Translate this page into:
Prevalence and investigations of bacterial contamination in dental healthcare associated environment
⁎Corresponding author. g.abusalim@psau.edu.sa (Ghadah Salim Abusalim) mjais_s@yahoo.com (Ghadah Salim Abusalim)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Microbial contamination of medical substrate surface of dental parts touched or exposed to blood and saliva of patients can act as a reservoir for pathogenic bacteria, resulting in cross-contamination. For this reason, presence of oral microorganisms in dental clinics is a major source of dental contamination and infection worldwide. The work described here aimed to determine the presence of bacteria on variety of dental clinic surfaces including a dental chair arm rest, a sink/faucet, the floor beneath a dental chair; a towel dispenser, handles connected to a light and to an instrument table; dental record paper; an X-ray viewer and finally, a bench and head-rest in five separate departments (pediatric dentistry, implant, dental prosthetics, oral medicine and restorative dentistry) of the King Saud University Dental Hospital, both before and after patient treatment. The isolation and identification of bacterial colonies was achieved using a range of methods such as using a Vitek2 automated system. The results showed that all surfaces in different departments were contaminated with bacteria, most notably in the Implant Department, while much less bacterial contamination was reported in the Department of Oral Medicine. The most commonly isolated bacteria were species of, Staphylococcus, Streptococcus, Pseudomonas, Bacillus and Micrococcus.
Keywords
Dental clinic
Bacterial contamination
Oral microorganisms
Infection
1 Introduction
Dental staff and patients are exposed daily to increased risk of cross-infection in the dental clinics setting by a wide range of pathogens and spores transmitted by pollutants and particles resulting from dental operating procedures (Harrel and Molinari, 2004; Castiglia et al., 2008; Szymanska, 2007). The oral microbial flora provides a potentially important source of cross-infection and contamination in dental clinics around the world (Ghosh and Mallick, 2012). Microorganisms can spread during a dental procedure following the dispersion of aerosols and splashes, and pathogens can be transmitted via blood and saliva then can be transmitted to the surrounding surfaces found in the dental clinics (Castiglia et al., 2008). Among the significant bacteria that can occur infection in dental environments are Pseudomonas aeruginosa, Streptococcus pneumoniae, Klebsiella pneumoniae, Mycobacterium tuberculosis, Legionella, Escherichia coli and pneumophila. Also, infectious agents such as Hepatitis B and C virus, Human Immunodeficency virus, Epstein Barr virus, Herpes Simplex virus, and Cytomegalovirus (Castiglia et al., 2008; Pasquarella et al., 2010). Many of these bacterial infections can survive on surfaces for extended periods of time unless they are removed through sterilization or disinfection (Kohn et al., 2003).
According to some studies, the environment, such as water, air, and surfaces, can play an essential role in pathogen transmission. Biofilm formation, water stagnation and a lack of disinfection in dental unit water systems encourage the growth of microorganisms (Barbeau and Nadeau, 1997; Checchi et al., 1998; Singh and Coogan, 2005; Zanetti et al., 2000). Moreover, generators and air–water infusion pumps can sometimes nebulize the saliva and microorganisms contained in the patient's mouth, contaminating the surrounding air and surfaces (King, 1997). Disease causes when microorganisms pass through the body, settle in a suitable location, and start reproducing (Andersen et al., 2009). Some people are more concerned about aerobic bacteria because they have a history of rheumatic heart disease, endocarditis mitral, valve prolapse and prosthetic joints (Williams et al., 2003).
Such contaminants can cause direct dental infection and also provide an indirect source of work-related risks (Pasquarella et al., 2010). Microbial prevalence contributes in a number of ways to disease spread in the dental clinics setting from patient to the clinical staff (Merchant,1991), from dental staff to the patient, from one patient to another (Borer et al., 2005), as well as from the dental clinic itself to the public (Brady et al., 2006). Infections in dental clinics settings which involve antibiotic-resistant bacterial strains are particularly important from the perspective of public health (Perveen et al., 2013). For this reason, the control of pathogens is highly significant in reducing infection spread (Woo and Joo, 2010, Kazi and Rajeev, 2012). Gugelmin et al., 2003 reported the prevalence of microbial contamination in waterlines used in a dental unit and concluded that the resultant biofilm formation is likely to contaminate dental-unit water.
The aim of the present study was to determine the prevalence of bacteria on various surfaces (a dental chair-arm rest; a sink and faucet; the floor beneath a dental chair; a towel dispenser; handles to a light and instrument table; paper dental records; an X-ray viewer; a bench and head rest) located in five departments (pediatric dentistry, implant, dental prosthetics, oral medicine and restorative dentistry). Samples were taken before and after patient-treatment.
2 Materials and methods
2.1 Collection and processing of samples
Five clinics were selected randomly patient for each specialty clinic. A Q-tip swab was used by the dental assistant to swab the ten different clinics surfaces for screening, prior to the patient entering the clinic for treatment and after the patient left. The Q-tip swab is then capped in the reservation gel and collected for storage before being sent to the laboratory for sample-analysis. A single specimen was obtained from the following dental clinic surfaces: a dental chair arm rest, a sink/faucet, the floor beneath a dental chair; a towel dispenser, handles connected to a light and to an instrument table; dental record paper; an X-ray viewer and finally, a bench and head-rest in five separate departments (pediatric dentistry, implant, dental prosthetics, oral medicine and restorative dentistry) of the King Saud University Dental Hospital. Clinical-surface samples were cultured on Nutrient Agar, to determine the number of colony-forming units (CFU), after incubation for 18–24 h at 37° C.
2.2 Identification of isolated bacteria
Standard microbiological methods according to the protocol of Forbes et al. (2007) were used, including, colony morphology and characteristics. Gram staining was also used, and biochemical tests were done using a Vitek2 automated system.
2.3 Statistical analysis
The results of experiments were shown as the mean ± standard deviation, and all experiments were achieved in triplicate. Data were analyzed using the SPSS statistical software (SPSS Inc., USA), A P-value < 0.05 indicated statistical significance.
3 Results
Table 1 shows the total number of bacterial colonies isolated before and after patient treatment in each specimen in each surface from the various departments. All surfaces located in all departments were contaminated with bacteria. Bacterial contamination ranged between 209 and 644 colony forming units. The Implant Department was the most contaminated, while the Department of Oral Medicine was the less contaminated than other departments. The most common isolated bacteria from the various surfaces sampled were species of Staphylococcus, Streptococcus, Pseudomonas, Bacillus and Micrococcus (Fig. 1).
Clinics
Surfaces
Implant
Mean of 5 pts*
Pedo
Mean of 5 pts
Prosthetic
Mean of 5 pts
Restorative
Mean of 5 pts
Oral Medicine
Mean of 5 pts
Bt**
At***
Bt
At
Bt
At
Bt
At
Bt
At
Dental chair arm rest
62
254
5
64
4
29
4
112
10
33
Floor beneath the dental chair
23
162
32
225
9
80
10
56
12
35
The sink/faucet
5
22
2
75
1
2
22
51
2
27
Towel dispenser
55
213
13
101
3
40
7
35
5
24
Tools table handle
24
132
3
82
6
28
4
13
3
22
Light handle
39
182
3
20
4
55
12
85
7
42
X-ray viewer
52
138
7
123
2
13
10
133
1
5
Paper File
47
116
30
149
5
105
15
100
4
30
Head rest
10
38
42
216
2
143
7
75
13
40
Bench
25
134
2
73
2
24
17
154
9
32
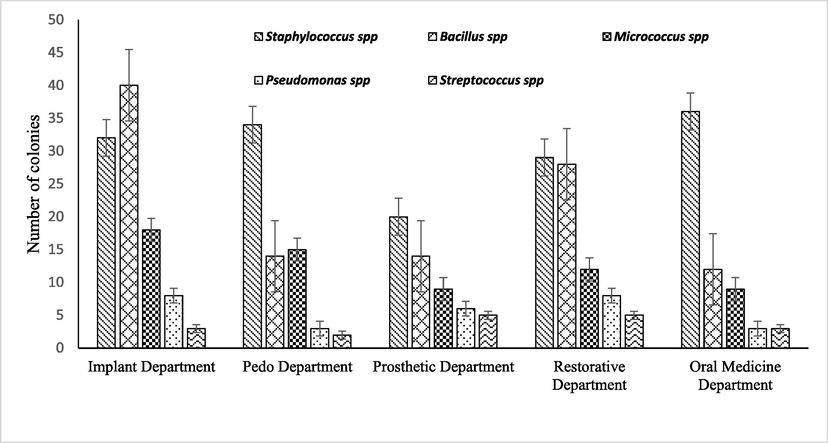
Bacteria isolated from the various dental clinic surfaces.
