Translate this page into:
Occupational radiation exposure among diagnostic radiology workers in the Saudi ministry of health hospitals and medical centers: A five-year national retrospective study
⁎Corresponding author. yalashban@ksu.edu.sa (Y. Alashban)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Objectives
To measure and establish a baseline for the annual mean occupational radiological dose for diagnostic radiology workers in Saudi Arabia.
Methods
A retrospective analysis was performed on the effective radiation doses using Thermoluminescent dosimeters for diagnostic radiology workers in Saudi Arabia from 2015 to 2019. They were employed in 412 Saudi Ministry of Health hospitals and medical centers. The diagnostic radiology workers in this study are radiological technologists, radiologists, and medical assistants.
Results
The study population contained 45,152 diagnostic radiology workers (58% male and 42% female). The annual mean effective doses were found to be 0.88 ± 0.002 mSv. Also, 95% of the workers received a radiation exposure dose below 1.60 mSv. The majority of the workers’ effective doses (55%) were frequently laid out between 0.50 and 1.00 mSv. An increase in the collective and mean effective doses have been observed during the study period, with a statistically significant time trend in the mean dose.
Conclusions
During the study period, there was no incidence of an occupational dose exceeding the annual regulatory limits of 20 mSv or the investigation level I. This indicates good implementation of the radiation protection protocols in compliance with ICRP recommendations. However, enhancements in radiation protection practices should be applied for further dose reduction by supplying hospitals and medical centers with the necessary protective equipment.
Keywords
Dose Limit
Radiation Protection
Effective Dose
Occupational Exposure
Ionizing Radiation
- UNSCEAR
-
United Nations Scientific Committee on the Effects of Atomic Radiation
- ICRP
-
International Commission on Radiological Protection
- DRW
-
Diagnostic radiology worker
- MOH
-
Saudi Ministry of Health
- RPP
-
Radiation Protection Program
- TLD
-
Thermoluminescent dosimeter
- SE
-
standard error
- ANOVA
-
An analysis of the variance test
- ALARA
-
As low as reasonably achievable
Abbreviations
1 Introduction
Advances in medical imaging technologies using ionization radiation have brought health risk concerns to the fore (Prasad et al., 2004). On the one hand, the use of radiation as a diagnostic tool may have led to substantial radiation exposures to radiologists, technologists, nurses, and medical assistants (Vano et al., 1988; Yoshinaga et al., 2004). On the other hand, the advances in technologies in radiation imaging and therapy have helped to increase the precision of the medical diagnosis and treatment.
Radiation protection authorities have a responsibility of assessing occupational radiation doses after a low and prolonged exposure to ionization radiation (Cardis et al., 2005; Ciraj-Bjelac et al., 2010; Miller et al., 2010).
Worldwide, medical radiation personnel account for 75% of the exposed workers to ionizing radiation (UNSCEAR, 2008). Over the last three decades, there has been an increase in occupational radiation doses due to utilization of diagnostic imaging in cancer assessment (Fazel et al., 2009). According to the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR), the annual number of radiological examinations around the world increased from 1380 million in 1988 to 3143 million in 2008. The annual collective effective dose (1000 man-Sv) also increased from 1800 million in 1988 to 4000 million in 2008 (UNSCEAR, 2008).
The recognition of radiation hazards to medical workers has led to occupational radiation monitoring (Weizhang et al., 2005; Freedman et al., 2003), and resulted in many experimental studies that have linked it to the mortality and cancer risk induced with radiation exposure (Muirhead et al., 2009; Martins et al., 2007; Piwowarska-Bilska et al., 2008; Piwowarska-Bilska et al., 2010; Szewczak et al., 2013). The related health risks include, but are not limited to: lung cancer, thyroid cancer, ovarian cancer, melanoma, breast cancer, leukemia, and rectum cancers (Sont et al., 2001).
The International Commission on Radiological Protection (ICRP) expressed occupational radiation dose in terms of effective dose and equivalent dose. The effective dose is the dose to the whole body, while the equivalent dose is the dose to the skin, extremities, and lens of the eyes. The annual effective dose limit set by ICRP is 20 mSv, with a limit of 100 mSv in five years. The equivalent dose limit for skin and extremities is 500 mSv, and 20 mSv for the eye lenses (IAEA, 1996; ICRP, 1991, 2012).
This study aims to assess and establish a baseline for the annual occupational dose for diagnostic radiology workers in Saudi Arabia, and compare it with the recommended ICRP dose limits.
2 Materials and Methods
A retrospective analysis was performed on the effective radiation doses for diagnostic radiology workers (DRWs) in Saudi Arabia for a period of five years (2015–2019). The workers were employed in 412 Saudi Ministry of Health (MOH) hospitals and centers in all of the Saudi administrative regions. These workers were employed in general x-ray, computed tomography, fluoroscopy, and mammography departments. The Radiation Protection Program (RPP) operates as a national register and regulator of occupational radiation doses for all medical centers’ work under the umbrella of the MOH. All the DRWs were issued personal bar-coded whole-body Thermoluminescent dosimeter (TLD-100), and were recommended to wear them at chest level under the lead apron. The bar-coded TLDs contain workers’ name, age, and the period of use. These TLDs consist of lithium fluoride doped with magnesium and titanium (LiF:Mg,Ti) materials. The TLD reading system consist of a 90Sr/90Y irradiator, a Harshaw 6600 plus reader (Thermo Electron Corporation, Ohio, USA), and WinREMS software. The reader has sensitivity that ranged from 10 μGy to 1 Gy with a minimum detectable limit of 10 μGy. All the workers in this study were monitored in a calendar quarterly basis. The DRWs in this study are radiological technologist, radiologists, and medical assistants. However, the database of the RPP do not specify the occupational position of each worker. Therefore, this study focuses on the effective dose for the diagnostic radiology personnel in general.
All statistical assessments were performed using the software Statistical Package for the Social Sciences (version 20; SPSS‑Inc; New York, USA) at a confidence level of 95%.
3 Results
The study population contained 45,152 diagnostic radiology workers (58% male and 42% female), who enrolled in MOH from 2015 to 2019. The number of diagnostic radiology workers, their annual mean effective dose (mSv) with standard error, their annual standard deviation, and annual collective effective dose (man-mSv) are listed in Table 1.
Year
2015
2016
2017
2018
2019
Number of workers
7419
8476
8990
9696
10,571
Annual effective dose (mSv)
Mean ± SE
0.71 ± 0.006
0.78 ± 0.006
0.84 ± 0.005
0.98 ± 0.005
1.02 ± 0.005
Standard deviation
0.51
0.59
0.51
0.51
0.58
Collective(man-mSv)
5295
6624
7607
9555
10,875
The annual mean effective dose averaged over the period of five years was found to be 0.88 ± 0.002 mSv, with a standard deviation of 0.56 mSv. Also, the collective effective doses averaged over the period of five years were found to be 39,955 man-mSv.
The RPP adopted three investigation levels, which are used as trigger points above which a certain decision should be taken. These levels are operational level (MDL − 1.25 mSv), level I (1.25–3.75 mSv), and level II (>3.75 mSv) per calendar quarter. Table 2 shows the percentage of workers in each investigation level. The RPP policy states that if workers exposed to doses below level I, no action will be taken. However, workers who exposed to a level I doses, a warning is issued without any further actions. Also, there are disciplinary penalties for workers who exposed to a level II doses and these penalties include warning, fine, and medical license suspension.
Investigation Level
Operational
Level I
Level II
Dose interval
MDL − 1.25 mSv
1.25–3.75 mSv
> 3.75 mSv
Percentage of workers
99.7%
0.3%
0%
4 Discussion
Fig. 1 shows the percentiles distribution graph for the effective dose for all workers during the study period. It shows that 95% (n = 42895) of all workers received a radiation exposure dose below 1.60 mSv. The frequency of the effective doses for all workers combined is illustrated in Fig. 2. The results show that the majority of the workers’ effective doses (55%) were frequently laid out between 0.50 and 1.00 mSv.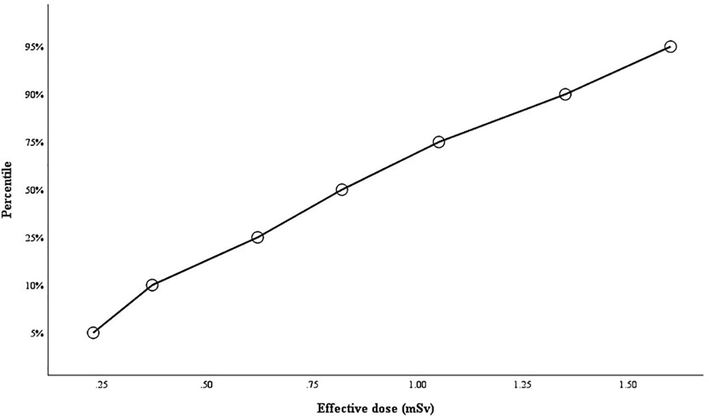
Percentiles distribution graph for the effective dose for all of the workers during the study period.
