Translate this page into:
Evaluation of BioVue Column Agglutination Technology for quality control purpose of therapeutic anti-Rh immunoglobulin preparations
*Address: Biology Dept., Faculty of Science, King Khalid University, Abha, Saudi Arabia essamebrahim@hotmail.com (Essam H. Ibrahim)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The preparation anti-D immunoglobulin is an important therapy for both treatment and protection. Titer of anti-D immunoglobulin preparation is an important factor to determine the dose of treatment. Many methods are used to evaluate the titer of anti-D immunoglobulin preparation. One of the new methods developed recently is column agglutination test. To evaluate the BioVue column agglutination test, it was compared to conventional tube agglutination test using anti-D immunoglobulin preparations from three different producers, ten lots each. Results showed that the BioVue column agglutination test is comparable to conventional tube agglutination test but with much ease. In conclusion, the BioVue column agglutination test is accurate and easy to use in determination of anti-D titer for quality control purposes.
Keywords
Anti-D immunoglobulin
BioVue column agglutination test
Quality control
Haemolytic disease
Anti-Rh(D) titration
Rh-factor
1 Introduction
Human Anti-Rh(D) immunoglobulin (anti-D) is a liquid or freeze-dried preparation containing immunoglobulin, mainly immunoglobulin G. The preparation is intended for intramuscular administration. It contains specific antibodies against erythrocyte D-antigen and may also contain small quantities of other blood-group antibodies. Human anti-D immunoglobulin is preferably obtained from the plasma of donors with a sufficient titer of previously acquired anti-D antibodies (Ph Eur, 2009). Although anti-Rh(D) was once the major etiology of haemolytic disease of the fetus and newborn (HDFN), the widespread adoption of antenatal and postnatal anti-D immunoglobulin has resulted in a marked decrease in the prevalence of alloimmunization due to the Rh(D) antigen present during pregnancy (Singla et al., 2010). Immune thrombocytopenia (ITP) is an acquired bleeding autoimmune disorder characterized by a markedly decreased blood platelet count. Anti-D has been successfully used in the setting of both acute and chronic immune thrombocytopenia (Cheung and Liebman, 2009). Preventing alloimmunization to the D antigen in other individuals would allow for the transfusion of D+ blood in an emergency, continued support with D+ granulocyte concentrates, and possibly prevent the concomitant formation of autoantibody (Rosse et al., 1990).
Titration is the common and simple method used in the routine laboratory to estimate the titer of an antibody (Judd, 2001).
Anti-D immunoglobulin titration can be performed in tubes, microplates or using microcolumn tests. Coombs et al. (1945) described the indirect antiglobulin test (IAT), and Diamond and Abelson (1945) described albumin, as a potentiator for the detection of “incomplete” or IgG antibodies. This classic saline IAT is still viewed as the gold standard (Rumsey and Ciesielski, 2000).
Three types of microcolumn tests have been developed: BioVue Column Agglutination Technology, affinity columns and glass microcapsules (Lapierre et al., 1990; Walker, 1997). The BioVue Column Agglutination Technology assay has been widely used in blood banking in Europe and America since 1991 for direct and indirect antiglobulin tests, ABO/Rh typing, red blood cell phenotyping, detecting unexpected antibodies, and for other applications (Lapierre et al., 1990). Its popularity grew from its standardized performance, technical ease, stable endpoint and the versatility of the methodology.
The purpose of the current study was to evaluate BioVue Column Agglutination Technology microcolumn assay for anti-D immunoglobulin titration in National Control Laboratories. The use of such method will facilitate the process of evaluating anti-D Ig titer in shorter time with more accurate results.
2 Material and methods
2.1 Samples and sample preparation
Ten Rh immune globulin (RhIG) lots each of RhoGAM UF, WinRho and Rhophylac were used. The WHO international standard anti-D immunoglobulin, 285 IU/ml (NIBSC Code: 01/572) was used as reference standard. Where 5 IU being equivalent to 1 μg (Stroncek et al., 2001), all samples and standard were initially diluted up to titer of 60 μg/ml in phosphate buffered saline (PBS) containing 2% bovine serum albumin (BSA, PBS–BSA). Serial twofold dilution of all starting preparations (60 μg/ml) was done up to 1/16,384.
2.2 Red blood cells
According to Ph Eur (2009), Rh-positive blood from five donors was pooled. These blood samples were kindly provided by blood bank, Egyptian Holding Company of Bio-Products and Vaccines. These blood samples were tested for HIV-1/2, HBsAg, HCV-Ab and syphilis antibody before supplying. Pooled blood was washed three times in PBS–BSA and then 5% RBCs suspension was prepared.
2.3 Anti-human globulin
Anti-human globulin, anti-IgG, -C3d; polyspecific (Rabbit and Murine Monoclonal) (Ortho-Clinical Diagnostics, Raritan, NJ).
2.4 Microcolumn
Ortho BioVue® system (poly cassette) was obtained from Ortho-Clinical Diagnostics. Ortho BioVue system poly cassettes (Ortho-Clinical Diagnostics, Raritan, NJ) are comprised of 6 columns containing a buffered solution with bovine albumin and macromolecular potentiators, as well as the preservatives 0.1% (w/v) sodium azide and 0.01 M ethylenediamine tetraacetic acid (EDTA).
2.5 Tube testing
Serial twofold dilutions were prepared as indicated above and titration was performed in triplicates according to American Association of Blood Banks Technical Manual (Vengelen-Tyler, 1999). Briefly, 100 μl of each serum dilution and 50 μl of red blood cell suspension were dispensed into each tube and incubated for 60 min at 37 °C. After washing three times with PBS–BSA, 100 μl of the antihuman globulin was added. All tubes were examined for agglutination. Significant titer is the last dilution giving positive reaction. Negative result was as no agglutination of the red blood.
2.6 BioVue column agglutination assay method
For the BioVue Column Agglutination Technology microcolumn assay, each 6-column cassette was seated on Ortho BioVue System Work Rack (Ortho-Clinical Diagnostics, Raritan, NJ), 50 μl BLISS (Ortho-Clinical Diagnostics, Raritan, NJ) and10 μl of RBCs suspension were added to all columns. Diluted samples in triplicates, 40 μl each, were dispensed in each corresponding column. The cassettes were incubated for 10 min in Ortho BioVue Heat Block and were spinned down for 5 min in Ortho BioVue centrifuge. Following centrifugation, the cards were examined for agglutination. Agglutinated red blood cells become trapped in or above the column glass beads and unagglutinated red blood cells move through the glass beads and form a pellet at the bottom. Significant titer is the last dilution giving positive reaction. Negative result was as no agglutination of the red blood and all of the red blood cells pass through the column glass beads and form a smooth button at the bottom of the bead column.
3 Results
3.1 Tube agglutination test
WHO international standard anti-D immunoglobulin showed positive agglutination up to dilution 1/4096 with clear negative reaction (no agglutination) at dilution 1/8192. Anti-D titration was performed on ten lots of RhoGAM UF product. The RhoGAM UF product showed positive agglutination up to dilution between 1/2048 (one lot) and 1/4096 (nine lots) with clear negative reaction (no agglutination) for all lots at dilution 1/8192. Anti-D titration was performed on ten lots of WinRho product. WinRho products showed positive agglutination up to dilution between 1/2048 (one lot) and 1/4096 (nine lots) with clear negative reaction (no agglutination) for all lots at dilution 1/8192. Anti-D titration was performed on ten lots of Rhophylac product. The product Rhophylac showed positive agglutination up to dilution between 1/1024 (one lot) and 1/2048 (nine lots) with clear negative reaction (no agglutination) for all lots at dilution 1/4096.
3.2 BioVue column agglutination assay
WHO international standard anti-D immunoglobulin showed positive agglutination up to dilution 1/8192 with clear negative reaction (all red cells at the bottom of the column) at dilution 1/16,384. The product RhoGAM UF showed positive agglutination up to dilution between 1/4096 (one lot) and 1/8192 (nine lots) with clear negative reaction for all lots at dilution 1/16,384 (Fig. 1). The product WinRho showed positive agglutination up to dilution between 1/4096 (one lot) and 1/8192 (nine lots) with clear negative reaction for all lots at dilution 1/16,384. The product Rhophylac showed positive agglutination up to dilution between 1/2048 (one lots) and 1/4096 (nine lots) with clear negative reaction for all lots at dilution 1/8192.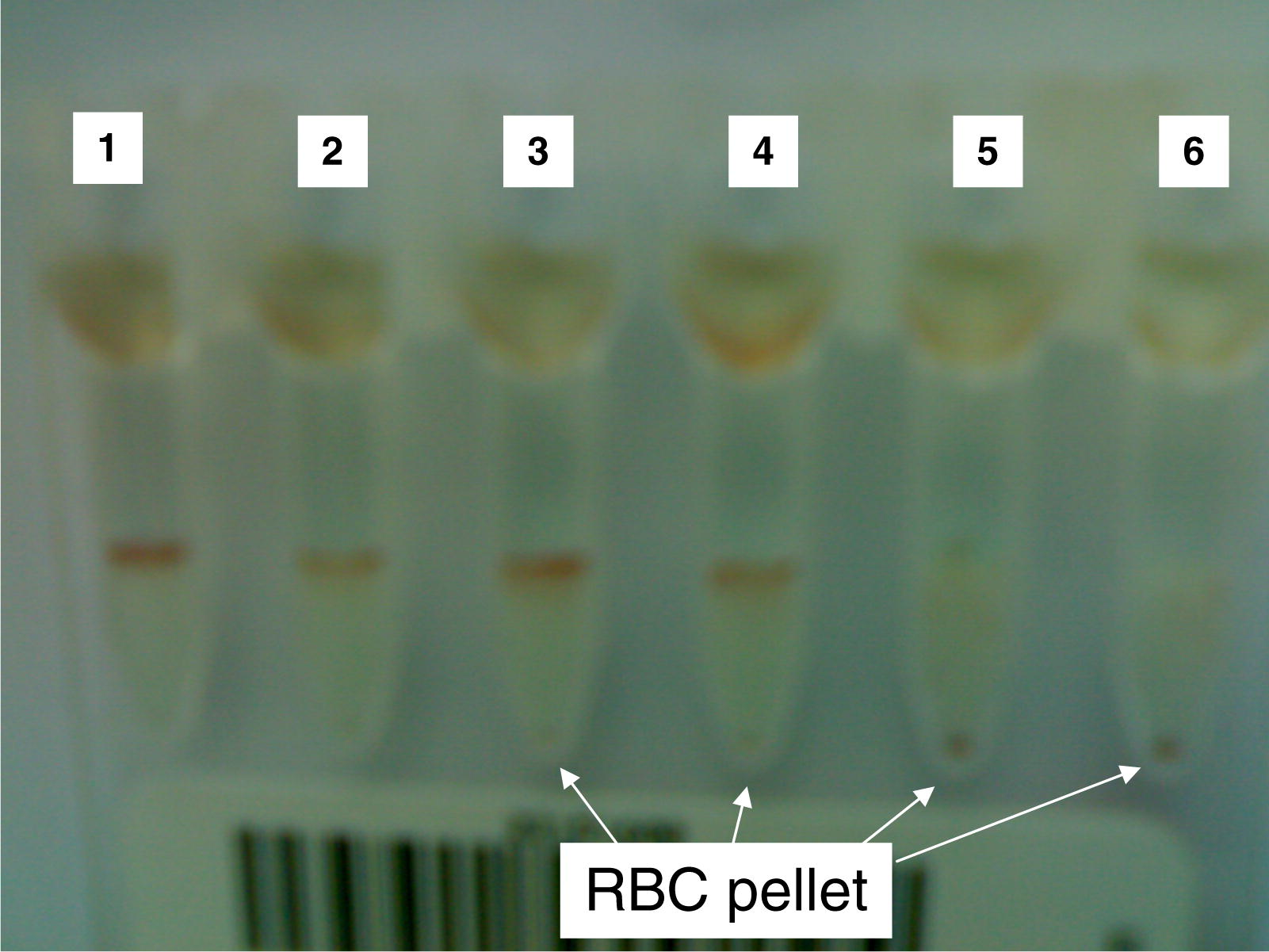
Titration of the product RhoGAM UF using ortho BioVue system poly cassettes. Microcolumns 1 and 2 showed positive agglutination (4+), microcolumns 3 and 4 showed 3+ positive agglutination, while microcolumns 5 and 6 showed negative reaction.
In all samples tested, the titers by the BioVue Column Agglutination Technology microcolumn assay were consistently higher than those by the conventional tube test. The observed differences were only twofold.
4 Discussion
The titer of human anti-D immunoglobulin preparation is determined by comparing the quantity of that preparation necessary to produce agglutination of D-positive red blood cells with the quantity of a reference preparation, calibrated in international units, required to produce the same effect. Human anti-D immunoglobulin is calibrated in international units by comparison with the international standard and intended for use in the assay of human anti-D immunoglobulin (Ph Eur, 2009).
Anti-D titration is traditionally performed by tube technique. Variation in results between laboratories is usual (Moise, 2002). In the time tube agglutination test showed twofold increase in results, but final titer of the sample regarding to the standard preparation of anti-D still the same. Studies done by Novartti et al. (2003) also demonstrated that anti-D titration in the BioVue Column Agglutination Technology microcolumn assay showed significantly higher titers (mean 3.4-fold) than the conventional tube test in all samples studied.
In tube agglutination test many steps before reading the results are involved including, incubation, wash steps, centrifugation, reconstitution and addition of reagents. Also in Ph. Eur, assay of human anti-D immunoglobulin, Method A, suitable apparatus for automatic continuous analysis, cooling coil and manifold are used as well as many reagents and reagent preparations are used. In contrary, BioVue BioVue Column Agglutination Technology used standardized method sparing the tedious washing steps which show much lower labor needed for performing the reaction and less total test time.
Method of reading of the results in tube agglutination test depends on evaluating RBCs agglutination by naked eye or by microscope which may involve human error or person-to-person differences. Techniques for reading and grading reactivity are difficult to learn, and it may be difficult for staff to maintain competence in low-volume laboratories. The unstable endpoints for the tube method can make reading, grading, and interpreting tests almost impossible (Rumsey and Ciesielski, 2000). In Ph. Eur, assay of human anti-D immunoglobulin, method A, RBCs are first lysed and haemoglobin content is estimated for every specimen. In the time it easy step to perform, it need the use of instrument and calculation. Reading of column is very easy where positive reactions are indicated by RBC agglutinates trapped anywhere in the column of the BioVue column. Negative reactions display a pellet of RBCs on the bottom of the microtube and no agglutinates within the matrix of the BioVue Column Agglutination Technology column (Rumsey and Ciesielski, 2000).
5 Conclusion
The advantages of the BioVue Column Agglutination Technology test include small sample size, decreased variation in volume delivery, greater uniformity between repeat tests, no cell washing step, and decreased technique dependence. The BioVue Column Agglutination Technology test has relatively few steps in the procedure and it provides a clear, easy-to-read, stable endpoint, so it is easy to learn. When the microtubes are covered and refrigerated, the BioVue Column Agglutination Technology cards can be read with accuracy for at least 24 h after testing. Sensitivity and specificity of BioVue Column Agglutination Technology testing have been found to be comparable to the tube agglutination test. The BioVue Column Agglutination Technology test method can replace tube agglutination method and other methods proposed in Ph Eur (2009) to evaluate the concentration of human anti-D immunoglobulin in national control laboratories as well as producer quality control laboratories.
Acknowledgements
All thanks are due LAB TOP Egypt and Ortho-Clinical Diagnostics who sponsored this work.
References
- Anti-RhD immunoglobulin in the treatment of immune thrombocytopenia. Biologics. 2009;3:57-62.
- [Google Scholar]
- A new test for the detection of weak and “incomplete” Rh agglutinins. Br. J. Exp. Pathol.. 1945;26:255.
- [Google Scholar]
- The demonstration of anti-Rh agglutinins, an accurate and rapid slide test. J. Lab. Clin. Med.. 1945;30:204-212.
- [Google Scholar]
- Practice guidelines for prenatal and perinatal immunohematology, revisited. Transfusion. 2001;41:1445-1452.
- [Google Scholar]
- The BioVue Column Agglutination Technology test: a new way to detect red cell antigen-antibody reactions. Transfusion. 1990;30:109-113.
- [Google Scholar]
- Management of rhesus alloimmunization in pregnancy. Obstet. Gynecol.. 2002;100:600-611.
- [Google Scholar]
- Comparison of conventional tube test with diamed BioVue Column Agglutination Technology microcolumn assay for anti-D titration. Clin. Lab. Haem.. 2003;25:311-315.
- [Google Scholar]
- Ph Eur, 2009. Human Anti-D Immunoglobulin, Ph Eur Monograph 0557.
- Transfusion and alloimmunization in sickle cell disease. The cooperative study of sickle cell disease. Blood. 1990;76:1431-1437.
- [Google Scholar]
- New protocols in serologic testing: a review of techniques to meet today's challenges. Immunohematology. 2000;16(4)
- [Google Scholar]
- Severe hydrops in the infant of a Rhesus D-positive mother due to anti-c antibodies diagnosed antenatally: a case report. J. Med. Case Rep.. 2010;4:57.
- [Google Scholar]
- Intravenous Rh immune globulin prevents alloimmunization in D-granulocyte recipients but obscures the detection of an alloanti-K. Immunohematology. 2001;17:37-41.
- [Google Scholar]
- Vengelen-Tyler, V., 1999. Methods. In: Technical Manual AABB, 13th ed. American Association of Blood Banks, Bethesda, MD, pp. 635–751.