The results of the present study showed the high prevalence of bacteria on various surfaces located in five departments of a hospital dental clinic. Bacterial contamination was significant after the patient visited various departments for treatment. (Table 1). The results show that the highest bacterial count was found in the Implant Department, this could be due to variety of clinical practices which are performed in this Department compared to others. In contrast, samples from the Department of Oral Medicine showed the lowest number of bacterial isolates; due presumably to the limited number of clinical practices and types of treatments provided at these clinics.
4 Discussion
The results of current study showed that all surfaces of dental clinics before treatment and after treatment of patients were contaminated with bacterial species. A number of studies have reported widespread microbial community in the mouths of dental patients (Spolidorio and Duque, 2013), and doubtless the contamination of dental clinic surfaces occurs because of hand transfer of blood and saliva during patient treatment (Engelmann et al., 2010). In this study, the most common bacteria isolated were species of Staphylococcus, Bacillus, Streptococcus, Pseudomonas and Micrococcus. Staphylococcus aureus is considered to be the most isolated bacteria compared to other bacterial species. S. aureus or Methicillin-resistant Staphylococcus aureus (MRSA) colonization of the oral cavity may be more common than previously thought (Didilescu et al., 2005; Smith et al., 2001). One study of over 5000 oral samples found an MRSA presence of 6% between 1017 S. aureus bacteria isolated (Smith et al., 2003). One other Swedish study linked S. aureus to periodontal-implant infections (Renvert et al., 2008). MRSA colonization rates were compared before and after patients visited each clinic for treatment in study of Faden, (2019). The findings of revealed that the prevalence of MRSA significantly increased after patients visited the area. Also, research Hoshyari et al. (2019) agreed with the current study's findings that there was a notable difference in the frequency of pathogens before and after clinical practice, and Staphylococci were more prominent on the outer surface. Other members of these genera have frequently been shown to be the most commonly isolated bacteria from dental- clinical settings (Coelho et al,. 2016; Castiglia et al,. 2008; Pasquarella et al,. 2010, Witwit et al,. 2019). The presence of such variety of microorganism on theses clinical surfaces mandate the implementation of more powerful decontamination protocol in dental clinics to reduce the risk of cross infection.
Dental clinic is now a health risk for a variety of infections, particularly in immunocompromised individuals (Pankhurst and Coulter, 2007). As a result, several other researchers have emphasized the importance of personal safety systems as well as common disinfection practices in reducing the infection risk related to dental airborne particles (Schel et al., 2006). Domestic infection control standards delineate hygiene measures intended to protect individuals from blood-borne and airborne pathogen transmission Standard warnings for preventing bacterial nosocomial infection spread in the dental hospital (British Dental Association, 2003; Siegel et al., 2007) including hand decontamination before and after contact with each patient, as well as the use of personal safety devices such as mask, robe, gloves and protective glasses. (Baehni et al., 2005; Siegel et al., 2007).
5 Conclusion
Indoor microbial contamination control is especially important because various pathogenic bacteria can be transmitted from the surroundings to patient populations. The aim of the present study was to assess the prevalence of bacteria on ten surfaces in the dental clinics of King Saud University, Dental Hospital, both before and after treatment of selected patients. The results show that all tested surfaces were contaminated with bacteria, with the degree of contamination being considered relatively high for all clinics. The difference in the level of bacterial contamination is due to the type of practice in each setting, with the most frequently isolated bacteria being species of Bacillus, Staphylococcus, Streptococcus, Pseudomonas and Micrococcus. We conclude that the prevalence of these bacteria in dental clinics requires critical attention to the level of disinfection and hygiene used in all clinics.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Floor cleaning: effect on bacteria and organic materials in hospital rooms. J Hosp Infect.. 2009;71(1):57-65.
- [Google Scholar]
- Praxishygiene, Qualitätsleitlinien in der Zahnmedizin. Schweiz. Monatschr. Zahnmed.. 2005;115(no. 7):15-24.
- [Google Scholar]
- Dental Unit waterline microbiology: a cautionary tale. J Can Dent Assoc. 1997;63(10):775-779.
