Translate this page into:
Occupational radiation dose assessment for nuclear medicine workers in Turkey: A comprehensive investigation
⁎Corresponding authors. welshami@sharjah.ac.ae (Wiam Elshami), ruerdemir@beun.edu.tr (R. Uslu Erdemir)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Objective
Radioisotopes are used extensively in nuclear medicine. Analysis of occupational doses received by medical radiation workers, especially nuclear medicine staff dealing with radioisotopes, contributes significantly to enhancing safe practice and promoting radiation protection measures in the radiology department. The current study aimed to determine the time trend and the differences in occupational radiation dose among nuclear medicine workers.
Methods
Readings of 394 OSL dosimeters were obtained from 31 medical workers and grouped into five worker groups (technologist, physician, nurse, radio-pharmacist, and radio-physicist).
Results
The average number of workers dropped to 4.5 in 2020 and 2021 compared to 14.4 in 2014 to 2019. The average annual effective dose and skin dose for all workers based on measurements for a typical yearly workload of 5000 patients were 1.21 (±1.15) mSv and 2.86 (±1.32) mSv, respectively. The highest average annual effective and skin dose was 5.41 and 5.82 mSv, respectively. The NM technologist working in PET/CT received higher mean and maximum effective and skin doses than the other worker groups.
Conclusion
The annual effective and skin doses were below the national legislation and international standards. However, improvements in radiation protection practices could be implemented to reduce occupational radiation dose to NM technologists, the most exposed worker group in this study.
Keywords
Nuclear medicine
PET CT
Occupational radiation dose
Radiation protection
OSL
Radiation
1 Introduction
The number of Nuclear Medicine (NM) investigations performed worldwide has increased rapidly in the past decades. For example, studies showed that NM examination increased by 2.5-fold between 1980 and 2006, increasing the effective dose by 600% (Adliene et al., 2020). The term “occupational dose” refers to workers being exposed to ionizing due to procedures within their workplace. Radiation workers, including workers in the medical field, should follow radiation protection standards established by international organizations (Dalah et al., 2018). The limit of occupational radiation exposure dose established by the International Commission on Radiological Protection (ICRP) to be 20 mSv/year, averaged over any five years, for occupational exposure provided that the individual dose does not exceed 50 mSv in any single year (ICRP, 2007). There is a piece of tolerable scientific evidence about occupational exposure on radiology, conventional NM and interventional radiology, but it is limited among NM staff during PET imaging (Alnaaimi et al., 2017). The ICRP and studies reported that NM staff might be at risk from occupational exposure (Clement, 2011; Rehani et al., 2011).
The increased use of hybrid has raised many radiation safety issues. Positron Emission Tomography (PET) has been a frequently utilized diagnostic tool for assessing vascular disorders and cancer over the last 15 years (Bernier et al., 2018). Radiation exposure to PET technologists has increased due to this growth, resulting in an increase in their total occupational radiation exposure (Antic et al., 2014). The literature showed evidence that a reversible and irreversible genotoxic effect increased with radiation exposure (Azizova et al., 2018). In addition, occupational exposure of NM workers is associated with biological effects, which increase with the workload and time (Al-Abdulsalam and Brindhaban, 2014). Chronic exposure to low doses of ionising radiation increases the risk of long term effect that might appear in a time of several years after the initial exposure. Studies showed increased risk of cancer, chromosomal aberrations and cytogenetic damage among NM workers (Adliene et al., 2020). As a result, estimating radiation doses for radiation workers is critical for assessing radiation risks and developing protective measures for governments and international organizations. Nevertheless, assessment of occupational dose is documented internationally and in Turkey (Alnaaimi et al., 2017; Bernier et al., 2018; Gunduz et al., 2004; Söylemez et al., 2012; Zeyrek and Gündüz, 2005), but fewer studies have been performed in NM (Bayram et al., 2011). The presence of significant research in the literature, performed in accordance with the ALARA principle and aimed at optimizing radiation worker safety measures, prompted us to conduct this study. We aimed to assess the occupational radiation dose for nuclear medicine workers, including PET/CT workers and determine the differences in the radiation dose level among workers. Accordingly, extensive occupational radiation dose assessments were performed for all occupational groups such as nuclear medicine physicians, nurses, radiographers, radio-pharmacists, radio-physicists working in the nuclear medicine facilities. The findings of this research have the potential to make significant additions to the literature by elucidating the dosage amount to which various professional groups operating in the same area are exposed depending on the number of performed examinations and other variables.
2 Method
This is a retrospective study that analyzed the occupational exposure for working in NM and PET CT. Whole-body dose (Hp 10) and skin dose (Hp 0.07) for various groups of medical radiation workers working in nuclear medicine and PET CT in large Turkish hospital have been analyzed (2014–2021). The typical annual workload in the NM department is 5000 patients (22 patients/day). Radiation dose records for 31 radiation medical workers were retrieved from the occupational radiation dosimetry service. Workers included in the study were radiographer/radiologic technologist in NM and PET CT, physicians, nurses, radio-pharmacist and radio-physicist. In this study, optically stimulated luminescence (OSL) dosimeter was used. OSL dosimeters are designed to provide measurement of X, gamma, beta and neutron radiation m. The OSL dosimeter provides a very high degree of sensitivity and applied commonly to monitor accumulated dose. Therefore, it is ideal for monitoring medical radiation workers. The validation method was used according to the TS-EN-62387 standard. As the decision rule; it has been applied with reference to the IAEA Safety Guide No: RS-G-1.3 document (Uc ≤ 0.21). The basic properties of the used OSL dosimeter were sensitivity = 0.1 mSv (up to: 10 Sv), detection range: 25 keV – 1.25 MeV and operating temperature: 0–50 Celsius degree. All workers used OSL to measure the Hp(10) and Hp(0.07) every three months. OSL is worn under the lead apron. The whole-body dose is reported as a personal dose equivalent Hp(10) recommended by the International Commission on Radiation Units and Measurement. The personal dose equivalent Hp(10) estimates the effective dose for those photon energies used in radiology when incident on the front of the body (Vañó et al., 1998). Thus, the Hp(10) is used directly, without any conversion factor or formula, when estimating the annual effective dose.
Statistical analysis all data were grouped into categories based on the occupation. Data were collected, categorized, and processed using Statistical Package for Social Sciences (SPSS), software package version 25. The quantitative variables were expressed as mean ± Standard Deviation (SD). The current study is quality improvement research; therefore, it was exempted from ethical approval.
3 Results
A total of 394 OSL readings for 31 workers were acquired from 2014 to 2021. Fifty-eight percent of the worker were radiographers (n = 18); of them, 14 were working in PET/CT and four working in NM, 7% (n = 7) were radio-pharmacist, and 3% (n = 1) were radio-physicist (Table 1). The average number of workers was 11.8 throughout the study period. The number of workers ranged from 10 to 16 in the years from 2014 to 2019. Nevertheless it dropped to 4 to 5 in 2020 and 2021 (Fig. 1).
Occupation
N
%
Radiographer (NM and PET CT)
18
58.1%
NM physicians
5
16.1%
Nurse
5
16.1%
Radio-pharmacist
2
6.5%
Radio-physicist
1
3.2%
Total
31
100.0%
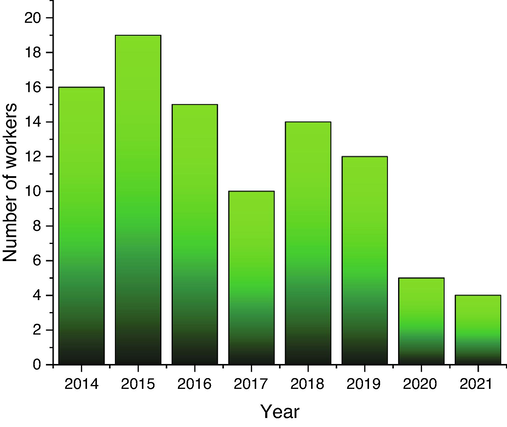
The total number of NM workers per year (2014–2021).
The average annual effective dose for all workers based on measurements for a typical yearly workload of 5000 patients was 1.21 (±1.15) mSv. The average annual effective dose for all workers throughout the study period ranged from 0.69 mSv (in 2016) to 2.83 mSv (in 2020) (Fig. 2). The average annual skin dose for all workers based on measurements for a typical yearly workload of 5000 patients was 2.86 (±1.32) mSv. The average annual skin dose for all workers throughout the study period ranged from 0.71 mSv (in 2017) to 2.97 mSv (in 2020) (Fig. 3).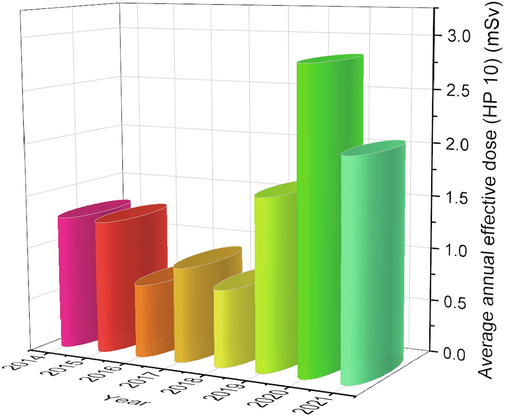
Average annual effective dose (HP 10) in mSv for medical workers per year (2014–2021).
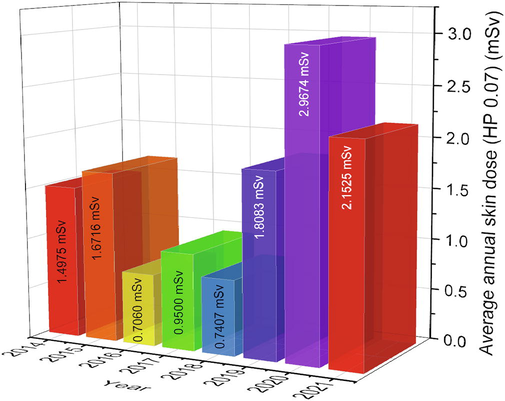
Average annual skin dose (HP 0.07) in mSv for medical workers (2014–2021).
The average annual effective dose and the standard deviation was calculated for each workers group. Table 2 shows that radiographers in PET/CT had the highest average annual effective dose compared to other occupations throughout the study period (Table 2). The yearly analysis showed that the highest dose was 5.41 mSv for a PET/CT radiographer in 2019. Similarly, in Table 3, the highest average annual skin dose was 5.82 mSv for a PET/CT radiographer in 2019 (Table 3). It shows the total number of workers decreased dramatically in 2020 and 2021. The average number of workers from 2014 to 219 and from 2020 to 2021 was 14.3 and 4.5, respectively. The average annual effective dose and skin dose are affected by number of workers because of the workload (Table 4).
HP10
Average
Max
Min
SD
Physicians
0.83
1.75
0.37
0.47
Nurse
0.59
1.30
0.16
0.33
Radiographer PET/CT
2.00
5.41
0.10
1.31
Radiographer NM
0.35
0.79
0.07
0.31
Radio-pharmacist
0.68
1.01
0.07
0.27
Radio-physicist
1.44
2.32
0.99
0.68
All
1.21
5.41
0.07
1.15
HP7
Average
Max
Min
SD
Physicians
0.89
1.80
0.36
0.53
Nurse
0.61
1.67
0.14
0.41
Radiographer ET/CT
5.34
5.82
0.10
1.46
Radiographer NM
0.62
3.27
0.06
0.96
Radio-pharmacist
0.59
2.25
0.06
0.54
Radio-physicist
2.26
3.19
0.95
1.04
All
2.86
5.82
0.06
1.32
Year
2014
2015
2016
2017
2018
2019
2020
2021
workload
2212
2719
6126
6678
7396
6711
3962
4818
workload PET CT
2212
2719
2895
3098
4085
4237
3626
3622
workload NM
0
0
3231
3580
3311
2474
336
1196
Number of workers
16
19
15
10
14
12
5
4
Average annual effective dose
1.27
1.26
0.69
0.90
0.73
1.62
2.83
2.05
Average Annual Skin Dose
1.50
1.67
0.71
0.95
0.74
1.81
2.97
2.15
Figs. 4 and 5 illustrate the distribution of dosimeter measurements for annual effective and skin doses. The majority of measurements were below 2 mSv annual effective and skin doses.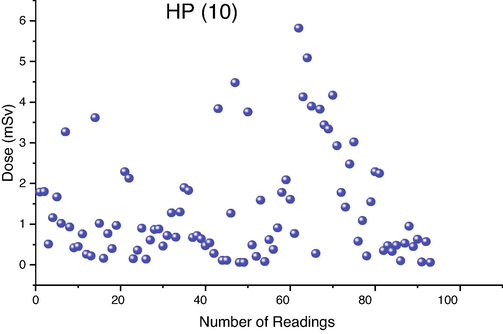
Distribution of average annual effective (HP 10) in mSv for all workers (2014–2021).
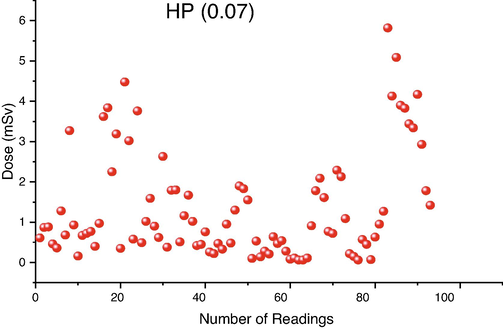
Distribution of annual skin dose (HP 0.07) in mSv for all workers (2014–2021).
4 Discussion
In the last few years, previous studies showed growth in the number of workers and the collective dose (Elshami et al., 2020; Miller, 2008; UNSCEAR, 2008). Nevertheless, the finding of this study showed a heterogeneous finding relating to the number of radiation medical workers and average annual dose for all workers. Reduction in the number of radiation medical workers in NM and PET CT in 2020 and 2021 might be due to the COVID-19 pandemic as there was a work adjustment in many radiology department globally (Cavli et al., 2021; Elshami et al., 2021). The reduction in workers is accompanied with increase in the average annual effective dose (HP 10) and average annual skin dose (HP 0.07) as seen in Figs. 2 and 3, respectively. In the current study, the workload was minimally affected by COVID-19 and the average number of patients remained comparable to pre COVID-19 (Table 4). Studies have found that the number of referrals to NM services showed reduced but referral to PET CT was not affected with COVID-19 as they were not viewed as elective procedures (Currie, 2020). PET CT has a great contribution to occupational radiation and usually workers in PET CT demonstrate higher doses (Li et al., 2020). The increase in the annual effective dose demonstrated in the year 2020 and 2021 can be due to less workers performing the same workload.
Table 5 shows the current result of occupational radiation dose as compared to different countries. The maximal estimated annual whole-body dose (5.4 mSv) was higher compared to some countries such as in Serbia the recorded whole-body doses were 3.4 mSv (Antic et al., 2014) and (4.0 mSv) in Kuwait (Alnaaimi et al., 2017). Nevertheless, the extremity dose was lower (5.82 mSv) compared to (45 mSv) in Serbia (Antic et al., 2014) and (120 mSv) in Kuwait (Alnaaimi et al., 2017). However, the current study found that, throughout the study period, the average annual effective and skin doses are less than the local authority and the international limits set by the ICRP, it was higher compared to Australia, Denmark, Finland, Germany, and some countries in the UNSCEAR Report 2000. Nevertheless, it was lower than Canada, China, and Spain (UNSCEAR, 2000). It was expected that radio-pharmacist working in the hot labs received the higher dose as reported in some studies (Alnaaimi et al., 2017; Antic et al., 2014), but the findings of the current study showed that radiographers working in PET/CT received the highest whole body and skin dose compared to radio-pharmacist. The present study demonstrated that the maximum annual whole-body dose is less than the 3.4 and 2.0 mSv which were reported in previous studies. Similarly, the highest annual skin dose is less compared to 45 mSv in previous studies (Antic et al., 2014; Dalianis et al., 2006). It was found that radiographers performing injection regardless of the automatic infusion system usually received the highest radiation exposure dose (Skovorodko et al., 2020). It is uncommon that radiographers receive higher dose compared to other professionals (Elshami et al., 2019). It is worth mentioning that the use of automatic injection/infusion systems showed a significant reduction of whole body and extremities radiation exposure, but radiographers reported higher doses (Al-Abdulsalam and Brindhaban, 2014). The higher dose reported for radiographers might be due to patient positioning as it contributes to 51.1% of the whole-body dose compared to 41.5% of the dose from radiopharmaceutical injection (Martins et al., 2007). It is critical to categorize radiation workers for appropriate safety procedures and to foster a radiation protection culture. Analysis of occupational radiation dose can lead to innovative ways to reduce radiation exposures (Kortesniemi et al., 2017). It is imperative to evaluate and improve all radiation protection measures (Abuzaid et al., 2018). Similarly, assessment of radiation protection practice can provide a guide to enhancing radiation safety measures. An emphasis should be placed on protecting radiographers since they are among the most exposed workers. *NA, Not available.
Annual dose (mSv)
Country
NM physicians
Nurse
NM technologist
Current study
Turkey
0.83 ± 0.47 (1.75–0.37)
0.59 ± 0.33 (1.30–0.16)
1.63 ± 1.33 (5.41–0.07)
(Alnaaimi et al., 2017)
Kuwait
2.8
3.2
2.4
(Piwowarska-Bilska et al., 2011)
Poland
0.1
4.0
0.6
(Antic et al., 2014)
Serbia
NA
NA
3.4
(Benatar et al., 2000)
UK
NA
NA
6.0
(Martins et al., 2007)
Portugal
0.79–1.39
2.73–3.18
2.45–3.45
(Lundberg et al., 2002)
Australia
NA
NA
1.4
(Al-Abdulsalam and Brindhaban, 2014)
Kuwait
1.01 ± 0.03 (0.08– 3.43)
1.00 ± 0.01 (0.08– 2.85)
NA
(Al-Haj and Lagarde, 2002)
Saudi Arabia
NA
NA
0.5–1.2
(Weizhang et al., 2005)
China
NA
NA
1.2–1.6
5 Conclusion
The radiation doses received by NM workers were assessed. In view of current practice and workload, all effective radiation doses received by workers were well below the dose limits recommended by the ICRP. Nevertheless, radiation dose optimization measures, particularly for radiographers, are still needed to occupational exposure, such as employing suitable shielding, automating injecting systems, and reducing time spent during patient injections.
On the other hand, the study showed reduction in workers in NM and PET CT in 2020 and 2021 combined with increase in the annual effective dose. Continuous monitoring and evaluation of occupational radiation is recommended to promote safe practice.
5.1 Limitation of the study
A limitation of the study is the small number of monitored radiopharmacist and radiophysicists. Also, compliance with ideal dose monitoring and radiation protection is not accounted for in the analysis of this study. It is important to assess the to ensure safe practice (Abuzaid et al., 2019). Future studies focus on the assessment of compliance to monitoring and radiation protection practice is recommended.
Conflict of interest
All authors declare that they have no conflict of interests.
References
- Knowledge and Adherence to Radiation Protection among Healthcare Workers at Operation Theater. Asian J. Sci. Res.. 2018;12:54-59.
- [CrossRef] [Google Scholar]
- Assessment of compliance to radiation safety and protection at the radiology department. Int. J. Radiat. Res. 2019
- [Google Scholar]
- Occupational radiation exposure of health professionals and cancer risk assessment for Lithuanian nuclear medicine workers. Environ. Res.. 2020;183:109144.
- [Google Scholar]
- Occupational radiation exposure among the staff of departments of nuclear medicine and diagnostic radiology in Kuwait. Med. Princ. Pract.. 2014;23:129-133.
- [CrossRef] [Google Scholar]
- Statistical analysis of historical occupational dose records at a large medical center. Health Phys.. 2002;83:854-860.
- [CrossRef] [Google Scholar]
- Occupational radiation exposure in nuclear medicine department in Kuwait. Radiat. Phys. Chem.. 2017;140:233-236.
- [CrossRef] [Google Scholar]
- Radiation exposure to nuclear medicine staff involved in PET/CT practice in Serbia. Radiat. Prot. Dosimetry. 2014;162:577-585.
- [CrossRef] [Google Scholar]
- Risk of malignant skin neoplasms in a cohort of workers occupationally exposed to ionizing radiation at low dose rates. PLoS One. 2018;13(10):e0205060.
- [Google Scholar]
- undefined, 2011. Radiation dose to technologists per nuclear medicine examination and estimation of annual dose. Soc. Nucl. Med. 2011;39(1):55-59.
- [Google Scholar]
- Radiation dose rates from patients undergoing PET: implications for technologists and waiting areas. Eur. J. Nucl. Med.. 2000;27:583-589.
- [CrossRef] [Google Scholar]
- Work history and radioprotection practices in relation to cancer incidence and mortality in US radiologic technologists performing nuclear medicine procedures. Occup. Environ. Med.. 2018;75:533-561.
- [CrossRef] [Google Scholar]
- Coronavirus disease 2019 strategies, examination details, and safety procedures for diagnostic radiology facilities: an extensive multicenter experience in Istanbul. Turkey. J. Radiol. Nurs.. 2021;40:172-178.
- [CrossRef] [Google Scholar]
- Clement, C., 2011. International Commission on Radiological Protection The International Commission on Radiological Protection (ICRP) in cooperation, icrp.org.
- Post–COVID-19 new normal for nuclear medicine practice: an Australasian perspective. J. Nucl. Med. Technol.. 2020;48:234-240.
- [CrossRef] [Google Scholar]
- Occupational doses to cardiologists performing fluoroscopically-guided procedures. Radiat. Phys. Chem.. 2018;153:21-26.
- [Google Scholar]
- Dosimetric evaluation of the staff working in a PET/CT department. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip.. 2006;569:548-550.
- [CrossRef] [Google Scholar]
- Occupational Dose and Radiation Protection Practice in Uae: a Retrospective Cross-Sectional Cohort Study (2002–2016) Radiat. Prot. Dosimetry. 2019;187:426-437.
- [CrossRef] [Google Scholar]
- Estimation of occupational radiation exposure for medical workers in radiology and cardiology in the United Arab Emirates: nine hospitals experience. Radiat. Prot. Dosimetry. 2020;189:466-474.
- [CrossRef] [Google Scholar]
- The radiology workforce’s response to the COVID-19 pandemic in the Middle East, North Africa and India. Radiography. 2021;27:360-368.
- [CrossRef] [Google Scholar]
- Occupational exposure to ionising radiation in the region of anatolia, turkey for the period 1995–1999. Radiat. Prot. Dosimetry. 2004;108:293-301.
- [CrossRef] [Google Scholar]
- ICRP, 2007. ICRP 103: The 2007 Recommendations of the International Commission on Radiological Protection. Ann. ICRP 37, 330. https://doi.org/10.1016/j.icrp.2007.10.001
- Kortesniemi, M., Siiskonen, T., … A.K.-R. protection, 2017, undefined, 2017. Actual and potential radiation exposures in digital radiology: analysis of cumulative data, implications to worker classification and occupational exposure monitoring. academic.oup.com 174, 141–146. https://doi.org/10.1093/rpd/ncw099
- Exposure doses to technologists working in 7 PET/CT departments. Dose. Response. 2020;18
- [CrossRef] [Google Scholar]
- undefined, 2002. Measuring and minimizing the radiation dose to nuclear medicine technologists. Soc. Nucl. Med.. 2002;30:25-30.
- [Google Scholar]
- Occupational exposure in nuclear medicine in Portugal in the 1999–2003 period. Radiat. Protect. Dosimetry 2007:130-134.
- [CrossRef] [Google Scholar]
- Overview of contemporary interventional fluoroscopy procedures. Health Phys.. 2008;95(5):638-644.
- [Google Scholar]
- Occupational exposure at the department of nuclear medicine as a work environment: A 19-year follow-up. Polish J. Radiol.. 2011;76:18-21.
- [Google Scholar]
- Occupational exposure in a PET/CT facility using two different automatic infusion systems. Phys. Medica. 2020;77:169-175.
- [CrossRef] [Google Scholar]
- Radiation exposure-do urologists take it seriously in Turkey? J. Urol.. 2012;187:1301-1305.
- [CrossRef] [Google Scholar]
- United Nations Scientific Committee on the Effects of Atomic Radiation. In: Sources and effects of ionizing radiation 2000 Report. 2000.
- [Google Scholar]
- UNSCEAR, 2008. Report of the United Nations Scientific Committee on the Effects of Atomic Radiation: Fiftysixth Session.
- Radiation exposure to medical staff in interventional and cardiac radiology. Br. J. Radiol.. 1998;71:954-960.
- [CrossRef] [Google Scholar]
- Occupational exposures of Chinese medical radiation workers in 1986–2000. Radiat. Prot. Dosimetry. 2005;117:440-443.
- [CrossRef] [Google Scholar]
- Occupational exposure to ionizing radiation with thermoluminescence dosimetry system in Turkey, In 2003. Radiat. Prot. Dosimetry. 2005;113:374-380.
- [CrossRef] [Google Scholar]