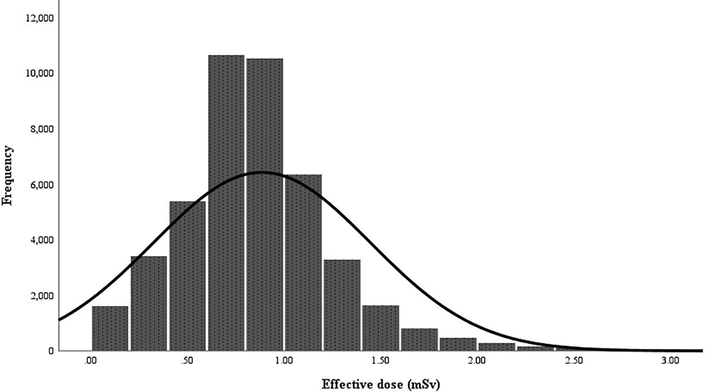
Frequency of the effective dose for all workers combined during 2015–2019 with the normal distribution curve.
An analysis of the variance test (one-way ANOVA) was conducted to determine if there were statistically significant differences in the mean effective dose during the study period. The means plot illustrated in Fig. 3 and the test reveals statistically significant differences in the effective doses between the study’s years (F (4,45147) = 531, p = 0.00). Also, the tests of homogeneity of variances and robust tests of equality of means (Welch and Brown-Forsythe) show statistically significant differences in the dose during the study period (p
0.05). The DRWs in 2019 were exposed to the highest annual collective dose compared to the workers in previous years. This is mainly due to an increase in the number of workers. Likewise, the DRWs in 2019 were exposed to the highest annual effective dose due to an increase in the diagnostic radiological procedures.
Mean annual effective dose during 2015–2019.
The study shows that>99% of the DRWs received an exposure dose within the operation level and therefore no action was taken by the RPP. The rest of the workers (<1%) received an exposure within Level I. For the DRWs whose doses were within Level I, the RPP alerted the radiation safety officer at the specific hospital or medical center for an increase in the radiation exposure while mentioning the names of DRWs exposed without taking any penal action. It is important to mention that there were a few workers during the whole study period who intentionally exposed their TLDs to radiation and therefore their data was excluded from the study.
During the five-year study period, there was no incidence of an occupational dose exceeding the annual regulatory limit of 20 mSv or the investigation level I adopted by the RPP. This indicates a proper implementation of the radiation protection protocols in compliance with ICRP recommendations. However, occupational radiation exposure should continuously remain as low as is reasonably achievable (ALARA).
A 2016 study in Saudi Arabia found that the majority of the national hospitals were equipped with lead aprons and thyroid shields. However, around 50% of these hospitals have protective lead glasses and sheets (Salama et al., 2016). Lead aprons and thyroid shields are the most effective types of shielding in terms of radiation reduction (>95% reduction). However, there is a need to supply all the MOH hospitals with lead glasses (35–90% reduction), gloves (20–50% reduction), and surgical caps (3.3% reduction) (Kim and Miller, 2009).
When comparing the mean doses obtained in this study with those in Table 3, it can be noticed that the occupational doses in this study are within the range of other studies in the literature.
Time period
Country
Average effective dose (mSv)
2012–2013
South Korea
1.80
2009
Japan
0.93
2007–2011
Pakistan
0.52
2011–2013
Lithuania
0.62
2008–2009
Kuwait
1.05
2000–2009
Ghana
1.05
2015–2019
Saudi Arabia (current study)
0.88
5 Conclusion
The study aims to establish a baseline for DRWs’ radiation doses in Saudi Arabia. The annual mean averaged over the period of five years was found to be 0.88 ± 0.002 mSv. Also, 95% of all workers received a radiation exposure dose below 1.60 mSv. The majority of workers’ effective doses (55%) were frequently laid out between 0.50 and 1.00 mSv. The annual effective doses were way below the limits established by national and international legislations, which indicates a good implementation of the radiation protection protocols in compliance with ICRP recommendations. However, enhancements in radiation protection practices should be applied for further dose reduction by supplying hospitals and medical centers with all of the necessary protective equipment.
Acknowledgement
Author extend their appreciation to the College of Applied Medical Sciences Research Center and Deanship of Scientific Research at King Saud University for funding this project.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Occupational Radiation Exposure among the Staff of Departments of Nuclear Medicine and Diagnostic Radiology in Kuwait. Med. Princ. Pract.. 2014;23(2):129-133.
- [Google Scholar]
- Risk of cancer after low doses of ionising radiation: retrospective cohort study in 15 countries. BMJ. 2005;331(7508):77.
- [CrossRef] [Google Scholar]
- Risk for radiation-induced cataract for staff in interventional cardiology: Is there reason for concern? Cathet. Cardiovasc. Intervent.. 2010;76(6):826-834.
- [Google Scholar]
- Occupational Dose in Interventional Radiology Procedures. Am. J. Roentgenol.. 2013;200(1):138-141.
- [Google Scholar]
- Risk of melanoma among radiologic technologists in the United States. Int. J. Cancer. 2003;103(4):556-562.
- [Google Scholar]
- Exposure to Low-Dose Ionizing Radiation from Medical Imaging Procedures. N. Engl. J. Med.. 2009;361(9):849-857.
- [Google Scholar]
- Assessment of annual whole-body occupational radiation exposure in medical practice in Ghana (2000-09) Radiat. Prot. Dosim.. 2012;149(4):431-437.
- [Google Scholar]
- ICRP, 1991. 1990 recommendations of the International Commission on Radiological Protection, Ann. ICRP. 60, 2–4.
- IAEA, 1996. International basic safety standards for protection against ionizing radiation and for safety of radiation sources. Safety Series No. 115, 1–30.
- ICRP, 2012. ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs–threshold doses for tissue reactions in a radiation protection context. Ann. ICRP, 01−322.
- Minimising radiation exposure to physicians performing fluoroscopically guided cardiac catheterisation procedures: a review. Radiat. Prot. Dosim.. 2009;133(4):227-233.
- [Google Scholar]
- J. Kim E.S. Cha Y. Choi W.J. Lee WORK PROCEDURES AND RADIATION EXPOSURE AMONG RADIOLOGIC TECHNOLOGISTS IN SOUTH KOREA 178 4 2018 2018 345 353 https://academic.oup.com/rpd/article/178/4/345/4098856.
- M.B. Martins J.G. Alves J.N. Abrantes A.R. Roda Occupational exposure in nuclear medicine in Portugal in the 1999-2003 period Radiation Protection Dosimetry 125 1-4 130 134 10.1093/rpd/ncl564 https://academic.oup.com/rpd/article-lookup/doi/10.1093/rpd/ncl564.
- Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers. Br J Cancer. 2009;100(1):206-212.
- [Google Scholar]
- Occupational Radiation Protection in Interventional Radiology: A Joint Guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc. Intervent. Radiol.. 2010;33(2):230-239.
- [Google Scholar]
- Assessment of Occupational Exposure Among Pakistani Medical Staff During 2007–2011. Australas Phys. Eng. Sci. Med.. 2012;35(3):297-300.
- [Google Scholar]
- Health Risks of Low Dose Ionizing Radiation in Humans: A Review. Exp. Biol. Med. (Maywood). 2004;229(5):378-382.
- [Google Scholar]
- Long-term monitoring of radiation exposure of employees in the department of nuclear medicine (Szczecin, Poland) in the years 1991-2007. Radiat. Prot. Dosim.. 2010;140(3):304-307.
- [Google Scholar]
- W.N. Sont J.M. Zielinski J.P. Ashmore H. Jiang D. Krewski M.E. Fair P.R. Band E.G. Létourneau First Analysis of Cancer Incidence and Occupational Radiation Exposure Based on the National Dose Registry of Canada 153 4 2001 2001 309 318.
- K. Szewczak S. Jednoróg P. Krajewski Individual dose monitoring of the nuclear medicine departments staff controlled by Central Laboratory for Radiological Protection Nucl. Med. Rev. 16 2 62 65 10.5603/NMR.2013.0036 http://czasopisma.viamedica.pl/nmr/article/view/35439.
- Assessment of annual average effective dose status in the cohort of medical staff in Lithuania during 1991–2013. Radiat. Prot. Dosimet.. 2015;167(4):671-677.
- [Google Scholar]
- Salama, K.F., AlObireed, A., AlBagawi, M., AlSufayan, Y., AlSerheed, M., 2016. Assessment of occupational radiation exposure among medical staff in health-care facilities in the Eastern Province, Kingdom of Saudi Arabia. Indian. J. Occup. Environ. Med. 20, 21. https://dx.doi.org/10.4103%2F0019-5278.183832
- UNSCEAR, 2008. Sources and effects of ionizing radiation. Volume I. United Nations, New York.
- W.u. Weizhang Z. Wenyi C. Ronglin Z. Liang'an Occupational exposures of Chinese medical radiation workers in 1986–2000 117 4 2005 2005 440 443 http://academic.oup.com/rpd/article/117/4/440/1673505/Occupational-exposures-of-Chinese-medical.
- Cancer Risks among Radiologists and Radiologic Technologists: Review of Epidemiologic Studies. Radiology. 2004;233(2):313-321.
- [Google Scholar]