- [Google Scholar]
- Cell phones and Acinetobacter transmission. Emerg. Infect. Dis.. 2005;11:1160-1161.
- [Google Scholar]
- Is your phone bugged? The incidence of bacteria known to cause nosocomial infection on healthcare workers’ mobile phones. J. Hosp. Infect.. 2006;62:123-125.
- [Google Scholar]
- British Dental Association (BDA), 2003. Advice sheet: infection control in dentistry.
- Contamination of the turbine air chamber: a risk of cross infections. J Clin Periodontol. 1998;25(8):607-611.
- [Google Scholar]
- Respiratory pathogens in dental plaque of hospitalized patients with chronic lung diseases. Clin. Oral. Investig.. 2005;9(3):141-147.
- [Google Scholar]
- Evaluation of procedures performed by surgeon-dentists from Cascavel state of Parana and surroundings for biosecurity control. Odontol. Clin. Cient.. 2010;9:161-165.
- [Google Scholar]
- Methicillin-resistant Staphylococcus aureus (MRSA) screening of hospital dental clinic surfaces. Saudi J Biol Sci.. 2019;26(7):1795-1798.
- [Google Scholar]
- Bailey and Scott's Diagnostic Microbiology. St Louis: Mosby. BDA Advice sheet. 2007;al2:19.
- [Google Scholar]
- Microbial bofilm: contamination in dental chair unit. Ind. Med. Gaz.. 2012;145:383-387.
- [Google Scholar]
- Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J. Am. Dent. Assoc.. 2004;135:429-437.
- [Google Scholar]
- Evaluation of Bacterial Contamination in Clinical Environment of Sari Dental School in 2018. J Res Dentomaxillofac Sci.. 2019;4(2):19-25.
- [Google Scholar]
- Infection control practices in dental settings-A review. J. Dent. Allied Scie.. 2012;1:67-71.
- [Google Scholar]
- Guidelines for infection control in dental health-care settings- -2003. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports. 2003 52(Rr-17):1–61
- [Google Scholar]
- Herpesviruses and other microorganisms of concern in dentistry. Dent. Clin. North. Am.. 1991;35:283-298.
- [Google Scholar]
- Do contaminated dental unit waterlines pose a risk of infection? J Dentistry.. 2007;35(9):712-720.
- [Google Scholar]
- Italian multicenter study on microbial environmental contamination in dental clinics: a pilot study. Sci. Total. Environ.. 2010;408:4045-4051.
- [Google Scholar]
- Prevalence and antimicrobial susceptibility pattern of methicillin-resistant Staphylococcus aureus and coagulase-negative Staphylococci in Rawalpindi. Pakistan. Br. J. Med. Med. Res.. 2013;3:198-209.
- [Google Scholar]
- Clinical and microbiological analysis of subjects treated with Branemark or Astra Tech implants: a 7-year follow-up study. Clin. Oral. Implants. Res.. 2008;19:342-347.
- [Google Scholar]
- Comparison of the Efficacies of Disinfectants To Control Microbial Contamination in Dental Unit Water Systems in General Dental Practices across the European Union. Appl Environ Microbiol. 2006;72(2):1380-1387.
- [Google Scholar]
- Isolation of pathogenic Legionella species and Legionella-laden amoebae in dental unit waterlines. J Hosp Infect. 2005;61(3):257-262.
- [Google Scholar]
- The ecology of Staphylococcus species in the oral cavity. J. Med. Microbiol.. 2001;50:940-946.
- [Google Scholar]
- Staphylococcus aureus in the oral cavity: a three-year retrospective analysis of clinical laboratory data. Br. Dent. J.. 2003;195(12):701-703.
- [Google Scholar]
- Microbiology and General and Dental Immunology. São Paulo: Artes Médicas; 2013.
- Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med.. 2007;14:203-207.
- [Google Scholar]
- Surface contamination in the dental operatory: a comparison over two decades. J American Dent. Asso.. 2003;134(3):325-330.
- [Google Scholar]
- A study of personal protection equipment for infection control at dental offices. J. Korean Soc. Dent. Hyg.. 2010;10:459-464.
- [Google Scholar]
- Water characteristics associated with occurrence of Legionella pneumophila in dental units. Eur J Oral Sci. 2000;108:22-28.
- [Google Scholar]







