Translate this page into:
Determinants, predictors and negative impacts of burnout among health care workers during COVID-19 pandemic
⁎Corresponding author at: The Nephrology Department, Hamed Al-Essa Organ Transplant Center, Ibn Sina Hospital, Sabah Area, Kuwait. amabbaas@zu.edu.eg (Ahmad Abbas),
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
The first defense line of the battle, healthcare workers (HCWs), faces a significant challenge in managing the current COVID-19 pandemic. An online electronic survey was sent to HCWs via email and social media networks. Socio-demographic data and work environment-related variables were assessed. Consequences of burnout (BO) were reported, e.g., elicited medical errors. Maslach burnout inventory was used to diagnose BO. Two hundred and eighty-four participants were included with a mean age of 39.83 ± 7.34 years, 70.8% worked in the COVID-19 frontline, 91.9% were followed daily updates about COVID-19, 63.7% were not satisfied with the coordination between triage and isolation, 64.4% got COVID-19 infection, 91.9% had a colleague or family member developed COVID-19 infection, and 21.5% experienced a colleague /a family member died due to COVID-19. Multivariate analysis by linear regression revealed that; working as a frontline HCW (OR 1.28, CI = 0.14–2.55) and sleep deprivation (OR 3.93, CI = 1.88–8.22) were the predictors of burnout.
Keywords
Burnout
COVID-19
Maslach Inventory
Medical errors
- CI
-
Confidence interval
Abbreviations
1 Introduction
In March 2020, the World Health Organization declared Corona Virus Disease 19 (COVID-19) to be a pandemic. It spread worldwide with >600 million documented cases and 6 million deaths till October 2022. This new pandemic has a broad spectrum of unpredictable presentations ranging from asymptomatic or mild illness up to acute diseases necessitating ICU and mechanical ventilation (Gheith et al., 2020; Singhal, 2020; Baud et al., 2020).
In the first defense line of the battle-healthcare workers (HCWs)- faces a significant challenge in managing the current pandemic. Beyond the stress on them regarding rapid decision-making for proper assessment and treatment, the risk of exposure to infected cases, getting the disease, and transmitting it to their family is also another concern.
Moreover, the catastrophic burden on the medical system that consumes all medical and human resources up to collapse was never witnessed and translated into negative affection on physical and mental well-being (Anon., 2019; Tsamakis et al., 2020; Abbas et al., 2021).
The condition known as Burnout syndrome (BOS) is brought on by ongoing, chronic stress at work. Between 50 and 70% of BOS cases were recorded in research conducted before the current pandemic. Emergency and critical care sectors, especially in times of pandemics, are at higher risk of BO. Unique work environments with loaded schedules, managing of critically ill patients with higher rated of mortality expected, and disrupted socio-familial relationships are often accused (Abbas et al., 2019; Rothenberger, 2017; Clough et al., 2017).
The objective of our work was to determine the frequency of BO between HCWs and to clarify its determinants, predictors, and negative impacts on the quality of medical service.
2 Material and methods
A cross-sectional study of HCWs registered with the Ministry of Health was conducted from January 2022 to June 2022. This work included HCWs who were on duty and agreed to participate during the period of the study, while who were employed for less than six months, on vacation, incomplete answers, or refused to participate were excluded.
2.1 Sample size
Using Epi Info, developed by CDC, (Atlanta, Georgia, US), 2002 and based on the expected frequency of BO (13%) (Wu et al., 2020), a 95% level of significance of, power of the study (80%), and a 5% error, the sample size was calculated to be 225.
2.2 Data collection tool
An online electronic survey (in English) using Google forms was prepared and sent to HCWs through email and social media networks. We attained ethical approval from the Research Ethics Committee of the MOH. The study was conducted after approval from Ministry of Health Ethical Committee and under the Declaration of Helsinki guidance on human research.
It includes:
-
Socio-demographic and profession-related data: age, gender, marital state, years of experience, comorbidities, and relation to COVID-19 (frontline or behind-line).
-
Work environment-related variables: can choose day off, satisfaction with resources, conflicts with patients/relatives, sleep deprivation, increased work hours after COVID-19, and appreciation state.
-
COVID-19 related variables: following daily news updates, satisfaction with resources, therapeutic protocols, doing swabs, had been infected with COVID-19, relative/colleague got infected or died with COVID-19 and daily COVID-19 mortality in the work area.
-
Consequences of BOS were reported: start smoking or increased number of cigarettes, suicidal thoughts, nervousness, medical errors, no check for drug allergy, incorrect dose or over dosage, and alternating medications between patients.
-
Maslach burnout inventory to diagnose Burnout.
A 22 items with a scale from (0) never to (6) every day representing the three dimensions of BO; Depersonalization (DP (, Emotional exhaustion (EE(, and the loss of professional accomplishment (AP).
For each dimension, the score is 'low,' moderate, or high. For EE, the mild level is defined as a score between 0 and 18, the moderate level (19–26), and the high level (≥27). For DP, low mild is defined as a score between 0 and 5, moderate (6–9), and high level (≥10). For PA, the mild level is defined as a score ≥ 40, the moderate level (34–39), and the high level (0–33).
A high score in EE and DP or a low score in AP is diagnostic of. The degree of BO is low, moderate or high according to the number of dimensions affected (Abbas et al., 2019; Wu et al., 2020; Maslach et al., 1996; Sabbah et al., 2012).
2.3 Statistical analysis
SPSS 22.0 for Windows was used to conduct the statistics (SPSS Inc., Chicago, Illinois, USA). The Shapiro-Wilk test was used for determining the normality of continuous variables, which were abridged as mean SD. The categorial variables were expressed numerically (%). The Chi-square test and independent t-test were used to assess the relationships between burnout and other factors. To evaluate the link between various variables, Spearman's rank correlation coefficient was used. To detect predictors for BOS, we built a univariate binary logistic model; then, we used a significant variable to build an unadjusted multivariate model. Finally, we built an adjusted multivariate model by adjusting by insignificant variables. For each variable, we reported Odds Ratio (OR) and corresponding 95%CI and also p-value. All tests were two-sided, and a P value was set at <0.05.
3 Results
3.1 Socio-demographic and profession-related data:
Two hundred and eighty-four participants had completed the survey. Their mean age was 39.83 ± 7.34 years, 66.9% were males, 61.3% were registrars, and 68.3% had more than ten years of experience. Most respondents were ≤ 40 years (64.8%) married (72.5%). Overall, 70.8% of them worked as COVID-19 frontline, and nearly half of them had co-morbid diseases (47.5%). The frequency of burnout reported was 48.2%, Table 1 and Fig. 1.
Variables
All (N = 284)
No.
(%)
Sex
Male
190
66.9
Female
94
33.1
Age (years)
Mean ± SD
39.83 ± 7.34
≤40 years
184
64.8
>40 years
100
35.2
Marital status
Single
40
14.1
Married
206
72.5
Widow/divorced
38
13.4
Job Title
Registrar
174
61.3
Senior registrar/specialist
88
30.9
Consultant
22
7.7
Type
Front-line
201
70.8
Behind-line
83
29.2
Experience (years)
≤5 years
36
12.7
6–10 years
54
19
>10 years
194
68.3
No
48
16.9
Comorbidity
Yes
135
47.5
No
149
52.5
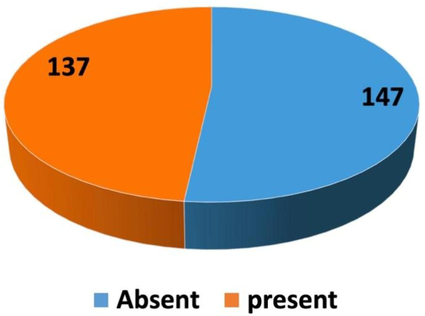
Frequency of Burnout in the studied population.
3.2 Work environment-related variables.
83.1% of the study participants reported they increased their working hours after COVID-19. Most of them had conflicts with either patients or their relatives, (75.4%) couldn‘t choose their days-off (88.4%), (20.1%) were not satisfied with resources, (76.4%) experienced sleep deprivation, and (70.8%) felt unappreciated, Table 2.
Variables
All (N = 284)
No.
(%)
Can choose day off
Yes
33
11.6
No
251
88.4
Satisfaction with resources
Yes
227
79.9
No
57
20.1
Conflict with patients/relatives
Yes
214
75.4
No
70
24.6
Sleep deprivation
Yes
217
76.4
No
67
23.6
Unappreciated
Yes
201
70.8
No
83
29.1
Increased work hours after COVID-19
Yes
236
83.1
No
48
16.9
3.3 COVID-19 related variables
Table 3 also, highlights COVID-19-related variables among studied participants in which 91.9% were followed daily COVID-19 updates, and 63.7% were not satisfied with the triage/isolation coordination. Moreover, 14.4% of participants were doing swabs for suspected COVID-19 patients, 64.4% got COVID-19 infection, 91.9% had a colleague/family got COVID-19 infection, and 21.5% experienced a colleague, or a family member died due to COVID-19, Table 3.
Variables
All (N = 284)
No.
(%)
Following daily COVID-19 news updates
Yes
261
91.9
No
23
8.1
Unsatisfied with coordination between triage and isolation
Yes
181
63.7
No
103
36.3
Doing swabs
Yes
41
14.4
No
243
85.6
Got infected with COVID-19
Yes
183
64.4
No
101
35.6
Colleague/relative got infected with COVID-19
Yes
261
91.9
No
23
8.1
Colleague /relative died with COVID-19
Yes
61
21.5
No
223
78.5
3.4 Levels of BO
As shown in Fig. 2, 53.3% of study participants had high EE domain score, 43.1% had high DP domain score and 30.7% had high reduced PA score. Moreover one-third of the study population had a severe type of BO predictors, according to the total BO score.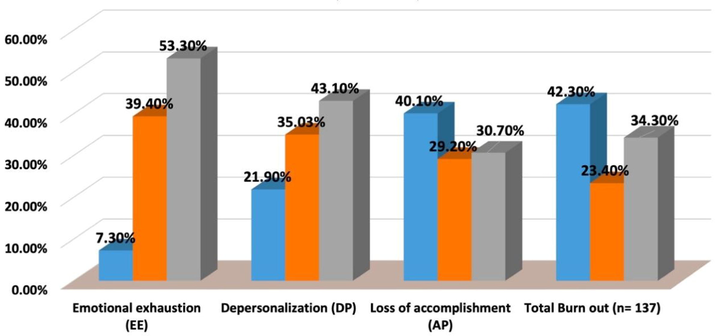
Severity of BOS domains among participants with Burnout (n = 137).
Multivariate analysis of predictors of BO was tested in Table 4, by linear regression and reported that; working as a frontline HCW (OR 1.28, CI = 0.14–2.55) and sleep deprivation (OR 3.93, CI = 1.88–8.22) were the predictors of Burnout. Both predictors were valid in both adjusted and non-adjusted models.
Variable Type
Univariate analysis
Unadjusted multivariate analysis
Adjusted multivariate analysis
P
OR (95% CI)
P
AOR (95% CI)
P
Type (frontline)
5.31 (2.96–9.54)
<0.001
0.33(0.17–0.62)
0.001
1.28(0.14–2.55)
<0.001
Age
0.97 (0.95–1.02)
0.47
1.02 (0.96–1.07)
0.45
Sex (male)
0.88 (0.54–1.44)
0.61
0.82(0.46–1.45)
0.49
Marital state
Single
1.11 (0.56–2.18)
0.78
0.93(0.42–2.03)
0.85
Married
1.23 (0.51–2.99)
0.65
1.30(0.47–3.61)
0.61
Experience (years)
≤5 years
1.04 (0.45–2.42)
0.93
1.11(0.43–2.88)
0.83
6–10 years
0.84 (0.41–1.72)
0.63
0.8(0.3–2.14)
0.0.65
Comorbidity (yes)
0.87 (0.55–1.38)
0.55
0.72(0.42–1.22)
0.22
Sleep deprivation (yes)
6.27 (3.23–12.17)
<0.001
3.92 (1.92–8.01)
<0.001
3.93(1.88–8.22)
<0.001
Unappreciated (yes)
1.8(1.07–3.02)
0.03
1.33(0.73–2.4)
0.349
1.37(0.74–2.52)
0.32
Increased work hours after COVID-19 (yes)
1.22 (0.66–2.28)
0.53
1.86(0.90–3.84)
0.09
Following daily COVID-19 news updates (yes)
0.75 (0.32–1.78)
0.52
0.89(0.33–2.42)
0.82
Unsatisfied with coordination between triage and isolation (yes)
1.28 (0.79–2.08)
0.32
1.3(0.74–2.23)
0.36
Got infected with COVID-19 (yes)
1.17 (0.72–1.9)
0.54
0.82(0.46–1.45)
0.49
Colleague or relative got infected with COVID-19 (yes)
0.75 (0.32–1.76)
0.52
0.73(0.27–1.97)
0.54
Colleague or relative died with COVID-19 (yes)
2.07 (1.15–3.71)
0.015
1.570(0.83–2.97)
0.168
1.65(0.83–3.26)
0.15
3.5 Consequences of burnout
Deleterious effects of Burnout on HCWs were shown in Fig. 3. The largest proportion of the studied population denied smoking initiation after the pandemic without any suicidal thoughts or attempts. On the other hand, 21.5% of the respondents treated patients/relatives nervously and accused perform medical faults as follows; no check for drug allergy (8.5%), incorrect dosing or over dosage (29%), wrong explanation of the drug usage (20.1%) and prescribing medication to the wrong patient (6.3%).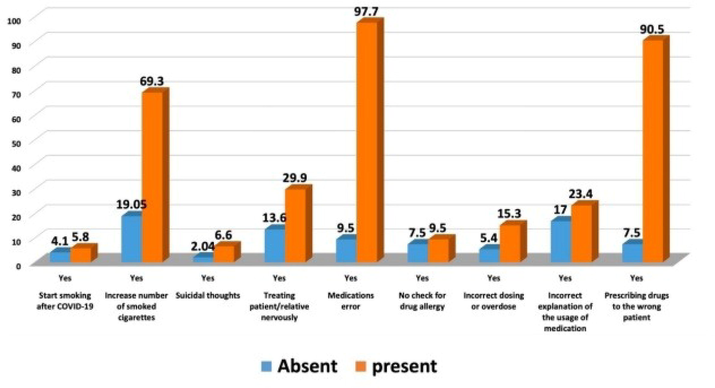
Consequences of Burnout Syndrome.
HCWs with Burnout -compared to those without Burnout- had experienced an increased number of daily smoked cigarettes (p < 0.001), treated patients/relatives nervously, accused of medical errors (P = 0.001) and incorrect or overdosing (p = 0.006).
4 Discussion
The entire healthcare system is negatively impacted by the COVID-19 pandemic. The impact on health care workers is increasing not only because of increased workload, but also because of fear of being diseased especially with limited personal protective equipment, fear of transmitting infections to their families, caring for patients who are quickly deteriorating and were diseased with a virus that doesn’t have obvious curative treatment and providing medical attention to sick coworkers (Albott et al., 2020; Senni, 2020; Walton et al., 2020; Chirico et al., 2020; Lotfy et al., 2021).
Our study findings were nearly similar to Duarte et al. (Duarte et al., 2020), in which their participants had mean age was 38 ± 10 years, and 37.8% had more than ten years of experience. Most respondents were ≤40 years married (53.3%) and 69.7% of them worked as COVID-19 frontline, and 26.1% had comorbid diseases.
Also, the current study goes hand in hand with Lasalvia et al. (Lasalvia et al., 2021), who reported that 59.6% of the sample said they were required to perform tasks they were typically not supposed to, 65.3% had an increase in workload, and 50% of the sample perceived more disputes between coworkers. Regarding the perception of risk, 66.5% of HCW who were caring for COVID-19 patients, said they felt anxious, and 82.8% said they were frightened of getting severe acute respiratory syndrome coronavirus 2.
The results show that 52.2 percent of people had high EE scores, 43.3 percent had high DP scores, and 34.5 percent had substantial levels of reduced personal accomplishment. Moreover one-third of the participants reported a significant level of burnout based on their overall score.
This result was in line with that of Lasalvia et al. (2021), who found that overall, 38.3% of their participants showed signs of high emotional exhaustion (EE), low professional efficacy (EF) (46.5%), and high cynicism (26.5%). These results also coincide with Chen et al. (2021), who revealed that the indicators of lack of personal success are reverse-coded; persons with scores of 0–33, 34–39, and ≥40 show, respectively, low, moderate, and high levels of this problem.
In a review article on burnout among middle eastern health care workers, resident physicians undergoing training in the United Arab Emirates (N = 302) expressed 70% overall burnout, 75.5% moderate-to-high emotional tiredness, 84% high depersonalization, and 74% a weakened sense of personal success (Chemali et al., 2019).
In Saudi Arabia, Agha et al. found that the prevalence of recorded high emotional exhaustion, high depersonalization, and reduced personal exhaustion among doctors working in a tertiary care hospital (N = 96) was 68.8, 63.6, and 38.5 percent, respectively (Agha et al., 2015).
In Egypt, another study found that 68.2 percent of the participants had moderate burnout. In addition, compared to doctors, nurses displayed higher degrees of emotional weariness and depersonalization (Abbas et al., 2019).
Our multivariate analysis by linear regression revealed that; working as a frontline HCW (OR 1.28, CI = 0.14–2.55) and sleep deprivation (OR 3.93, CI = 1.88–8.22) were the predictors of Burnout.
Working with patients who have COVID-19 in frontline settings, a lower risk of emotional tiredness was noticed in non-COVID wards (0.53; 95% CI 0.37–0.77) and the administration (0.53; 95% CI 0.29–0.96) than working in intensive care units, according to adjusted ORs from Italy (Lasalvia et al., 2021).
An Egyptian study found that lack of sleep in resident physician besides feeling unappreciated, were all significant predictors of burnout (Abbas et al., 2019).
According to a Saudi Arabian study, the number of patients seen each day, the amount of paperwork completed, the flow of unorganized patients into clinics, and patient violence were all positive predictors of burnout. (Bawakid et al., 2017).
According to Abdelhafiz et al., while female gender exhibited a strong correlation with higher EE, males were predictors of DP. Furthermore, there was a strong correlation between elevated EE and reduced PA in cases of COVID-19 infection or death in coworkers or family, respectively (Abdelhafiz et al., 2020).
Deleterious effects of Burnout on HCWs showed that most study participants denied having suicidal intentions, starting smoking after COVID-19. On the other hand, 21.5 percent of respondents were nervous when treating patients/relatives and were accused of making medical errors such as not checking for drug allergies (8.5 percent), incorrect dosing or overdosing (29 percent), incorrect explanation of medication usage (20.1%), and prescribing medication to the wrong patient (6.3 percent). HCWs with Burnout (compared to those without Burnout) had experienced the following: increased number of daily smoked cigarettes (p < 0.001), treated patients /relatives nervously, accused of medical errors (P = 0.001), and incorrect or overdosing (p = 0.006).
According to one study, stress is a risk factor for burnout as well. Severe stress can cause mental exhaustion, trouble concentrating, loss of short-term memory, and anxiety, among other serious effects on a person's health. In a randomized controlled experiment, stress management program and burnout prevention were found to be beneficial, the program intended to reduce existing stress levels while also giving stress management skills. Stress management abilities should be improved as much as possible (Stier-Jarmer et al., 2016).
The current study has a number of limitations. First, the study's design (cross-sectional) makes it difficult to assess different time intervals. Second, subjectivity of perception may have influenced the assessment of Maslach burnout inventory variables, resulting in study variability. Additional research is needed to standardize the tool that is used to assess BO. Eventually, the impact of nursing experience and workload, as well as other characteristics like depression and anxiety, that may be related to burnout and have an impact on the performance of the medical team, were not taken into consideration.
However, studies on physician burnout have raised awareness of the critical nature of professional mental health and wellbeing. Recently, US national organizations demanded that all healthcare systems evaluate their doctors' well-being, frequently with a focus on burnout (Perlis, 2020). Based on what we know, this is the first study to have examined Burnout among HCWs during the current pandemic, reported its frequency and risk factors, and evaluated its impact on the performance of the medical team with regard to medical errors and hazards.
5 Conclusion
In conclusion, during the COVID-19 pandemic in Kuwait, this nationwide online survey disclosed a high frequency of Burnout among HCWs, which had a detrimental impact on medical errors made. Burnout was predicted by working as a frontline HCW (OR 1.28, CI = 0.14–2.55) and sleep deprivation (OR 3.93, CI = 1.88–8.22).
Funding
The authors extend their appreciation to the Researchers Supporting Project number (RSP2022R418), King Saud University, Riyadh, Saudi Arabia.
Institutional Review Board Statement
Ethical approval was obtained from the Research Ethics Committee, Ministry of Health, Kuwait. (Number of acceptances 1871/2021).
Informed Consent Statement
Consent to participate was the first question and answering “yes” was mandatory.
CRediT authorship contribution statement
Torki Al-Otaibi: Resources, Supervision, Conceptualization. Ahmad Abbas: . Osama Ashry Gheith: Resources, Supervision, Conceptualization. Prasad Nair: Supervision. Mohamed A. Zahab: . Mryhan A.A. Hammouda: . Mahmoud M. Farid: Resources. Reem M. Aljowaie: Conceptualization. Noorah A. AlKubaisi: Conceptualization. Eman Fouad Mohamed: . Arshad Mehmood Abassi: Supervision. Yasmine H. Eisa: Resources, Conceptualization.
Acknowledgments
We would like to acknowledge staff members of Hamed Al-Essa organ transplant center and MOH hospitals, who suffered a lot during the COVID-19 pandemic. This paper is wholehearted to them, as their dynamic share to knowledge about COVID-19 made it possible.
Sample availability
Samples of the compounds ... are available from the authors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Prevalence, associated factors, and consequences of Burnout among ICU healthcare workers: An Egyptian experience. Egypt. J. Chest Dis. Tuberc.. 2019;68(4):514-525.
- [Google Scholar]
- Sleep Quality Among Healthcare Workers During the COVID-19 Pandemic and Its Impact on Medical Errors: Kuwait Experience. Turk. Thorac. J.. 2021;22(2):142-148.
- [CrossRef] [Google Scholar]
- Prevalence, Associated Factors, and Consequences of Burnout Among Egyptian Physicians During COVID-19 Pandemic. Front. Pub. Health. 2020;8:590190
- [CrossRef] [Google Scholar]
- Burnout among middle-grade doctors of tertiary care hospital in Saudi Arabia. Work (Reading, Mass.). 2015;51(4):839-847.
- [CrossRef] [Google Scholar]
- Battle Buddies: Rapid Deployment of a Psychological Resilience Intervention for Health Care Workers During the COVID-19 Pandemic. Anesth. Analg.. 2020;131(1):43-54.
- [CrossRef] [Google Scholar]
- Anon., 2019. Health workforce burn-out. Bull. World Health Organ. 97(9), 585–586. https://doi.org/10.2471/BLT.19.020919.
- Real estimates of mortality following COVID-19 infection. Lancet Infect. Dis.. 2020;20(7):773.
- [CrossRef] [Google Scholar]
- Burnout of Physicians Working in Primary Health Care Centers under Ministry of Health Jeddah, Saudi Arabia. Cureus. 2017;9(11):e1877.
- [Google Scholar]
- Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Public Health. 2019;19(1):1337.
- [CrossRef] [Google Scholar]
- A Large-Scale Survey on Trauma, Burnout, and Posttraumatic Growth among Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs.. 2021;30(1):102-116.
- [CrossRef] [Google Scholar]
- Protecting the mental health of healthcare workers during the COVID-19 emergency. B. J. Psych. Int. 2020:1-6.
- [Google Scholar]
- (Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst. Rev.. 2017;6(1):144.
- [CrossRef] [Google Scholar]
- Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health. 2020;20(1):1885.
- [CrossRef] [Google Scholar]
- Coronavirus 2019 pandemic and renal diseases: a review of the literature. J. Egypt. Soc. Nephrol. Transplant.. 2020;20(4):191-203.
- [Google Scholar]
- Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1):e045127.
- [Google Scholar]
- Use of Hydroxychloroquine in Patients with COVID-19: A Retrospective Observational Study. Turk. Thorac. J.. 2021;22(1):62-66.
- [CrossRef] [Google Scholar]
- Maslach Burnout Inventory manual (3rd ed.). Palo Alto.; CA: Consulting Psychologist Press; 1996.
- Exercising Heart and Head in Managing Coronavirus Disease 2019 in Wuhan. JAMA Netw. Open. 2020;3(3):e204006.
- [Google Scholar]
- Physician Burnout and Well-Being: A Systematic Review and Framework for Action. Dis. Colon Rectum. 2017;60(6):567-576.
- [CrossRef] [Google Scholar]
- Burnout among Lebanese nurses: psychometric properties of the Maslach burnout inventory-human services survey (MBI-HSS) Health. 2012;4:644-652.
- [Google Scholar]
- COVID-19 experience in Bergamo, Italy. Eur. Heart J.. 2020;41(19):1783-1784.
- [CrossRef] [Google Scholar]
- A Review of Coronavirus Disease-2019 (COVID-19) Indian J. Pediatr.. 2020;87(4):281-286.
- [CrossRef] [Google Scholar]
- The Effectiveness of a Stress Reduction and Burnout Prevention Program. Deut. Arzt. Int.. 2016;113(46):781-788.
- [CrossRef] [Google Scholar]
- COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp. Ther. Med.. 2020;19(6):3451-3453.
- [CrossRef] [Google Scholar]
- Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc.. 2020;9(3):241-247.
- [CrossRef] [Google Scholar]
- A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J. Pain Symptom Manag.. 2020;60(1):e60-e65.
- [CrossRef] [Google Scholar]
Appendix A
Supplementary material
Supplementary material to this article can be found online at https://doi.org/10.1016/j.jksus.2022.102441.
Appendix A
Supplementary material
The following are the Supplementary material to this article:







