53) and one RCT (Lau et al., 2008) subgroup (MD = −0.04, 95% CI 0.30 to 0.22, P = 0.76) (Fig. 7).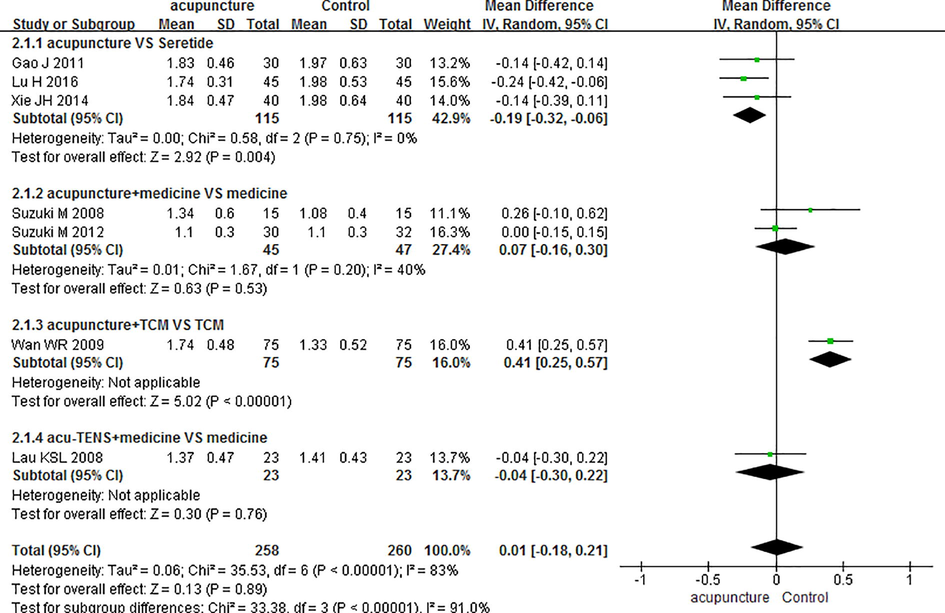
Forest plot of mean difference of the FEV1 on different studies. FEV1, The first second forced expiratory volume. TCM, Traditional Chinese medicine. Acu-TENS, transcutaneous electrical nerve stimulation over acupoints.
4.3.2 FeV1% predicted
FEV1% predicted was reported in 10 RCTs (Gao et al., 2011; Guo et al., 2013; Liu et al., 2015; Liu et al., 2014; Lu et al., 2016; Suzuki et al., 2012; Suzuki et al., 2008; Tong et al., 2014; Wan et al., 2009; Xie et al., 2014) and showed a large heterogeneity. After excluding the study by Wan et al. (2009), the other studies showed a moderate heterogeneity (P = 0.02, I2 = 56%) and a high sensitivity. The RCT did not report a baseline of GOLD staging of lung function and should not be compared with other studies. The results showed that FEV1% predicted was higher in all the experimental group as compared to the control group. For instance, the studies by two RCTs (Guo et al., 2013; Tong et al., 2014) showed that FEV1% predicted in the patients experiencing acupuncture + exercise was significantly higher than in the patients experiencing placebo needle + exercise (MD = 15.51, 95% CI 6.30 to 24.71, P = 0.001). Besides, one RCT (Wan et al., 2009) showed that FEV1% predicted in the patients receiving acupuncture + TCM was significantly higher than that in the patients receiving TCM (MD = 27.6, 95% CI 24.54 to 30.66, P < 0.00001). Nevertheless, the other studies showed non-significant increase in the FEV1% in the experimental group as compared to control group (Fig. 8).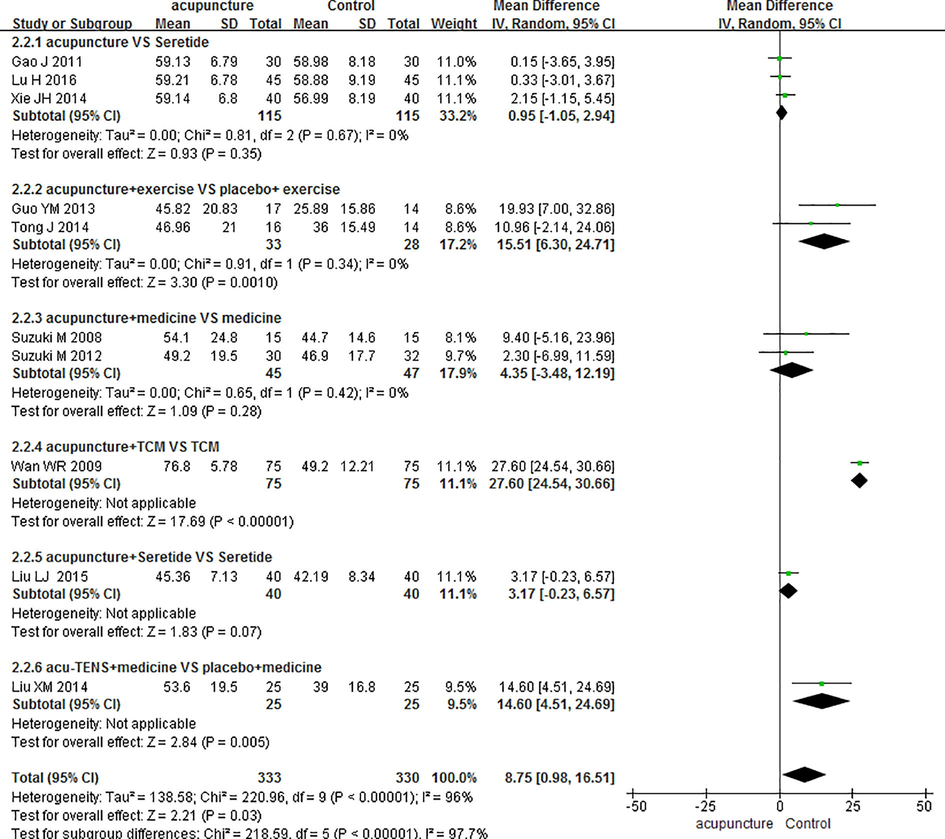
Forest plot of mean difference of the FEV1% predicted on different studies. FEV1% predicted, the ratio of the measured values of predicted values of forced expiratory volume in 1 s. TCM, Traditional Chinese medicine. Acu-TENS, transcutaneous electrical nerve stimulation over acupoints.
4.3.3 FvC
The FVC were reported in four RCTs (Lau et al., 2008; Suzuki et al., 2012; Suzuki et al., 2008; Wan et al., 2009) and showed moderate heterogeneity (P = 0.12, I2 = 48%). Using a fixed-effect model analysis, the FVC in the experimental group was significantly higher than that in the control group (MD = 0.16, 95% CI 0.01 to 0.30, P = 0.04). This showed that acupuncture treatment of COPD could improve FVC and lung functions (Fig. 9).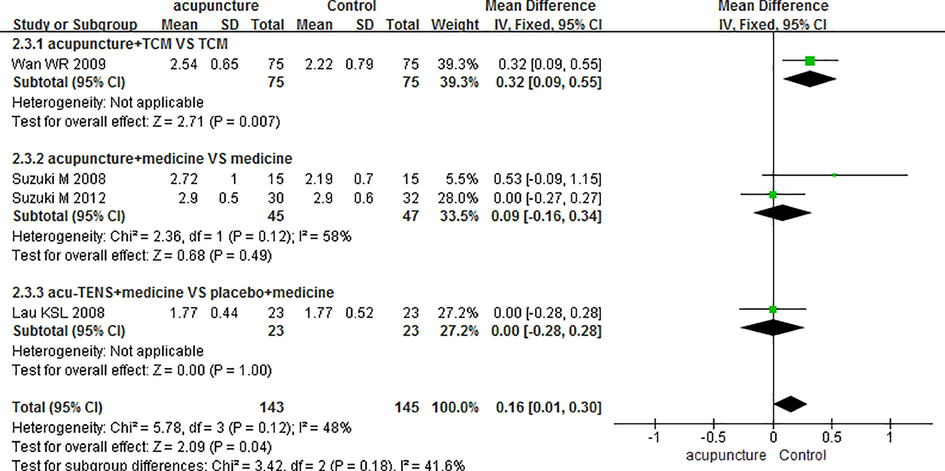
Forest plot of mean difference of the FVC on different studies. FVC, the volume of forced vital capacity. TCM, Traditional Chinese medicine. Acu-TENS, transcutaneous electrical nerve stimulation over acupoints.
4.3.4 FvC% predicted
FVC% was reported in three RCTs (Guo et al., 2013; Liu et al., 2014; Tong et al., 2014) and showed no statistically significant heterogeneity (P = 0.46, I2 = 0%). The fixed-effect model analysis showed that the FVC% predictive value of the experimental group was significantly higher than that of the control group after treatment (MD = 7.93, 95% CI 1.83 to 14.03, P = 0.01). This showed that acupuncture treatment of COPD can improve FVC% predicted and lung function (Fig. 10).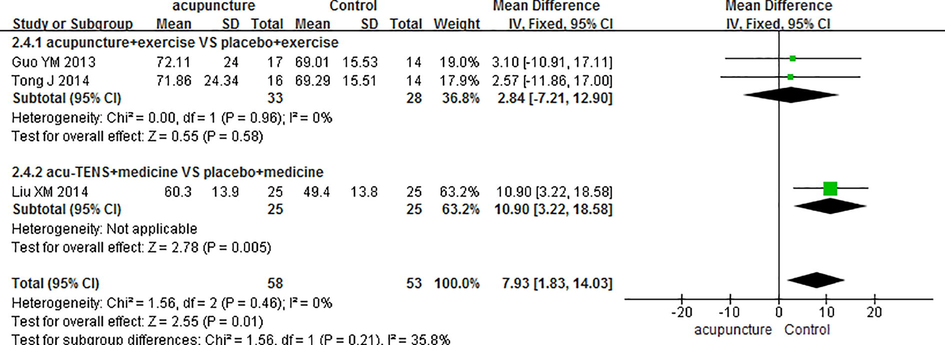
Forest plot of mean difference of the FIV% predicted on different studies. FVC% predicted, the ratio of the measured values of predicted values of forced expiratory volume in 1 s. Acu-TENS, transcutaneous electrical nerve stimulation over acupoints.
4.3.5 6MwD
6MWD was reported in six RCTs (Guo et al., 2013; Liu et al., 2015; Liu et al., 2014; Suzuki et al., 2012; Suzuki et al., 2008; Tong et al., 2014) and showed mild heterogeneity (P = 0.14, I2 = 40%). Using fixed-effect model analysis, the 6MWD of experimental group showed non-significant higher 6MWD results than the control group (MD = 4.98,95% CI 10.17 to 20.13, P = 0.52) (Fig. 11).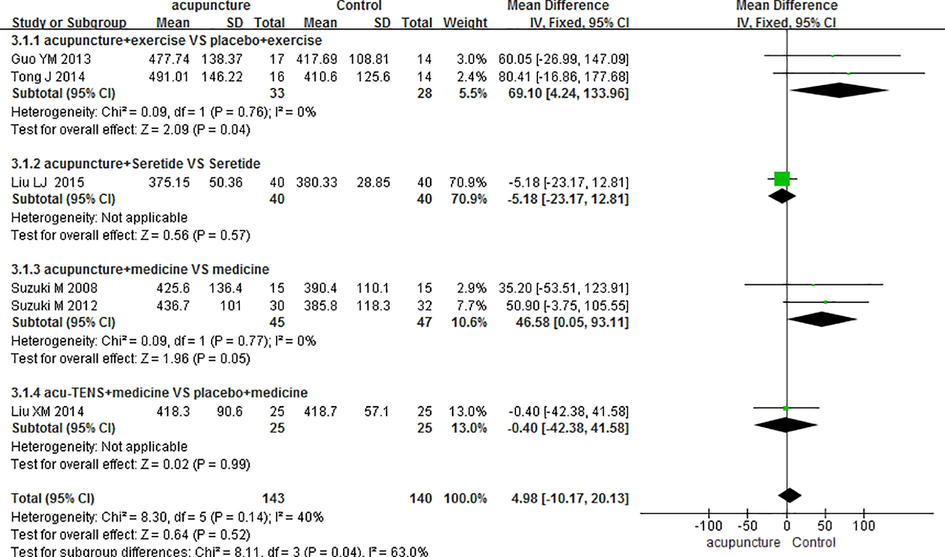
Forest plot of mean difference of 6MWD on different studies. 6MWD, 6 min walking distance. Acu-TENS, transcutaneous electrical nerve stimulation over acupoints.
4.3.6 Borg score
Borg score was reported in two RCTs (Suzuki et al., 2012; Suzuki et al., 2008) and showed mild heterogeneity among studies (P = 0.23, I2 = 30%). The fixed effect model analysis showed that Borg score in the experimental group was significantly lower than the control group (MD = -3.00, 95% CI −3.99 to −2.01, P = 0.00001). This showed that acupuncture treatment of COPD could improve the patients’ tolerance to exercise (Fig. 12).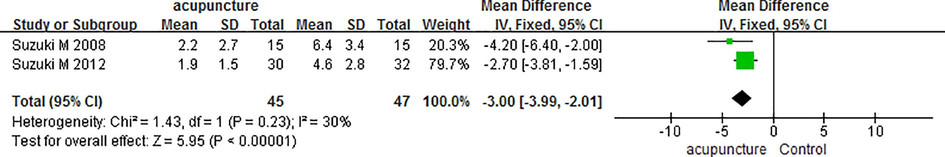
Forest plot of mean difference of Borg score on different studies. Borg score, a modified 10-point Borg category scale.
5 Discussion
Acupuncture has been widely used in the treatment of clinical chronic diseases. Our systematic review included a total of 709 COPD patients from 11 studies, most of whom were elderly, and all levels of lung functions were included. Our results show that acupuncture treatment of COPD improves the treatment efficiency (MD = 1.11, 95% CI 1.02 to1.21, P = 0.02), reduces the SGRQ score to improve the quality of life (MD = -3.66, 95% CI −5.56–1.76, P = 0.0002), increases FEV1% predicted (MD = 8.75, 95% CI 0.98 to 16.51, P = 0.03), increases FVC% predicted (MD = 7.93, 95% CI 1.83 to 14.03, P = 0.01) and increases FVC(L) (MD = 0.16, 95% CI 0.01 to 0.30, P = 0.04) and lowers the Borg score (MD = -3.00, 95% CI −3.99 to −2.01, P = 0.00001) but no significant difference in CAT score, mMRC score and 6MWD between acupuncture group and control group. The adverse reactions of acupuncture treatment were poorly reported. One study reported 3 cases of mild contusion and pain and two reported no adverse effects. Nevertheless, our combined data showed no significant difference in adverse effects between acupuncture group and control group. Therefore, acupuncture is a safe treatment method for COPD.
The acupuncture treatment itself varied across the 11 included RCTs. Different types of acupuncture including needle acupuncture, warm needle, electric acupuncture and acu-TENS were used and acupoints differed between the included studies. Acupoints such as EX-B-1 (Dingchuan), BL13 (Feishu), DU-14 (Dazhui), and ST36 (Zusanli) that mainly used in treating respiratory related symptoms and diseases are the most common acupoints used among the included studies. In addition, the frequency, duration and course of acupuncture treatment differed in each study. The course of acupuncture treatment can be from single 1 to 20 courses. Studies reported that 4 weeks of treatment is more acceptable. As the effects of acupuncture treatment are cumulative (Hwang et al., 2008), it is recommended that multiple courses be taken once a day for a total of 4 weeks (Liu et al., 2014).
The quality of the RCT design of the included RCTs were evaluated in accordance with the CONSORT items. The most common shortcomings of the eleven included RCTs include the type of study involved, the sample size, the approval of ethics committee for clinical trials, the details on random sequence generation, and the details of standard procedure. In addition, blinding implementation of the study, the exit of study participants from the study, the use of the analysis of shedding cases such as intention-to-treat (ITT) analysis, the adverse effects of the treatment, the detailed record of adverse effects, the limitations and generalization of the study, research protocols and experimental registrations were not described.
We used STRICTA to evaluate the quality of the interventions. The most common shortcomings of the eleven included RCTs are: (1) the basis or background of the selected acupuncture was not reported, (2) the depth of acupuncture needle was not reported, (3) patients feedback such as getting Qi and soreness was not reported after acupuncture treatment, (4) the treatment site and related information including the operating instructions for the therapist was not reported, (5) the information and explanations to the patients was not reported, (6) No description of the experience or years of acupuncture practice of the participating acupuncturists.
There are also some limitations in this systematic review. The number of studies eventually included was small, and we retrieved only documents in both English and Chinese but no other languages, such as Japanese and Korean, which decreased the credibility of the results of this study to some extent.
6 Conclusions
Our systematic review shows that the combination of acupuncture and western medicine, rehabilitation exercise and traditional Chinese medicine have clinical relevant benefits in alleviating the clinical symptoms, improving the quality of life and improving the treatment efficiency in COPD patients. It is a safe treatment albeit more high-quality RCTs comparing acupuncture with the conventional treatments are warranted to further evaluate the effects of acupuncture on COPD. Nevertheless, a simple alternative to acupuncture treatment of drugs is not recommended.
Acknowledgement
This study was supported by a project of Health and Family Planning Commission of Chengdu city, Sichuan province, China (project no. 2018098).
References
- Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc.. 1982;14:377-381.
- [Google Scholar]
- Randomised controlled trial of transcutaneous electrical muscle stimulation of the lower extremities in patients with chronic obstructive pulmonary disease. Thorax. 2002;57:1045-1049.
- [CrossRef] [Google Scholar]
- New insights into the immunology of chronic obstructive pulmonary disease. Lancet. 2011;378:1015-1026.
- [CrossRef] [Google Scholar]
- Effect of electroacupuncture on bronchial asthma induced by ovalbumin in rats. J. Altern. Complement. Med.. 2005;11:127-134.
- [CrossRef] [Google Scholar]
- Acupuncture: role in comprehensive cancer care–a primer for the oncologist and review of the literature. Integr. Cancer Ther.. 2005;4:131-143.
- [CrossRef] [Google Scholar]
- A pilot project to assess the methodological issues involved in evaluating acupuncture as a treatment for disabling breathlessness. J. Altern. Complement. Med.. 2001;7:633-639.
- [CrossRef] [Google Scholar]
- Comparative research on effect of warm needling therapy on pulmonary function and life quality of patients with COPD in the stable phase. Zhongguo Zhen Jiu. 2011;31:893-897.
- [Google Scholar]
- A randomized comparative trial of acupuncture versus transcutaneous electrical nerve stimulation for chronic back pain in the elderly. Pain. 1999;82:9-13.
- [CrossRef] [Google Scholar]
- Effect of Acupuncture on Respiratory Function of Stable Chronic Obstructive Pulmonary Disease. J. Guangzhou Univers. Tradit. Chinese Med.. 2013;30:658-663.
- [Google Scholar]
- Pneumoretroperitoneum following acupuncture. J. Altern. Complement. Med.. 2008;14:1299-1301.
- [CrossRef] [Google Scholar]
- Controlled trial of acupuncture for disabling breathlessness. Lancet. 1986;2:1416-1419.
- [CrossRef] [Google Scholar]
- A critical analysis of acupuncture in pulmonary disease: efficacy and safety of the acupuncture needle. J. Altern. Complement. Med.. 1995;1:57-85.
- [CrossRef] [Google Scholar]
- Acute effects of acu-TENS on FEV1 and blood beta-endorphin Level in chronic obstructive pulmonary disease. Altern. Ther. Health Med.. 2011;17:8-13.
- [Google Scholar]
- Acupuncture in the management of chronic low back pain: a blinded randomized controlled trial. Clin. J. Pain. 2003;19:364-370.
- [CrossRef] [Google Scholar]
- A single session of Acu-TENS increases FEV1 and reduces dyspnoea in patients with chronic obstructive pulmonary disease: a randomised, placebo-controlled trial. Aust. J. Physiother.. 2008;54:179-184.
- [CrossRef] [Google Scholar]
- Can a standardized acupuncture technique palliate disabling breathlessness: a single-blind, placebo-controlled crossover study. Chest. 2004;125:1783-1790.
- [CrossRef] [Google Scholar]
- Anti-Inflammatory Effects of Acupuncture Stimulation via the Vagus Nerve. PLoS ONE. 2016;11:e0151882
- [CrossRef] [Google Scholar]
- Clinical effect observation on acupuncture for chronic obstructive pulmonary disease. J. Acupunct. Tuina Sci.. 2015;13:306-311.
- [CrossRef] [Google Scholar]
- Effects of transcutaneous electrical acupoint stimulation on patients with stable chronic obstructive pulmonary disease: A prospective, single-blind, randomized, placebo-controlled Study. J. Altern. Complement. Med.. 2014;21:610-616.
- [CrossRef] [Google Scholar]
- Clinical Observation on 45 Cases of Chronic Obstructive Pulmonary Disease Treated by Warm Needling Moxibustion. Chin. J. Ethnomed. Ethnopharm.. 2016;25:111-112.
- [Google Scholar]
- Improving the quality of reporting acupuncture interventions: describing the collaboration between STRICTA, CONSORT and the Chinese Cochrane Centre. J. Evid. Based Med.. 2009;2:57-60.
- [CrossRef] [Google Scholar]
- Feasibility of transcutaneous electrical muscle stimulation in acute exacerbation of COPD. Wien. Klin. Wochenschr.. 2011;123:384-387.
- [CrossRef] [Google Scholar]
- Home based neuromuscular electrical stimulation as a new rehabilitative strategy for severely disabled patients with chronic obstructive pulmonary disease (COPD) Thorax. 2002;57:333-337.
- [CrossRef] [Google Scholar]
- Effect of 4 weeks of Acu-TENS on functional capacity and beta-endorphin level in subjects with chronic obstructive pulmonary disease: a randomized controlled trial. Respir. Physiol. Neurobiol.. 2010;173:29-36.
- [CrossRef] [Google Scholar]
- Inhaled corticosteroids (ICS) and risk of mycobacterium in patients with chronic respiratory diseases: a meta-analysis. J. Thorac. Dis.. 2014;6:971-978.
- [CrossRef] [Google Scholar]
- Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life. A systematic review. J. Pain Symptom Manage.. 2000;20:374-387.
- [CrossRef] [Google Scholar]
- CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332
- [CrossRef] [Google Scholar]
- Pulmonary hypertension complicating interstitial lung disease and COPD. Semin. Respir. Crit. Care Med.. 2013;34:600-619.
- [CrossRef] [Google Scholar]
- Community-based multidisciplinary care for patients with stable chronic obstructive pulmonary disease (COPD): an evidence-based analysis. Ont. Health Technol. Assess. Ser.. 2012;12:1-51.
- [Google Scholar]
- Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur. Respir. J.. 2019;53
- [CrossRef] [Google Scholar]
- A randomized, placebo-controlled trial of acupuncture in patients with chronic obstructive pulmonary disease (COPD): the COPD-acupuncture trial (CAT) Arch. Intern. Med.. 2012;172:878-886.
- [CrossRef] [Google Scholar]
- The effect of acupuncture in the treatment of chronic obstructive pulmonary disease. J. Altern. Complement. Med.. 2008;14:1097-1105.
- [CrossRef] [Google Scholar]
- Criteria of diagnosis and therapeutic effects of diseases and syndromes in traditional chinese medicine. Beijing: China Medical Science Press; 2002. p. :54-58.
- Traditional chinese medicine diagnostic and therapeutic protocols for 105 diseases in 24 disciplines. Beijing: Division of Medical Administration, State Administration of Traditional Chinese Medicine; 2011. p. :103-104.
- Regulatory effects of acupuncture on exercise tolerance in patients with chronic obstructive pulmonary disease at stable phase: a randomized controlled trial. Zhongguo Zhen Jiu. 2014;34:846-850.
- [Google Scholar]
- Clinical study on effect of lung-function of patients with COPD in remission stage treated by acupuncture and moxibustion combining with chinese herbs for warming kidney-yang and regulating qi. Chin. Arch. Tradit. Chin. Medi.. 2009;27:163-165.
- [Google Scholar]
- Pulmonary hypertension in chronic obstructive pulmonary disease: current theories of pathogenesis and their implications for treatment. Thorax. 2005;60:605-609.
- [CrossRef] [Google Scholar]
- Effect of warming needle moxibustion on pulmonary function of elderly patients with stable chronic obstructive pulmonary disease. World J. Acupunct. - Moxibustion. 2014;24:21-24.
- [CrossRef] [Google Scholar]
- Zheng, X. Y. 2002. Guiding Principle of Clinical Research on New Drugs of Traditional Chinese Medicine (Trial). Chinese Medical Science and Technology Press, 29-31.
- Anti-inflammatory actions of acupuncture. Mediators Inflamm.. 2003;12:59-69.
- [CrossRef] [Google Scholar]
Appendix A
Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jksus.2020.04.001.
Appendix A
Supplementary data
The following are the Supplementary data to this article:







