Translate this page into:
The frequency spectrum of the acoustic environment in a neonatal intensive care unit
⁎Corresponding author at: Acoustic Engineering Laboratory, CASEM Building, Puerto Real Campus, Cadiz University, Avda of the University of Cádiz s / n, 11515 Puerto Real, Cádiz, Spain. ricardo.hernandez@uca.es (Ricardo Hernández-Molina)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Objectives
The acoustic frequencies present in an incubator are within the hearing range of a newborn; this requires adapting the environment so that the noise inside the incubator is more compatible with that range and facilitates proper hearing development. The objective of this study is to make a comparison, in thirds of an octave (frequency analysis), of the noise present in the NICU room and the interior space of the incubator, analyzing the ambient acoustic quality perceived by the newborn.
Methods
The experiment carried out in this work consisted of two series of measurements of noise levels in the NICU of the “Puerta del Mar” University Hospital (Cádiz, Spain) and two selected incubators in the room. A third-octave frequency band analysis was performed within the audible field (20 Hz/20 kHz). Data were recorded at 1 s intervals for more than 24 h (3600 registers de 1 s.)
Results and conclusions
One may wonder if noise levels inside incubators affect newborns. Based on existing references, the answer is probably “yes”, since the frequencies present inside an incubator are within the audible range of a newborn. According to the consulted bibliography, the audible range of neonates is between 400 Hz and 4 kHz. In this work, the acoustic measurements carried out in the NICU made it possible to evaluate the noise levels in the room and inside the incubators. According to the results, the indicator used LAeq, 1 h, should be complemented with a study in 1/3 octave bands (frequency analysis) to determine the acoustic quality and hearing protection of neonates.
Keywords
Newborn
Intensive care units
Neonatal
Noise
Hearing
Pediatrics
1 Introduction
In recent times, the rate of premature births has grown steadily owing to several factors including an increase in the mother’s age, assisted reproduction, multifetal pregnancies, premature membrane breakage, bacterial infections, and other medical recommendations, such as preeclampsia (Ananth and Vintzileos, 2006). Premature births have been estimated to account for 75–80% of all perinatal deaths (Ovalle et al., 2012), of which 40% o occur within the first 32 weeks of pregnancy (Goldenberg, 2001).
Although advanced care increases the chances of survival in neonatal intensive care units (NICUs), there is growing concern about the overstimulation that newborns are subjected to in these wards. Overstimulation of a newborn’s immature system produces stress that results in disproportionate energy expenditure and may affect curing, recovery, and growth-related processes (Ananth and Vintzileos, 2006). Stress in this scenario originates mainly from ambient light and noise, tactile and stimulative handling, and care of the neonates (Peng et al., 2014). Noise exposure is a necessary, continuous form of sensory stimulation for premature neonates and one that is thus ordinarily included in interventions for this type of patient (Krueger et al., 2012). Excessive noise and especially tonal noise, impulsive noise, and noise events cause harmful effects on human health, especially on newborns. So harmful as to result in stress-derived functional disorder high noise levels can not only lead to hearing losses in neonates (Stennert et al., 1977) but also lower mean blood pressure (Slevin et al., 2000), increase heart and breathing rate, decrease oxygen saturation (Bremmer et al., 2003) and impair the self-regulatory capacity of newborns (Shimizu and Matsuo, 2016). Also, the mid and long-term effects of cyclical stimulation with high sound pressure levels can have psychological impacts with behavioral consequences (Trapanotto et al., 2004).
Although a quiet hospital is impossible, reducing current noise levels to acceptable levels is essential to ensure that patients do well (Cardoso et al., 2015) and especially neonates, who are still immature and more vulnerable to the adverse effects of noise. Clinical practice has shown that reducing some stimuli such as noise, light, odors, handling, pain, and inappropriate positions can alleviate neurological damage and ease the development of a more robust central nervous system in neonates (Gascón Gracia and García Berman, 2011).
Fetuses in their mothers’ wombs have the advantage over neonates in incubators where the former are surrounded by amniotic fluid and abdomen tissues —two efficient attenuators of external noise. It should be noted that womb inner structures substantially reduce sound pressure levels at frequencies above 500 Hz. For example, animal experiments conducted by Gerhardt and Abrams showed that a 72 dB signal at 500 Hz was reduced by 24 dB, while others at higher frequencies were reduced more markedly (by 38 dB at 1000 Hz and 48 dB in 2000–4000 Hz). These layers can filter out a great part of the high-frequency sound energy, in fact, they work as a low-pass filter that allows fetuses to hear only low-frequency sounds (Abdollahi et al., 2017). About the range of sound frequencies to which the neonate is sensitive, and given the difficulty of the investigation, there is a significant disparity in the results of some authors. According to Gerhardt et al., a 27-week-old fetus can only hear low-frequency sounds (below 500 Hz) and takes two more weeks to sense frequencies above 500 Hz (Gerhardt et al., 2000). A study carried out by Hepper and Shahidullah (Hepper, 1994), agrees with Gerhardt et al., in locating the cutoff frequency of hearing for 19 to 27-week-old fetuses in 500 Hz. Furthermore, Lahav A et al., agree to locate hearing sensitivity above 1000 Hz after 33 weeks of pregnancy (Lahav, 2015). However, Avery et al., claimed that the hearing sensitivity range of a fetus in the third term of pregnancy is 500 to 1000 Hz and that of a full-term newborn is 400 to 4000 Hz (Avery et al., 2001). Precisely for this reason, Harrison focuses his concern on exposure to high-frequency noise doses (>800 Hz) during this stage in which the auditory system of premature infants is not yet fully developed (Harrison et al., 2004).
According to the American Academy of Pediatrics (AAP), noise levels above 45 dBA can cause cochlear damage or even arrest normal development in neonates (AAP, 1997). Several authors have concluded that exposure to high noise levels can affect neural development by favoring unwanted neural pathways and placing neonates under the task of hearing disorders and learning disabilities in the future (Neille et al., 2014). Although these disorders are also seen in infants with normal hearing thresholds, they are more frequently found in preterm children (Kurtzberg et al., 1988). Noise damage essentially depends on objective factors such as frequency, sound pressure level, exposure time, and rest period (Morata and Santos, 1996).
Regarding the recommended noise for indoor hospitals, the US-EPA suggests that Ldn = 45 dB (the day-night weighted noise indicator as defined in ISO-1996:1) should not be exceeded (US-EPA, 1974; Knutson, 2012), since the goal is to protect patients’ public health and well-being. The AAP recommends that the LAeq,1h, resulting from the combination of continuous and transient noise in neonatal care areas not exceed 45 dB. In addition, other recommendations suggest that LAF10,1h = 50 dB should not exceed, and LAFmax = 65 dB must never be exceeded (AIA, 2001; White, 2006).
Reducing noise levels in a NICU is rather difficult owing to the considerable number and variety of sources contributing to its acoustic environment. The main factor to be considered in developing effective solutions here is the NICU structure (physical design). The Spanish Pediatric Association has issued some recommendations about room space and placement of NICUs in hospital buildings to ease the right development of premature neonates (Agra Varela et al., 2014).
Other noise problems can originate from a variety of factors such as room size and conditioning, and the presence of specific noise sources (Naresh, 2003). The catalog of noise sources at NICUs comprises monitor alarms, support equipment, HVAC systems (heating, ventilation, and air conditioning), phones, and health staff activities (Hernandez Molina et al., 2018). Other sources of noise to consider include the implementation of recent technologies such as those of motorized toilet paper, towel dispensers, or hand dryers can raise noise levels rather than lower those (Brandon et al., 2008).
All of this serves as justification for this work that aims to characterize the levels and spectral composition of the total noise present in a NICU room and inside two different incubators and using scientific evidence, determine if these levels are compatible with the proper auditory development of preterm infants.
2 Materials and methods
To carry out the work, a test was designed in the NICU of the “Puerta del Mar” University Hospital (Cádiz, Spain). This test consisted of two series of noise measurements carried out simultaneously over 24 h. For health reasons, and to exclude neonate-generated noise, the two target incubators were empty but working in normal conditions. To do so, two sound level meters were used. The first one is a Brüel & Kjaer 2270 and the other is a B&K 2250 [https://bitly.ws/ykxX]. The Extended Sound Analysis Software B&K BZ-7225 used in both equipment allows the logging of all broadband parameters and spectra. Both sound level meters meet the requirements of a type 1 instrument, as defined by the International Electrotechnical Commission, EN-IEC 61672-1:2013. To verify the proper functioning of the equipment a Sound Calibrator B&K 4231 was used. The data was downloaded and later analyzed using the software from the same manufacturer, the B&K 7820 (Evaluator) [https://bitly.ws/yb53].
The microphone of the B&K 2250 was placed inside the two empty analyzed incubators to assess the influence of noise on the neonates. In this way, it becomes possible to show the noise exposure of a neonate inside the incubator, despite the potential noise absorption or reflection by the incubator panels. For this purpose, the microphone was mounted on a small tripod that was placed on the mattress, approximately 10 cm above the area where the neonate’s head would rest (Fig. 1).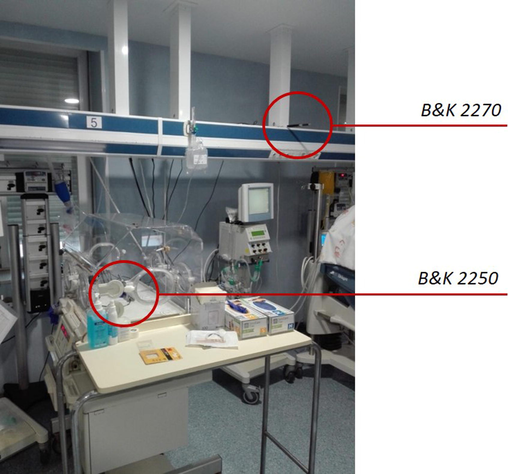
Positioning of microphones in the NICU.
The incubator studied in the first set of measurements was an Ohmeda Medical Giraffe Omni Bed (Giraffe) [https://bitly.ws/yhku]. This incubator is situated at one end of the room away from the staff worktable (Fig. 2). The incubator studied in the second measurement series was an Ohmeda Medical Ohio Care Plus 3000 model (OCP 3000) [https://bitly.ws/yhm4]. In this case, the incubator was located in the main area of the room near the staff’s workbench. The number of occupied incubators increased from 7 in the first measurement series to 9 in the second. Both incubators are from the same manufacturer Avante Medical Surgical https://www.dremed.com/.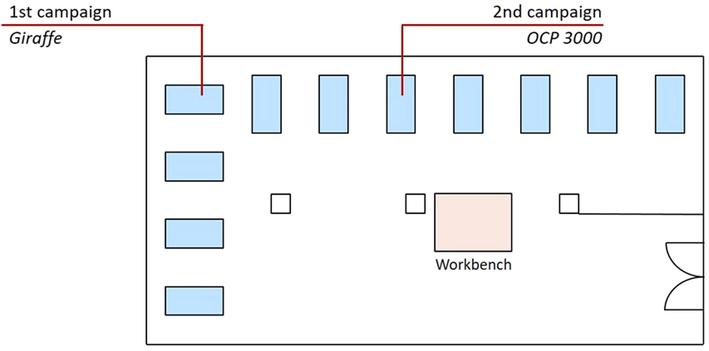
Positioning of microphones in the NICU.
During both campaigns, the B&K 2270 that defines the noise inside the NICU is placed in the same location (Fig. 1), which is chosen because it has a clear view of the room and is located more than 1.5 m from the wall and the nearest ceiling.
The main parameter collected were the wide band A-weighted and unweighted continuous equivalent sound pressure levels (LAeq and LZeq), and the 1/3 octave noise spectra from 12.5 to 20 000 Hz (LAeq). The frequency spectrum has been measured in A-weighting so that the assessment can be made according to the AAP. The rest of the parameters are the maximum and minimum response-weighted levels (LAFmax and LAFmin, respectively), the impulse-weighted levels (LAIeq), and the C-weighted peak levels (LCpeak). These two noise indices have been selected to monitor if there are any high-energy sound events in the room. All these noise descriptors have been measured and stored every second during the total measurement time (24 h). Therefore, 4 (time) series of the mentioned noise parameters have been generated, with a length of at least 86,400 data per series. The B&K 2270 was also programmed to make audio recordings during the measurement period to reveal the cause of certain sound events.
3 Results
3.1 Noise inside the NICU
During the first round of measurements, the LAeq,24h value was 60.0 dB and LCpeak was 109.0 dB, however, during the second round the LAeq,24h value experienced an increase to reach 63.8 dB, while the value of LCpeak remains at similar values of 109.1 dB. Fig. 3 shows the evolution of the sound pressure levels collected second by second during the 24 h of the second test. As can be seen, the ambient noise in the NICU during this test ranged from LAeq,1s = 45.2 to 66.3 dB. The comparison of the 24-hour frequency spectrum between the two measurement campaigns can be seen in Fig. 4.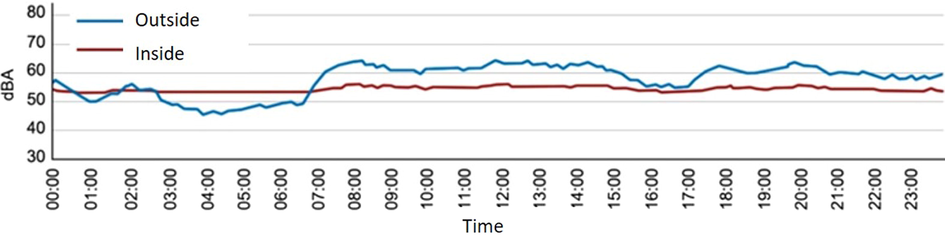
The time series shows the evolution during 24 h of the LAeq,1s, inside and outside the Giraffe incubator at the NICU of the Puerta del Mar University Hospital, in Cádiz.
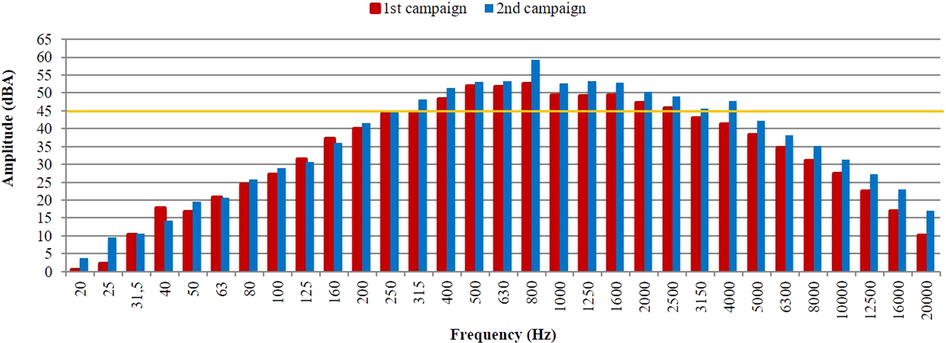
Comparison of the frequency spectra recorded in the two NICU measurement series.
3.2 The noise inside the incubators
Sound pressure levels in the first round of noise measurements (inside Giraffe) ranged from LAFmax = 84.2 dB and LAFmin = 44.2 dB. The LAeq,24h value was 50.4 dB, and LCpeak also reaches high values close to 108.3 dB. As can be seen in Fig. 5, most of the noise energy is concentrated between the frequencies 100 Hz to 1.6 kHz. Sound pressure levels in the second round of noise measurements (inside OCP 3000) ranged from LAFmin = 54.5 dB to LAFmax = 86.8 dB, being the LAeq,24h of 58.5 dB, and the LCpeak was 104.4 dB. As can be seen in Fig. 6, most of the noise energy is concentrated in a wider frequency range than in the previous case (from 80 Hz to 8 kHz).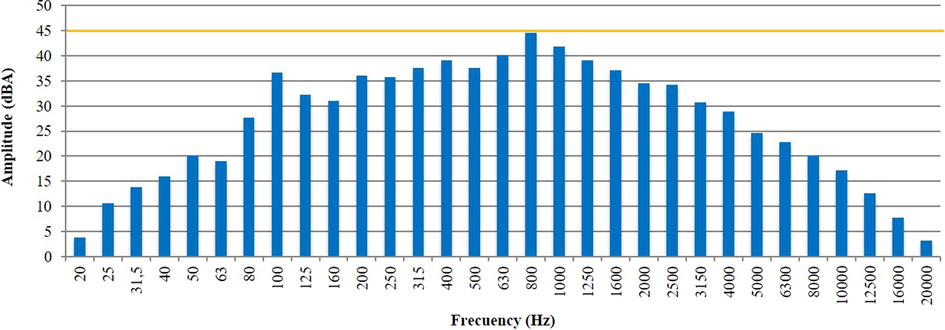
The total frequency spectrum of noise levels inside the Giraffe incubator during the 24 h of the 1st measurements campaign.
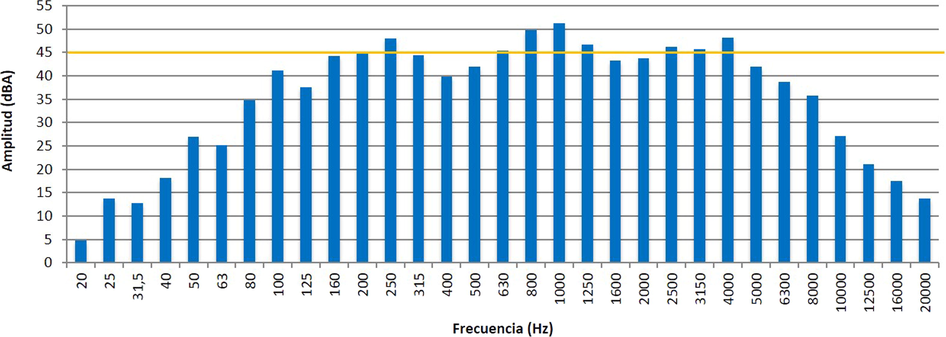
The total frequency spectrum of noise levels inside the OCP 3000 incubator during the 24 h of the 2nd measurements campaign.
4 Discussion
Measurements in the second campaign exceeded those in the first. This was largely the result of the greater number of neonates present in the NICU —and hence of the also greater number of items of electrical and medical equipment running in the NICU, and of the higher volume needed by the staff to communicate— in the second. The cause that contributed the most to the noise dose inside the room (LAeq,24h) was conversations in the NICU which agrees with other studies (Jonckheer et al., 2004), while the highest energy sound peaks (LCpeak) were reached by sporadic events, such as falling objects.
As can be seen from Fig. 3, noise levels invariably exceeded the recommended limit (LAeq,1s = 45 dB). If the examination is carried out in bands of thirds of an octave, it becomes clear that it is the medium frequency bands that contribute to causing this negative situation (Fig. 4).
4.1 Are neonates inside incubators exposed to excessive noise levels?
This is the main question addressed in this work. Although the cover of an incubator can attenuate noise by LpA = 10–12 dB, this reduction is downgraded, especially in the mid-and high-frequency range (Fernández Zacarías et al., 2018), by inner noise from the fan motor used to adjust the temperature and relative humidity in the incubator. A comparison of the frequency spectrum for the NICU room and the incubator inner space of the OCP 3000 (Fig. 7), reveals that the sound pressure level in the low-frequency band (20–250 Hz) was higher in the incubator than in the room and just the opposite in the range of 315–2500 Hz. It is interesting to note that a 100 Hz tone appears in the frequency spectrum (Fig. 5) as a consequence of the electrical supply (second harmonic of the alternating current frequency in Spain).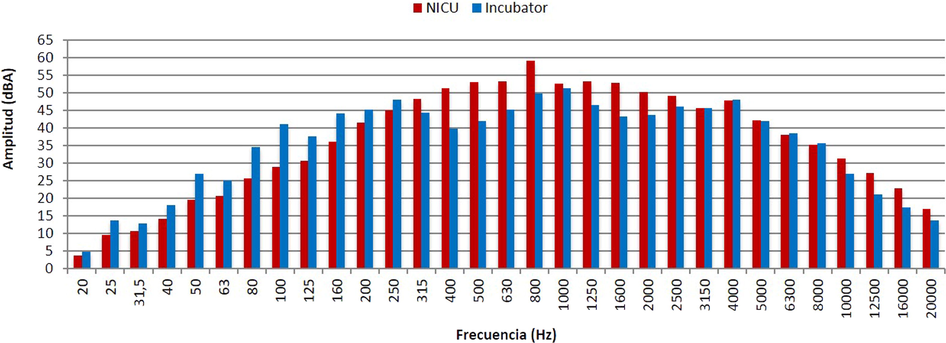
Comparison of the acoustic spectra for the NICU room and the inside of the incubator OCP 3000, during the second measurement campaign.
Noise levels inside incubators can be as high as LpA = 57 dB regardless of whether the noise levels outside stay low (Plangsangmas et al., 2012). Some authors have reported mean and maximum levels of 57.0 and 88.8 dB, respectively (Fortes-Garrido et al., 2014). As noted earlier, the noise inside an incubator comes mainly from its fan, the water recycling circuit, door opening and closure, and equipment alarms (Vendramini et al., 2011). Thus, although noise within an incubator should not exceed LpA = 60 dB according to, the standard ANSI/AAMI/IEC 60601-2-19:2009, alternative recommendations have set the limit (as said previously) at LpA = 45 dB (B. Beccrglund et al., 1999).
The second measurement series, performed on the OCP 300 model, exceeded the recommended limit over the frequency range of 200–4000 Hz (Fig. 6). This result suggests that an OCP 3000 incubator is “noisier” than a Giraffe incubator (Fig. 5); also, it is consistent with reported data for earlier comparative studies (Rodríguez Montaño, 2018) where, however, the differences were not so marked. A comparison of the sound spectrum recorded in the NICU and inside the incubator is shown in Fig. 8. If we follow Avery et al., conclusions regarding, the hearing sensitivity range of a fetus in the different phases of pregnancy (Avery et al., 2001), what can be deduced from the results presented in Figs. 5 and 6 is the following. For a neonate inside the Giraffe incubator, the exposition to noise is LAeq 500-1000Hz,24h = 48 dB, and for the OCP-3000 incubator LAeq 500-1000Hz,24h = 54.3 dB. For a full-term newborn inside the Giraffe incubator, the exposition to noise is LAeq 400-4000Hz,24h = 49.6 dB, and for the OCP-3000 incubator LAeq 400-4000Hz,24h = 57 dB. Exceeding in all cases is the recommended limit.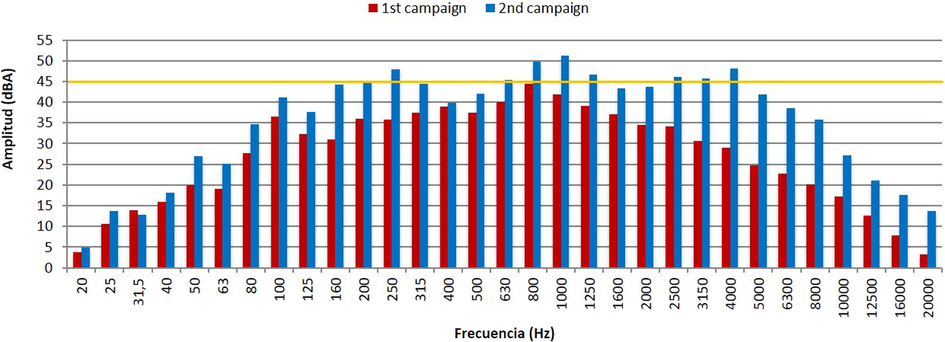
Comparison of the noise frequency spectra inside the incubators during the first and second series of measurements.
If the time series of the noise pressure levels inside and outside the incubator are correlated (Fig. 3), it is verified that there is a correlation during the day. But this does not happen during night hours when the values inside the incubator remain steady and always above the recommended values. This indicates that certain noise is generated by the incubator itself, noise that at night is higher than that induced by the NICU.
Answering the question asked above requires also considering the location and position of the incubator in each measurement series. Thus, the Giraffe incubator was at one end of the room far from the staff’s workbench, while the OCP 3000 incubator was in the main area, close to the workbench. This was the main reason inner noise levels were much higher in the OCP 3000 model —noise near the workbench is typically much higher than in other NICU locations.
5 Conclusions
Based on existing references and the acoustic measurements made in the NICU of the “Puerta del Mar” University Hospital (Cadiz, Spain), it can be affirmed that neonates that occupy the incubators in the case study NICU, will be exposed to excessive noise levels and frequencies for which their hearing systems are not yet prepared.
Three recommendations and good practices follow from the results of the tests. (i) The necessity of analyzing the acoustic quality inside every incubator and proposing, if necessary, the corresponding neonatal hearing protection. This analysis must include a frequency spectra evaluation that considers the neonate’s hearing range to minimize the health impact of neonates. (ii) The study of NICU in detail to place incubators with preterm infants in the least noisy areas, according to their gestational age. (iii) A combined mitigation plan that includes, staff training, continuous noise monitoring, relocation of alarms and adjustment of their volume, and improved NICUs with different strategies such as introducing special building materials (wall lining, floors, ceilings, ventilation, and air conditioning systems).
The three recommendations given can alleviate the problem of current hospitals, but to obtain a real improvement there are other possible lines of research and development. One of the most promising areas of study is the adaptation and redesign of incubators so that their interior can be more compatible with the correct auditory development of newborns. This is the research area in which the authors are developing their work and where a patent is expected soon.
Disclosure of Funding
“This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.”
Data availability
The data obtained to carry out this work is based on original sound recordings, processed using specific software, specifically the 7820 Evaluator, developed by the company Brüel & Kjær.
The 7820 type requires a license and associated HASP dongle to function. For this reason, it is necessary to apply certain restrictions to have this data.
The data sets generated and/or analyzed during the current study are not publicly available. Still, they are available through the authors upon reasonable request and with the permission of the director of the Acoustic Engineering Laboratory of the University of Cádiz [Ricardo Hernandez Molina].
Author Contributions
All authors contributed to the study’s conception and design. Conceptualization: [All authors], Funding acquisition: [Ricardo Hernández-Molina], Methodology, analysis, and conclusions: [Francisco Fernández-Zacarías], Project administration: [Virginia Puyana‐Romero], Resources: [Ricardo Hernández-Molina], Supervision: [All authors], Writing – original draft preparation: [Rodríguez-Montaño, Víctor], Review and editing: [All authors]. All authors read and approved the final manuscript.
CRediT authorship contribution statement
Víctor Rodríguez-Montaño: Supervision, Conceptualization, Writing – original draft, Writing – review & editing. Juan Luis Beira-Jiménez: Conceptualization, Supervision, Writing – review & editing. Francisco Fernández-Zacarías: Conceptualization, Methodology, Supervision, Writing – review & editing. José Luis Cueto Ancela: Conceptualization, Supervision, Writing – review & editing. Virginia Puyana-Romero: Conceptualization, Project administration, Supervision, Writing – review & editing. Ricardo Hernández-Molina: Resources, Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Acknowledgments
The authors are grateful to the NICU staff of the “Puerta del Mar” University Hospital (Cadiz, Spain), for their help in the development of this work. As well as the University of Cádiz for the concession of the Project within the framework of the “Program for the promotion and promotion of research and transfer at the University of Cádiz 2016-2017”, which has allowed the realization of this work.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Unidades de neonatología. Estándares y recomendaciones de calidad. Minist. Sanidad, Serv. Soc e Igual. 2014
- [CrossRef] [Google Scholar]
- Committee on Environmental Health. Noise: A Hazard for the Fetus and Newborn. Pediatrics.. 1997;100(4):724-727.
- [Google Scholar]
- Epidemiology of preterm birth and its clinical subtypes. J. Matern. Neonatal. Med.. 2006;19(12):773-782.
- [CrossRef] [Google Scholar]
- ANSI/AAMI/IEC 60601-2-19:2009: Medical Electrical Equipment Ù Part 2-19: Particular Requirements for the Basic Safety and Essential Performance of Infant Incubators.
- Neonatología : Fisiopatología y Manejo Del Recién Nacido (5th ed.). Montevideo: Médica Panamericana; 2001.
- B. Beccrglund, T., Lindvall, D.S., 1999. Guideline for community noise. https://doi.org/10.1260/0957456001497535.
- Effect of environmental changes on noise in the NICU. Adv. Neonatal. Care.. 2008;8(5):S5-S.
- [Google Scholar]
- Noise, and the premature infant: Physiological effects and practice implications. J. Obstet. Gynecol. Neonatal. Nurs.. 2003;32(4):447-454.
- [Google Scholar]
- Cardoso, S.M.S, Kozlowski, L de C., de Lacerda, A.B.M., Marques, J.M., Ribas, A., 2015. Newborn physiological responses to noise in the neonatal unit. Braz. J. Otorhinolaryngol. 81(6), 583–588. https://doi.org/10.1016/j.bjorl.2014.11.008.
- Noise level in neonatal incubators: A comparative study of three models. Int. J. Pediatr. Otorhinolaryngol. 2018:107.
- [CrossRef] [Google Scholar]
- The characterization of noise levels in a neonatal intensive care unit and the implications for noise management. J. Environ. Heal. Sci. Eng.. 2014;12(104):1-9.
- [CrossRef] [Google Scholar]
- Prospects for research in reproductive health and birth outcomes. J. Am. Med. Assoc.. 2001;285(5):633.
- [CrossRef] [Google Scholar]
- The relationship between physiological and behavioral measures of stress in preterm infants. J. Obstet. Gynecol. Neonatal. Nurs.. 2004;33(2):236-245.
- [Google Scholar]
- Hernandez Molina, R., Fernández Zacarías, F., Puyana Romero, V., et al. Characterizing the acoustic environment in a Neonatal Intensive Care Unit. Applied Acoustics; ISSN: 0003682X. Vol.165, pp. 1–11. https://doi.org/10.1016/j.apacoust.2020.107301.
- Le bruit en néonatologie, impact du personnel hospitalier. Presse Med.. 2004;33(20):1421-1424.
- [CrossRef] [Google Scholar]
- Knutson, A.J., 2012. Acceptable noise levels for neonates in the neonatal intensive care unit. Indep Stud Capstones. 2012. http://digitalcommons.wustl.edu/pacs_capstones/643.
- Safe sound exposure in fetus and preterm Infant. J. Obs. Gynecol. Neonatal. Nurs.. 2012;41(2):166-170.
- [CrossRef] [Google Scholar]
- Kurtzberg, D., Stapells, D.R., 1998. Wallance IF. Event-related potential assesment of auditory system integrity: implications for language development. In: Vietze, P.M., Vaughan, H.G. (Eds.), Early identificationof infants with Dev Disabil Philadelphia Grune Strat.
- Questionable sound exposure outside of the womb: frequency analysis of environmental noise in the neonatal intensive care unit. Acta Paediatr.. 2015;104(1):e14-e19.
- [CrossRef] [Google Scholar]
- Morata, T., Santos, U., 1996. Efeitos do ruído na audição. In: Santos, UDP. Ruído: Riscos e Prevenção. São Paulo, Hucitec. 43–54.
- A single-room NICU-The next generation evolution in the design of neonatal intensive care units. Acad. J.. 2003;6:3.
- [Google Scholar]
- A study investigating sound sources and noise levels in neonatal intensive care units. South African J. Child Heal.. 2014;8(1):6-10.
- [CrossRef] [Google Scholar]
- Factores asociados con el parto prematuro entre 22 y 34 semanas en un hospital público de Santiago. Rev. Med.Chil.. 2012;140(1):19-29.
- [CrossRef] [Google Scholar]
- Energy expenditure in preterm infants during periods of environmental stress in the neonatal intensive care unit. Japan J. Nurs. Sci.. 2014;11(4):241-247.
- [CrossRef] [Google Scholar]
- Sound Pressure Level in an Infant Incubator. Mapan – J. Metrol. Soc. India. 2012;27(4):199-203.
- [Google Scholar]
- Rodríguez Montaño, V.M., 2018. Análisis del acondicionamiento acústico del habitáculo de una incubadora neonatal: propuestas de mejora.
- Sound environments surrounding preterm infants within an occupied closed incubator. J. Pediatr. Nurs.. 2016;31(2):e149-e154.
- [CrossRef] [Google Scholar]
- Altering the NICU and measuring infants’ responses. Acta Paediatr. Int. J. Paediatr.. 2000;89(5):577-581.
- [CrossRef] [Google Scholar]
- The American Institute of Architects Academy of Architecture for Health, Guidelines for Design and Construction of Hospital and Health Care Facilities. Vol. 48; 2001.
- Behavioural and physiological reactivity to noise in the newborn. J. Paediatr Child Health.. 2004;40(5–6):275-281.
- [CrossRef] [Google Scholar]
- US-EPA (The U.S. Environmental Protection Agency), 1974. Information on Levels of Environmental Noise Requisite to Protect Public Health and Welfare with an Adequate Margin of Safety.
- Internal noise levels in neonatal intensive care unit incubators *. Acta Paul Enferm.. 2011;24(3):359-364.
- [Google Scholar]
- Recommended standards for newborn ICU design. J. Perinatol.. 2006;26:S2-S18.
- [CrossRef] [Google Scholar]
Appendix A
Supplementary material
Appendix A
Supplementary material
The following are the Supplementary data to this article:







