Reduced platelet-lymphocyte ratio in a Saudi population with impaired fasting glycemia and hyperglycemia
⁎Corresponding author at: Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia. malfeehily@ksu.edu.sa (Mohammad A. Alfhili)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Background
Diabetes mellitus (DM) is an inflammatory disorder characterized by elevated fasting blood glucose (FBG) with life-threatening complications. However, the physiological response of peripheral blood cells to impaired fasting glycemia (IFG) and hyperglycemia (HG) is ill-defined.
Aim
In this report, we investigated the patterns of change in platelet-lymphocyte ratio (PLR) relative to glycemic control.
Methods
WBC count, PLR, C-reactive protein (CRP), FBG, HbA1c, and Hb results for 1,793 subjects were retrospectively analyzed.
Results
PLR was significantly reduced in HG compared to IFG and to normoglycemia (NG) while FBG was only significantly lower in males with elevated PLR. Increased PLR was less prevalent in subjects with HG and was a protective factor against HG. Upon stratification by HbA1c, PLR was found to be significantly lower in IFG compared to NG only in females. Importantly, PLR performed better than CRP in discriminating NG and HG in females.
Conclusion
This report provides insights into the cellular physiological response to DM and evaluates PLR as a novel marker for DM management.
Keywords
Diabetes
Inflammation
Platelet-lymphocyte ratio
Biomarkers
- DM
-
Diabetes mellitus.
- HG
-
Hyperglycemia.
- FBG
-
Fasting blood glucose.
- PLR
-
Platelet-lymphocyte ratio.
- CRP
-
C-reactive protein.
- CBC
-
Complete blood count.
- WBC
-
White blood cell.
- PR
-
Prevalence risk.
- OR
-
Odds ratio.
- PRR
-
Prevalence risk reduction.
- ROC
-
Receiver operating characteristic.
- NLR
-
Neutrophil-lymphocyte ratio
Abbreviations
1 Introduction
Diabetes mellitus (DM) is a chronic disease characterized by hyperglycemia (HG) either due to insufficient insulin synthesis or response. Genetic predisposition, unhealthy diet, increased body weight, tobacco use, and physical inactivity are known risk factors of DM. Increased fasting blood glucose (FBG) is accompanied by a parallel increase in blood osmotic pressure leading to leakage of cellular content and organ damage (Zapuskalov, Filippova, Shilova, & Krivosheina, 2000). Complications of DM thus include vascular, neurological, retinal, and renal sequelae. In fact, DM predisposes to blindness, infection, limb amputation, stroke, renal failure, myocardial infarction, and premature mortality (WHO, 2021).
Mounting evidence points at a central role for systemic inflammation in mediating the pathological sequelae of DM. In particular, insulin resistance develops due to overproduction of interleukins, adipokines, and chemokines, which precipitate β-cell dysfunction and inflammatory damage to peripheral tissue (Rehman & Akash, 2016). Oxidative injury instigated by HG and hyperlipidemia stimulates stress signaling pathways that decreases tissue sensitivity to insulin (Cooke, 2004). The classical inflammatory marker, C-reactive protein (CRP), has been extensively investigated in DM screening, diagnosis, and prognosis, with inconsistent findings biased in part by ethnicity (Pan, Wang, Yuan, & Koh, 2017; Rehman & Akash, 2016; Shaheer, Tharayil, & Krishna, 2017).
Platelets and lymphocytes both contribute to thrombotic events and inflammatory processes by releasing cytokines and growth factors (Kurtul & Ornek, 2019). Platelet-lymphocyte ratio (PLR) has thus been investigated as an emerging inflammatory marker in a variety of pathological conditions (Uslu et al., 2015). PLR was found to be a predictor of various outcomes in cardiovascular disease (Kurtul & Ornek, 2019). PLR was also found to be an independent risk factor for pneumonia and was associated with poor prognosis in acute ischemic stroke patients (Altintas, Altintas, Tasal, Kucukdagli, & Asil, 2016; Li & He, 2022). Contrasting reports do exist however regarding the association of PLR with DM (Atak et al., 2019; Mendes, Oliveira, & Alcantara, 2019). In a meta-analysis, PLR was not even associated with gestational DM (Hessami et al., 2021). Since PLR is a feasible and inexpensive marker included in a routine complete blood count (CBC) test, this work aims to assess the pathological fluctuations and clinical utility of PLR in light of glycemic control.
2 Materials and methods
2.1 Study design
The protocol for this retrospective, cross-sectional study was approved by the Biomedical Ethics Unit at Al-Borg Medical Laboratories (approval number: 07/21). Laboratory records for 1,793 subjects were extracted from the database of Al-Borg Medical Laboratories and analyzed for age, gender, white blood cell (WBC) count, platelet count, PLR, CRP, FBG, hemoglobin A1c (HbA1c), and Hb. PLR was calculated by dividing the absolute platelet count over that of lymphocytes. Characteristics of study subjects are shown in Table 1. Age groups were designated as young (<17 years), young adults (18–39 years), adults (40–64 years), and elderlies (≥65 years) as per our previous reports (Alfhili, Alsughayyir, Basudan, Ghneim, Aboul-Soud, et al., 2022; Alfhili, Alsughayyir, Basudan, Alsubki, et al., 2022; Alfhili, Alsughayyir, Basudan, Ghneim, Alfaifi, et al., 2022; Alfhili, Basudan, et al., 2022). Normal values for WBC count were 4.5–11.0x106 cells/ml whereas for platelets were 150-400x106 cells/ml. We used a range of 36.63–172.68 for a normal PLR (Wu, Zou, Wang, Tan, & Yu, 2019). FBG < 100 mg/dl as normoglycemia (NG), 100–125 mg/dl as impaired fasting glycemia (IFG), and ≥ 126 mg/dl as HG were used as cutoff points as per the ADA guidelines (American Diabetes, 2014). HbA1c values were set at < 6.5% for NG, 6.5–8.5% for IFG, and > 8.5% for HG (American Diabetes, 2014). To validate HbA1c results, a Hb cutoff of < 12 g/dl was used to exclude anemics (Alquaiz et al., 2015).
| Gender | No. of subjects (%) |
|---|---|
| Male | 804 (44.84) |
| Young | 58 (3.23) |
| Young adults | 325 (18.12) |
| Adults | 346 (19.29) |
| Elderlies | 75 (4.18) |
| Female | 975 (54.37) |
| Young | 72 (4.01) |
| Young adults | 524 (29.22) |
| Adults | 308 (17.17) |
| Elderlies | 71 (3.95) |
| Unknown | 14 (0.78) |
| WBC count (x106/ml) | Mean (95% CI) |
| Male | |
| 6.08 (5.95–6.21) | |
| Female | |
| 6.02 (5.90–6.14) | |
| Platelet count (x106/ml) | Mean (95% CI) |
| Male | |
| 266.55 (261–272) | |
| Female | |
| 271.44 (267–276) | |
2.2 Statistics
GraphPad Prism v9.2.0 (GraphPad Software, Inc., San Diego, CA, USA) was used for statistical analysis. Results are represented as means ± 95% CI. Unpaired, two-tailed student’s t test was used for two groups and one-way ANOVA with Tukey’s correction for more than two groups. Pearson correlation and simple linear regression were employed in univariate models, and the natural sampling design allowed for calculation of the prevalence risk (PR), odds ratio (OR), and prevalence risk reduction (PRR). The cutoff for statistical significance was set as P < 0.05.
3 Results
Our results show that PLR is significantly diminished in HG compared to NG, which remained significant after adjustment for gender. There was significant reduction in PLR between IFG and HG but not between NG and IFG (Fig. 1A-C). Similarly, FBG was only significantly lower in males with increased PLR (Fig. 1D-F).
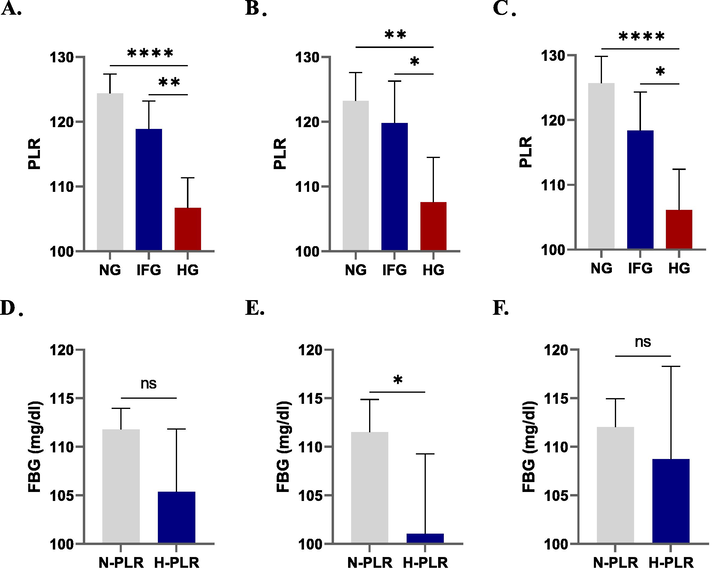
-
Changes in PLR in light of FBG in males and females. Means ± 95% CI of PLR in prediabetics and diabetics of (A) both genders, (B) males, and (C) females. Means ± 95% CI of FBG in normal PLR (N-PLR) and high PLR (H-PLR) groups in (D) both genders, (E) males, and (F) females.
Age-wise comparisons revealed a significant decrease in PLR between IFG and HG in the young, and between NG and HG in young adults and adults (Fig. 2A-C). In the elderlies, no significant difference in PLR was observed based on the glycemic state (Fig. 2D). Next, we adjusted for both age and gender and found that significance was displaced in males across all age groups (Fig. 2E-H) while in females PLR was only significantly lower in HG compared to IFG in the young (Fig. 2I) and in HG compared to NG in adults (Fig. 2K).
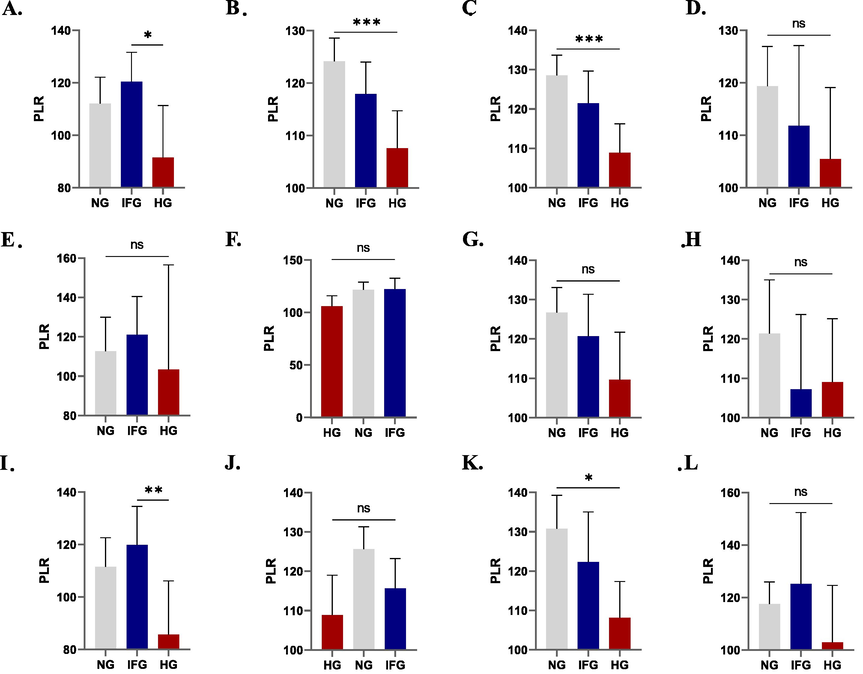
-
Individual and combined effect of gender and age on PLR. Means ± 95% CI of PLR in prediabetics and diabetics. Both genders are presented in (A) young, (B) young adults, (C) adults, (D) and elderlies. Males are presented in (E) young, (F) young adults, (G) adults, and (H) elderlies. Females are presented in (I) young, (J) young adults, (K) adults, and (L) elderlies.
As revealed from our linear regression analysis, we found no correlation between PLR and FBG even after adjustment for gender (Fig. 3A-C). However, the small P values indicate that PLR does indeed influence FBG but other factors are likely to be involved as well. For comparison, correlation between CRP and FBG followed a similar pattern although it was not significant in females (Fig. 3F).
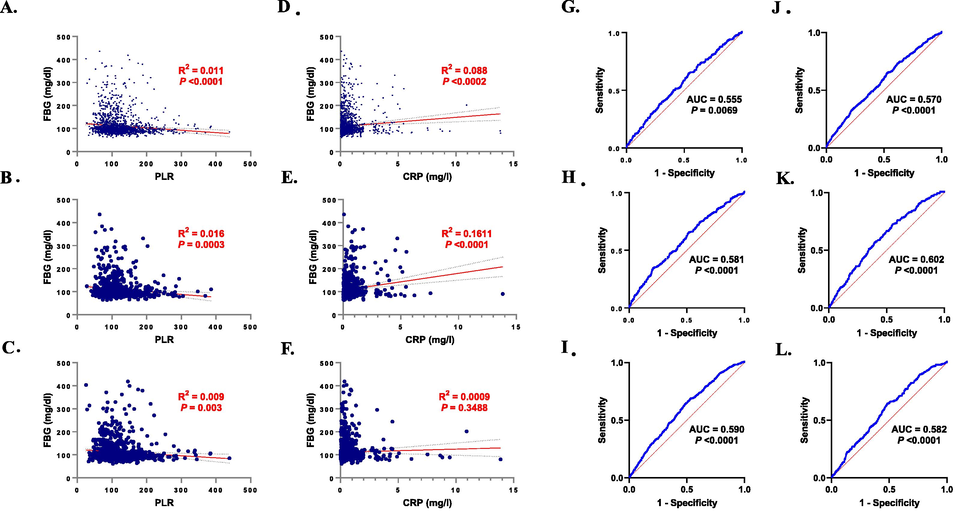
-
Association of PLR with FBG and CRP. (A-C) Simple linear regression of PLR and FBG in both genders, males, and females, respectively. (D-F) Simple linear regression of CRP and FBG in both genders, males, and females, respectively. (G-I) ROC curves of PLR and FBG in both genders, males, and females, respectively. (J-L) ROC curves of CRP and FBG in both genders, males, and females, respectively.
In congruence with these results, assessment of the prevalence of elevated PLR in our study population revealed that it was less prevalent in individuals with HG in comparison to those with NG. In hyperglycemic males, elevated PLR was less by 37.52% while in females it was less by 31.48%. This is the percent reduction in prevalence of high PLR in the HG group compared to NG. It was obtained by first calculating the difference in prevalence between NG and HG groups, and then finding out the proportion this difference constitutes relevant to the NG group. Similarly, when PLR was elevated, HG was less prevalent by 25.03% and 24.35% in males and females, respectively (Table 2). Moreover, PR values for increased PLR were 0.72 and 0.76 for males and females, respectively, whereas OR values were 0.59 for males and 0.63 for females. The PRR is derived from PR and is a function of OR. The PRR of elevated PLR against HG was therefore 0.40 in males and 0.36 in females (Table 2).
| Prevalence (%) | ||||||
|---|---|---|---|---|---|---|
| Elevated PLR | All subjects | NG | HG | |||
| Male and female | 10.94 | 12.91 | 8.43 | |||
| Male | 10.61 | 12.63 | 7.89 | |||
| Female | 11.36 | 13.34 | 8.94 | |||
| HG | All subjects | N-PLR | H-PLR | |||
| Male and female | 43.9 | 45.14 | 33.84 | |||
| Male | 42.69 | 43.99 | 31.76 | |||
| Female | 45.04 | 46.27 | 35.45 | |||
| Risk assessment | ||||||
| Gender | PR | 95% CI | P | OR | 95% CI | P |
| Male and female | 0.74 | 0.61–0.91 | 0.0056 | 0.62 | 0.45–0.84 | 0.0029 |
| Male | 0.72 | 0.52–0.99 | 0.0477 | 0.59 | 0.36–0.95 | 0.0326 |
| Female | 0.76 | 0.58–0.99 | 0.0466 | 0.63 | 0.42–0.96 | 0.0329 |
NG, normoglycemic; HG, hyperglycemic; N-PLR, normal PLR; H-PLR, high PLR. P < 0.05 is statistically significant.
To further assess the clinical utility of PLR in discriminating individuals with NG from those with IFG and HG, we performed a receiver operating characteristic (ROC) curve analysis as shown in Fig. 3G-I. The area under the curve (AUC) was highest in females reaching 0.590 (P < 0.0001) which is higher than CRP in that group (AUC = 0.582, P < 0.0001). In contrast, the AUC of CRP was higher than that of PLR in males (0.602 vs. 0.581, P < 0.0001 for both).
Next, we stratified subjects based on their glycemic status using HbA1c levels instead of FBG. Fig. 4A-C shows that PLR was significantly decreased in prediabetics and diabetics compared to nondiabetics in the unadjusted model. This was also true in females but in males PLR was only significantly lowered in diabetics compared to non-diabetics. Conversely, HbA1c was only significantly reduced in males with high PLR (Fig. 4E). Furthermore, the correlation between PLR and HbA1c was similar to that observed between PLR and FBG (Fig. 4G-I). Testing for the diagnostic accuracy of PLR in discriminating individuals based on HbA1c levels yielded the best performance in females (AUC = 0.621, P < 0.0001). Notably, PLR performed better than CRP in discriminating NG from HG using either FBG or HbA1c to segregate controls and patients.
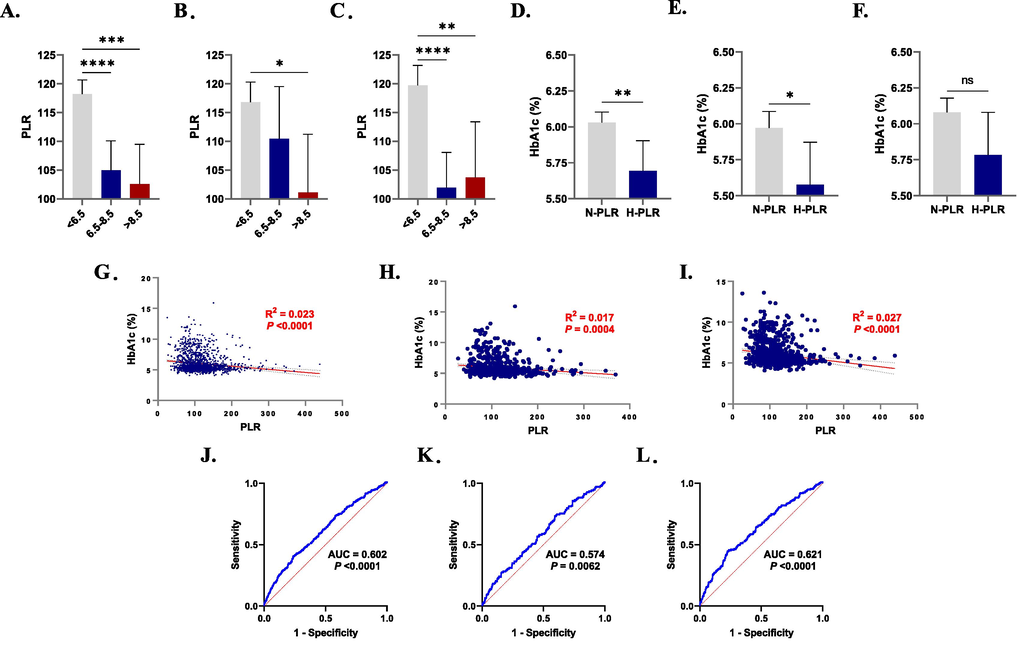
-
Patterns of PLR in light of HbA1c in males and females. Means ± 95% CI of PLR in prediabetics and diabetics of (A) both genders, (B) males, and (C) females. Means ± 95% CI of HbA1c in normal PLR (N-PLR) and high PLR (H-PLR) groups in (D) both genders, (E) males, and (F) females. (G-I) Simple linear regression of PLR and HbA1c in both genders, males, and females, respectively. (J-L) ROC curves of PLR and HbA1c in both genders, males, and females, respectively.
4 Discussion
Physiological sequelae of disturbances in FBG include tissue infiltration of inflammatory cells causing oxidative injury. In this report, we demonstrate that platelets and lymphocytes are altered in IFG and HG with contrasting age and gender disparities. We also present a comparative binary analysis of PLR based on FBG and HbA1c levels which revealed that PLR discriminates male diabetics based on FBG better than HbA1c, whereas in females, PLR discriminates diabetics based on HbA1c better than FBG. Moreover, PLR was only significantly decreased in females with IFG as defined by HbA1c but not FBG.
Stratification of subjects based on FBG levels permitted PLR to distinguish HG from NG and IFG (Fig. 1A-C). Increased PLR was also found to be less common in HG and was also a protective factor against glucose dysregulation (Table 2). There was, however, no significant difference between NG and IFG groups which suggests that PLR may not be a sensitive marker of glucose disturbances. In a study by Metroglu et al., PLR exhibited biphasic dynamics where it was low in prediabetes and early DM but high in late DM (Mertoglu & Gunay, 2017). Another report showed that PLR performed better than neutrophil–lymphocyte ratio (NLR) in correlating with hepatitis C severity (Meng et al., 2016) and with inflammatory response to renal disease (Turkmen et al., 2013). Also, increased PLR was an independent risk factor for higher mortality in DM complicated by myocardial infarction (Hudzik et al., 2015). No consensus regarding the progression of PLR in diabetic patients was however found in the literature, and interventional, longitudinal studies to monitor alterations in PLR over time and under varying clinical contexts are urgently needed.
Our study also highlights the gender disparity associated with changes in PLR in relation to FBG. When subjects were divided into normal PLR and high PLR groups, only males had significantly lower FBG in the latter group (Fig. 1E). Further age-wise comparisons of PLR in FBG-stratified males displaced that significance across all age groups (Fig. 2E-H). In females, PLR was only significantly decreased in HG compared to IFG in the young and in HG compared to NG in adults (Fig. 2I-L). In agreement with these observations, accumulating evidence indicates that DM is more prevalent in Middle Eastern women which is in contrast to trends observed in other ethnicities (Tramunt et al., 2020). Conversely, peaks of DM prevalence are observed in men earlier than in women (Cho et al., 2018). One possible explanation is that sex steroids participate in the maintenance of plasma glucose levels by regulating lipid and carbohydrate metabolism and thus counteract insulin resistance. This is evidenced by the increased incidence of DM in menopausal women with estrogen deficiency and its reversal by estrogen therapy (Appiah, Winters, & Hornung, 2014). Estrogens have also been shown in preclinical models to prevent apoptosis and preserve pancreatic β-cell longevity (Le May et al., 2006). On the other hand, estrogen impairs glucose tolerance resulting in higher plasma glucose following oral glucose tolerance test in women (Mauvais-Jarvis, 2018). Like estrogen in women, testosterone similarly possesses diabetogenic potential. In fact, testosterone exhibits a rather dichotomous dynamism in regulating glucose homeostasis in men and women. Decreasing levels of testosterone in elderly males predispose to DM, while elevated levels in women along with reduced sex hormone-binding globulin disrupt glucose metabolism (Hackett et al., 2014; Wang et al., 2021). Perhaps more important are the differences in insulin sensitivity between males and females. Higher postprandial insulin, C-peptide, and glucose utilization by skeletal muscle may account for the increased insulin sensitivity in women (Mauvais-Jarvis, 2018).
Gender differences were similarly underscored when assessing the glycemic state using HbA1c. In females, PLR was sensitive to identify both IFG and HG (Fig. 4C) while in males it identified only those with HG (Fig. 4B). Also similar to FBG levels, only males with high PLR had significantly lower HbA1c (Fig. 4E). Although men and women respond differently to glucose challenge, with women having significantly lower postprandial FBG than men, this is not the case with regard to HbA1c (Mauvais-Jarvis, 2018). Nevertheless, gender differences have indeed been described in the literature in various ethnicities. In Chinese adults, significantly higher baseline HbA1c was found in males and positively correlated with age (Ma, Liu, Xiang, Shan, & Xing, 2016). Also, at normal HbA1c, Chinese men have a lower risk of cardiovascular disease and are more resistant to metabolic exhaustion leading to DM than women (Du, Yuan, Zhou, & Sun, 2016). In Italy, HbA1c was significantly higher in young male subjects compared to females (Callà C, 2019). HbA1c has also been utilized to predict mortality. It has been demonstrated in the Danish population that variations and absolute change in HbA1c carried a greater risk for mortality in subjects below and above a cutoff of 8%, respectively (Skriver, Sandbaek, Kristensen, & Stovring, 2015).
The strength of the current study is based on the large sample size which is representative of the Saudi population, nonexistent variation in generation, acquisition, and validation of data, and the ability to determine prevalence and risk estimates. However, given the cross-sectional nature of this study, it was not possible to determine a possible causal relationship between disturbances in glucose regulation and fluctuations in PLR. In addition, data on potentially confounding factors that may or may not have significantly influenced the findings were missing.
5 Conclusion
In conclusion, the current study highlights the disruption in platelet and lymphocyte homeostasis in response to elevations in FBG and HbA1c. Analysis of lymphocyte subtypes Th1 (pro-inflammatory) and Th2 (anti-inflammatory) and the governing dynamics of antigenic shifts relative to glycemic control deserves further examination. Equally important, the assessment of the usefulness of PLR in predicting DM risk and development, the occurrence of neurovascular and renal complications, and the need for hypoglycemic agents and insulin replacement therapy are urgently needed.
CRediT authorship contribution statement
Mohammad A. Alfhili: Project administration, Supervision, Writing – review & editing, Investigation, Methodology, Conceptualization, Formal analysis, Writing – original draft. Jawaher Alsughayyir: Visualization, Writing – review & editing, Investigation, Methodology, Conceptualization, Formal analysis, Writing – original draft. Ahmed Basudan: Investigation, Methodology, Formal analysis, Writing – original draft. Mohammed Alfaifi: Investigation, Methodology, Formal analysis, Writing – original draft. Zuhier A. Awan: Project administration, Methodology, Data curation, Validation, Formal analysis, Writing – original draft. Mohammed R. Algethami: Project administration, Data curation, Methodology, Validation, Formal analysis, Writing – original draft. Yazeed A. Al-Sheikh: Supervision, Writing – review & editing, Software, Investigation, Methodology, Resources, Formal analysis, Writing – original draft, Funding acquisition.
Acknowledgement
The authors extend their appreciation to the Deputyship for Research & Innovation, Ministry of Education in Saudi Arabia for funding this research through grant number IFKSURC-1-4403.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Isolated and combined effect of age and gender on neutrophil-lymphocyte ratio in the hyperglycemic Saudi population. Medicina (Kaunas). 2022;58(8)
- [CrossRef] [Google Scholar]
- Monocyte-lymphocyte ratio and dysglycemia: a retrospective, cross-sectional study of the Saudi population. Healthcare (Basel). 2022;10(11)
- [CrossRef] [Google Scholar]
- Patterns of dyslipidemia in the anemic and nonanemic hypertensive Saudi population: a cross-sectional study. Int. J. Gen. Med.. 2022;15:7895-7906.
- [CrossRef] [Google Scholar]
- Patterns of 25-hydroxyvitamin D3, calcium status, and anemia in the Saudi population: a cross-sectional study. Life (Basel). 2022;12(12)
- [CrossRef] [Google Scholar]
- Prevalence and correlates of anaemia in adolescents in Riyadh city, Kingdom of Saudi Arabia. Public Health Nutr.. 2015;18(17):3192-3200.
- [CrossRef] [Google Scholar]
- The relationship of platelet-to-lymphocyte ratio with clinical outcome and final infarct core in acute ischemic stroke patients who have undergone endovascular therapy. Neurol. Res.. 2016;38(9):759-765.
- [CrossRef] [Google Scholar]
- Standards of medical care in diabetes–2014. Diabetes Care. 2014;37(Suppl 1):S14-S80.
- [CrossRef] [Google Scholar]
- Bilateral oophorectomy and the risk of incident diabetes in postmenopausal women. Diabetes Care. 2014;37(3):725-733.
- [CrossRef] [Google Scholar]
- Atak, B., Aktas, G., Duman, T. T., Erkus, E., Kocak, M. Z., & Savli, H. (2019). Diabetes control could through platelet-to-lymphocyte ratio in hemograms. Rev Assoc Med Bras (1992), 65(1), 38-42. doi:10.1590/1806-9282.65.1.38.
- Callà C, N. G., Pieri M, Pignalosa S, Zenobi R, Bernardini S, Dessi M, Martino FG, Marrone G, Noce A, Di Daniele N. (2019). HbA1c: Gender Differences in Non-Diabetic Young Population. Biomedical Journal of Scientific & Technical Research, 16(2), 11981-11984. doi:10.26717/BJSTR.2019.16.002838
- IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract.. 2018;138:271-281.
- [CrossRef] [Google Scholar]
- Asymmetrical dimethylarginine: the Uber marker? Circulation. 2004;109(15):1813-1818.
- [CrossRef] [Google Scholar]
- Sex differences in the effect of HbA1c-de fi ned diabetes on a wide range of cardiovascular disease risk factors. Ann. Med.. 2016;48(1–2):34-41.
- [CrossRef] [Google Scholar]
- Hackett, G., Cole, N., Bhartia, M., Kennedy, D., Raju, J., Wilkinson, P., & Group, B. S. (2014). Testosterone replacement therapy improves metabolic parameters in hypogonadal men with type 2 diabetes but not in men with coexisting depression: the BLAST study. J Sex Med, 11(3), 840-856. doi:10.1111/jsm.12404
- Gestational diabetes mellitus and inflammatory biomarkers of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio: a systematic review and meta-analysis. Biomarkers. 2021;26(6):491-498.
- [CrossRef] [Google Scholar]
- Platelet-to-lymphocyte ratio is a marker of poor prognosis in patients with diabetes mellitus and ST-elevation myocardial infarction. Biomark. Med.. 2015;9(3):199-207.
- [CrossRef] [Google Scholar]
- Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology. 2019;70(9):802-818.
- [CrossRef] [Google Scholar]
- Estrogens protect pancreatic beta-cells from apoptosis and prevent insulin-deficient diabetes mellitus in mice. Proc. Natl. Acad. Sci. U. S. A.. 2006;103(24):9232-9237.
- [CrossRef] [Google Scholar]
- Association of Platelet-to-lymphocyte ratio with stroke-associated pneumonia in acute ischemic stroke. J. Healthc. Eng.. 2022;2022:1033332.
- [CrossRef] [Google Scholar]
- Association between glycated hemoglobin A1c levels with age and gender in Chinese adults with no prior diagnosis of diabetes mellitus. Biomed. Rep.. 2016;4(6):737-740.
- [CrossRef] [Google Scholar]
- Gender differences in glucose homeostasis and diabetes. Physiol. Behav.. 2018;187:20-23.
- [CrossRef] [Google Scholar]
- Comparison of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in normoglycemic and hyperglycemic subjects. Einstein (Sao Paulo). 2019;17(1):eAO4403.
- [CrossRef] [Google Scholar]
- The platelet-to-lymphocyte ratio, superior to the neutrophil-to-lymphocyte ratio, correlates with hepatitis C virus infection. Int. J. Infect. Dis.. 2016;45:72-77.
- [CrossRef] [Google Scholar]
- Neutrophil-Lymphocyte ratio and Platelet-Lymphocyte ratio as useful predictive markers of prediabetes and diabetes mellitus. Diabetes Metab. Syndr.. 2017;11(Suppl 1):S127-S131.
- [CrossRef] [Google Scholar]
- High-sensitive C-reactive protein and risk of incident type 2 diabetes: a case-control study nested within the Singapore Chinese Health Study. BMC Endocr. Disord.. 2017;17(1):8.
- [CrossRef] [Google Scholar]
- Mechanisms of inflammatory responses and development of insulin resistance: how are they interlinked? J. Biomed. Sci.. 2016;23(1):87.
- [CrossRef] [Google Scholar]
- A comparative study of high sensitivity C-reactive protein and metabolic variables in type 2 diabetes mellitus with and without nephropathy. J. Clin. Diagn. Res.. 2017;11(9):BC01-BC04.
- [CrossRef] [Google Scholar]
- Relationship of HbA1c variability, absolute changes in HbA1c, and all-cause mortality in type 2 diabetes: a Danish population-based prospective observational study. BMJ Open Diabetes Res. Care. 2015;3(1):e000060.
- [Google Scholar]
- Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63(3):453-461.
- [CrossRef] [Google Scholar]
- Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodial. Int.. 2013;17(3):391-396.
- [CrossRef] [Google Scholar]
- Two new inflammatory markers associated with Disease Activity Score-28 in patients with rheumatoid arthritis: neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Int. J. Rheum. Dis.. 2015;18(7):731-735.
- [CrossRef] [Google Scholar]
- Wang, A., Gerstein, H. C., Lee, S. F., Hess, S., Pare, G., Ryden, L., & Mellbin, L. G. (2021). Testosterone and sex hormone-binding globulin in dysglycemic women at high cardiovascular risk: A report from the Outcome Reduction with an Initial Glargine Intervention trial. Diab Vasc Dis Res, 18(2), 14791641211002475. doi:10.1177/14791641211002475.
- WHO. (2021). Diabetes. Retrieved from https://www.who.int/news-room/fact-sheets/detail/diabetes
- Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in Chinese Han population from Chaoshan region in South China. BMC Cardiovasc. Disord.. 2019;19(1):125.
- [CrossRef] [Google Scholar]
- The role of the osmotic pressure of the blood in the pathogenesis of diabetic changes in the retina. Vestn Oftalmol. 2000;116(2):32-34.
- [Google Scholar]







