Translate this page into:
Effects of comfort care combined with blue-light phototherapy on neonatal jaundice and total bilirubin and high-sensitivity C-reactive protein levels
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
In order to explore the effects of comfort care combined with blue-light phototherapy on neonatal jaundice and total bilirubin (TBIL) and high-sensitivity C-reactive protein (hsCRP) levels, this study selected 100 neonates as research objects. Those 100 neonates were diagnosed with neonatal jaundice in a designated hospital of this study from December 2020 to December 2021, and randomly divided into observation group and control group with 50 cases in each group. The neonates in control group were given blue-light phototherapy, while the neonates in observation group were given comfort care combined with blue-light phototherapy. Before and after the treatment, the neonates in the two groups were evaluated for their quiet sleep time, the number of crying, decrease in jaundice, weight gain, and TBIL and hs-CRP levels, and compared those indicators for follow-up analysis. The results of this study show that the total effective rate was 96.0 % (48/50) in the observation group and 82.0 % (41/50) in the control group, with statistically significant difference between the two groups (P < 0.05); the indexes of the neonates’ jaundice decline [(4.41 ± 0.71) μmol/l] of the observation group were significantly better than the neonates’ jaundice decline [(3.32 ± 0.68) μmol/l] of the control group (P < 0.05); before treatment, there was no statistically significant difference in the levels of TBIL [(304.12 ± 27.63) μmol/l] and Hs-CRP [(8.01 ± 2.29) mg/L] of the observation group between the levels of TBIL [(304.08 ± 27.58) μmol/l] and Hs-CRP [(8.03 ± 2.41) mg/L] of the control group (P > 0.05); after treatment, the TBIL level [(99.27 ± 11.35) μmol/l] and hs-CRP level [(1.18 ± 0.32) μmol/l] of the observation group and the TBIL level [(123.25 ± 19.43) μmol/l] and hs-CRP level [(1.62 ± 0.45) μmol/l] of the control group were both lower than those before treatment, while the reduction degree of those in the observation group was better than that of the control group with statistically significant difference (P < 0.05). Therefore, the comfort care combined with blue-light phototherapy can achieve more ideal treatment effects than that of single use of blue-light phototherapy, which proves that the two treatment methods have certain synergy and provides a new potential technology for the prevention and treatment of neonatal jaundice.
Keywords
Neonatal Jaundice
Blue-light Phototherapy
Comfort Care
Total Bilirubin
High-sensitivity C-reactive Protein
1 Introduction
Jaundice manifested within 28 days of neonate birth is neonatal jaundice, which has a high incidence, is mainly manifested as yellowish neonatal skin, mucous membranes and sclera, and usually divided into physiological type and pathological type, with the pathology of abnormal metabolism of neonatal bilirubin and significantly increased serum bilirubin level (Montealegre et al., 2020). The blood–brain barrier in the early neonatal period is not yet mature, and bilirubin easily penetrates neonates’ brain tissues. If treatment is not timely, neonatal jaundice can lead to bilirubin encephalopathy and bring serious consequences to neonates (Nemomssa et al., 2021). The pathogenesis and causes of pathological jaundice are extremely complex, and the severity varies; if not diagnosed and treated in time, it is easy to develop into bilirubin encephalopathy, which will not only affect the normal development of neonatal nervous system, but also leave different degrees of neurological sequelae, even is life-threatening. At present, blue-light phototherapy is mainly used in clinical treatment of neonatal jaundice (Quandt et al., 2017). Continuous blue-light irritation has some treatment effects, but many neonates cannot tolerate it due to its long irradiation time. It has also been reported that continuous blue-light phototherapy can cause diarrhea, fever and other adverse reactions. Comfort care can increase the excitability of vagus nerve, increase the secretion of gastrin and insulin, thereby increase neonates’ digestive function, accelerate the excretion of meconium and conjugated bilirubin, and reduce the incidence of neonatal jaundice (Fadilla et al., 2020).
Bilirubin is metabolized from heme-containing protein and cholesterol in liver cells through complex chemical reactions, and is a metabolite of heme and is excreted with bile secretion. The neonatal body maintains a certain level of bilirubin, which can play an anti-oxidative and immunoregulatory role, but an excessive increase in its level will lead to neonate tissue and organ damage, and even develop hyperbilirubinemia (Mendes, 2017). IBIL is also called un-conjugated bilirubin, that is, bilirubin that is not bound to glucuronic acid; indirect bilirubin (IBIL) and direct bilirubin (DBIL) make up total bilirubin (TBIL). The principle of blue-light phototherapy is to irradiate the skin with light, change the structure of fat-soluble un-conjugated bilirubin, and decompose it into optical bilirubin that is non-toxic to the brain, so that it is easily soluble in water and can be quickly excreted in bile or urine and increase the excretion of bilirubin (Metz et al., 2017). High-sensitivity C-reactive protein (hs-CRP) is an acute phase protein produced by liver under stress, and it is a very important indicator of non-specific response to bacterial inflammation (Click et al., 2013). Neonatal jaundice is mostly caused by bacteria or viral infection; especially bacterial infection can produce toxins to accelerate the destruction of red blood cells, inhibit the activity of glucuronyltransferase, and affect the neonate's appetite and cause hypoglycemia, which further aggravates jaundice (Riskin et al., 2014).
In order to explore the effects of comfort care combined with blue-light phototherapy on neonatal jaundice and TBIL and hs-CRP levels, this paper conducted research by selecting 100 neonates diagnosed with neonatal jaundice in the designated hospital of this study from December 2020 to December 2021, and randomly divided them into observation group and control group with 50 cases in each group. The neonates in control group were given blue-light phototherapy, while the neonates in observation group were given comfort care combined with blue-light phototherapy. Before and after treatment, the neonates in the two groups were evaluated for their quiet sleep time, the number of crying, decrease in jaundice, weight gain, and TBIL and hs-CRP levels, and compared those indicators for follow-up analysis. The detailed chapters are arranged as follows: Section 2 introduces research materials and methods; Section 3 compares the therapeutic efficacy and TBIL and hs-CRP levels of notates in the observation and control group; Section 4 analyzes the effects of comfort care combined with blue-light phototherapy on neonatal jaundice and on TBIL and hs-CRP levels, and conducts the correlation analysis of serum hs-CRP level and TBIL level in neonatal jaundice; Section 5 discusses the mechanism of comfort care helping to improve the condition of neonatal jaundice and the clinical value of comfort care combined with blue-light phototherapy in the treatment of neonatal jaundice; Section 6 is conclusion.
2 Materials and methods
2.1 General information
In order to explore the effects of comfort care combined with blue-light phototherapy on neonatal jaundice and TBIL and hs-CRP levels, this paper conducted research by selecting 100 neonates diagnosed with neonatal jaundice in the designated hospital of this study from December 2020 to December 2021, and randomly dividing them into observation group and control group with 50 cases in each group. The control group included 27 males and 23 females; their birth times were 5–22 days with an average birth time of (10.53 ± 2.97) days; their weights were 2.15–4.33 kg with an average weight of (3.54 ± 0.37) kg; there were 3 premature infants and 47 full-term infants; their transdermal jaundice index were 11.83–17.46 mg/dl; the conditions of neonates in this group were divided into mild jaundice (13 cases), moderate jaundice (25 cases) and severe jaundice (12 cases); their etiologies were divided into infectious jaundice (13 cases), obstructive jaundice (15 cases), hemolytic jaundice (12 cases) and breast milk jaundice (10 cases). The observation group included 26 males and 24 females; their birth times were 5–23 days with an average birth time of (10.47 ± 3.14) days; their weights were 2.07–4.25 kg with an average weight of (3.44 ± 0.29) kg; there were 2 premature infants and 48 full-term infants; their transdermal jaundice index were 12.14–18.22 mg/dl; the conditions of neonates in this group were divided into mild jaundice (14 cases), moderate jaundice (26 cases) and severe jaundice (10 cases); their etiologies were divided into infectious jaundice (12 cases), obstructive jaundice (16 cases), hemolytic jaundice (11 cases) and breast milk jaundice (11 cases). The general clinical data of the two groups were similar, the difference was not significant (P > 0.05) (Table 1). This study has been approved by the hospital ethics committee, and the study's purpose, significance, and potential benefits and risks have been explained to the patients and the patients or his or her families have signed an informed consent.
Group
Gender
(male/female)
Average birth time (days)
Average weight (kg)
Jaundice index (mg/dl)
Mild
(case)
Moderate
(case)
Severe
(case)
Control
27/23
10.53 ± 2.97
3.54 ± 0.37
11.83–17.46
13
25
12
Observation
26/24
10.47 ± 3.14
3.44 ± 0.29
12.14–18.22
14
26
10
P
>0.05
>0.05
>0.05
>0.05
>0.05
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) Neonates with gestational age between 37 and 42 weeks; (2) Neonates with a birth weight of>2500 g; (3) Neonates with normal vital signs; (4) Neonates whose parents voluntarily participated in this study and were willing to sign informed consent.
Exclusion criteria: (1) Neonates with congenital diseases; (2) Neonates with abnormal liver function and bile duct obstruction; (3) Neonates with drug allergy; (4) Neonates with severe immunodeficiency; (5) Neonates whose relatives refused to participate in the study.
2.3 Treatment scheme
The neonates in the control group were given blue-light phototherapy and the treatment process was as follows: (1) Neonates' clothes and bedding were removed, the eyes were covered with black cloth, and the anus and perineum were covered with black cloth, and put into the blue-light phototherapy treatment box. (2) Continuous treatment. The wavelength of blue-light phototherapy was adjusted to 440–450 nm, the temperature in the treatment box was maintained at 28–30 °C, the irradiation time was 16 h, and the treatment was performed once a day. (3) Intermittent treatment. The irradiation wavelength and the temperature of the treatment box remained unchanged, the irradiation time was reduced to 5 h each time, the treatment was performed 3 times a day, the treatment interval was 3 h, and the course of treatment was 7 days.
The neonates in the observation group were given comfort care on the basis of the blue-light phototherapy of the control group.
2.4 Comfort care methods
-
(1)
Comfort care before phototherapy: Before phototherapy, bathe the neonates, trim their nails, wear cotton gloves and foot covers to prevent their hands and feet from scratching the skin due to crying and noisy, and put a head ring on the head to prevent the head from directly touching the flat and hard glass plate; if it causes discomfort, use black cotton goggles to protect the eyes to avoid damage to the retina, and cover the perineum and anus with diapers; the movements should be gentle and appropriate to avoid irritability.
-
(2)
Comfort care for touch and massage. Before placing the neonates in the phototherapy box, lightly stroke the neonate's head to make them feel safe. After the neonates has calmed down, perform a slight circular massage on the neonate's abdomen and back to stimulate the skin nerves and promote the excretion of meconium. The caring staffs should make eye contact with the neonates in a timely manner to enhance the neonate's sense of security and make sure that the neonates have enough sleep and try to treat during the day.
-
(3)
Comfort care for breastfeeding. It is advisable to lie on the side when feeding, so that the milk fills the front of the bottle to prevent air from entering the stomach. After feeding, assist the neonates in the right lateral position to reduce the frequency of spitting up.
-
(4)
Comfort care after phototherapy. After the phototherapy, take the neonates out of the box, remove the eye mask with gentle movements, check the eyes for infection, take a bath, and check the skin color of the whole body and whether it is damaged or not, wear clothes, and carry the neonates safely to the mother's arms.
2.5 Evaluation indicators
(1) Clinical efficacy: Neonates were tested with a skin jaundice detector; skin jaundice less than 11 and complete disappearance of skin and sclera jaundice were taken as the standard. if it reaches the standard after 1 course of treatment, it is markedly effective; if it reaches the standard after 2 courses of treatment, it is effective; if it does not reach the standard or even serious after the end of the treatment, it is invalid; total effective rate = markedly effective rate + effective rate. Markedly effective: bilirubin is<85.0 μmol/L and all clinical symptoms are disappeared; effective: bilirubin is between 85.0 and 171.0 μmol/L and all clinical symptoms are significantly improved; ineffective: bilirubin is more than 171.0 μmol/L and the clinical symptoms are not improved or even worsened. (2) Hospitalization and jaundice subsidence time. (3) Serum TBIL level of neonates: 3 mL of fasting venous blood was drawn from neonates before treatment and on the 2nd and 4th day of treatment, and the upper serum was collected after centrifugation, and the automatic biochemical analyzer was used for determination of serum TBIL level. (4) The incidence of adverse reactions in neonates during treatment, including rash, diarrhea, decreased milk production, dehydration, abnormal body temperature, etc.
2.6 Statistical methods
The obtained data were processed and analyzed by SPSS 22.0 software. The quantitative data were all expressed by the mean standard deviation ( ±s), and the t test was used for comparison between groups; the count data was expressed by the rate, and the χ2 test was used. P < 0.05 was considered statistically significant.
3 Results
3.1 Comparison of the therapeutic efficacies between the observation and control group
The data of this study shows that the jaundice decreased to (2.98 ± 0.37) μmol/L, the number of crying times was (5.11 ± 1.64) times, and the sleeping time was (13.85 ± 5.21) hours in the control group after care. The jaundice decreased to (4.19 ± 0.59) μmol/L, the number of crying times was (4.14 ± 1.14) times, and the sleeping time was (17.54 ± 4.26) hours in the observation group after care. After comparison, it was found that the indexes of jaundice decrease, crying times and sleep time in the observation group were significantly better than those in the control group (P < 0.05). The study showed that after the caring staffs adopted the comfort care program, they could significantly reduce the decrease in jaundice and the number of crying, and effectively improve the patient's sleep time. On the basis of comfort care, neonates in the observation group were treated with blue-light phototherapy and adopted a comfort care program. Caring staffs preheated the phototherapy room, adjusted the ambient temperature and humidity, wore gloves and foot covers for neonates, and adjusted the patient's body position in time according to the actual situation of neonates. Corresponding care measures should be adopted in the situation, such as checking the patient's body and skin, and carrying out cold-proof and warm-keeping work for comfort care. After care, it was found that the program can provide comprehensive care to neonates, thereby significantly improving the quality and effects of care. Table 2 shows the comparison of the therapeutic efficacies between the observation and control group.
Group
n
Quiet sleep time (h)
Crying times (n)
Jaundice drop (μmol/l)
Weight gain (g)
Control
50
13.98 ± 1.37
5.12 ± 1.63
3.32 ± 0.68
21.98 ± 1.54
Observation
50
18.55 ± 3.02
3.29 ± 1.43
4.41 ± 0.71
29.12 ± 2.44
t value
8.483
7.193
9.799
7.753
P
<0.05
<0.05
<0.05
<0.05
In this study, comfort care was given to the neonates in the control group, and comfort care was given to the neonates in the observation group. Comparing the care effects of the two groups, it was found that the sleep time of the neonates in the observation group was significantly increased compared with that in the control group, and the jaundice index was significantly higher than that in the control group. The control group decreased, the care effective rate was significantly higher than that of the observation group, and the adverse reactions were also less than those of the control group, and the difference was statistically significant (P < 0.05). It can be seen that the use of comfort care can effectively promote the therapeutic effects of blue-light phototherapy for neonatal jaundice. The environment of the phototherapy box will greatly reduce the neonate's sense of security, and the adverse reactions of the phototherapy process will bring physical and mental discomfort to the neonate (Stokowski, 2011). At this time, the neonates will vent their fear and anxiety by crying. In the face of neonates with increased physical activity, if they are not prepared, it is easy to cause skin abrasions in neonates. At the same time, neonate’s tears may cause sac infection in neonates. In addition, the change of feeding method and the special level of the stomach of the neonate can easily cause the neonate to vomit. At the same time, gentle stimulation should be delivered to the central nervous system of the neonate through the skin of the neonate by stroking, so that the neonate will have a positive physiological response and a sense of satisfaction and security, which can reduce the neonate's crying and make it actively cooperate.
Physical touch is a key factor in the care process of the treatment process, and it is the premise for allowing the neonate to receive treatment quietly. Because the neonate leaves their mother's body, there will be psychological factors such as fear and anxiety, which are expressed through crying, which is not conducive to the neonate receiving treatment (Nemomssa et al., 2021). Therefore, the caring staffs should give neonates the appropriate skin touch and comfort, so as to appease the neonate’s emotions. It is difficult to feed neonates during treatment because neonates cannot breastfeed during treatment; they can only use baby bottles instead, which causes neonates to be uncomfortable. Caring staffs should take the form of feeding a small amount multiple times. If caring staffs spit up milk, they should pay attention to keeping the inside of the box hygienic, change the position of the neonate on a regular basis, usually once an hour, change the diaper for the neonate in time, keep the skin of the neonate clean and dry, and prevent the occurrence of skin diseases. This study proves that, compared with traditional care, comfort care can effectively calm neonate’s emotions, improve neonate’s sleep quality and treatment effects, and eliminate the doubts of neonate’s family members about blue-light phototherapy treatment, which is worthy of popularization and application. Caring staffs must strictly follow the regulations during the operation, wear sunglasses to prevent eye damage, and at the same time ensure the safety of neonates and themselves.
3.2 Comparison of TBIL and hs-CRP levels between the observation and control group
In the control group, the levels of IBIL, TBIL and DBIL before treatment were (141.04 ± 22.45), (279.32 ± 40.92) and (148.63 ± 18.25) μmol/L, respectively, and the levels of IBIL, TBIL and DBIL after treatment were (79.66 ± 66 ± 40) 11.71), (151.66 ± 35.54), (81.44 ± 11.02) μmol/L; the levels of IBIL, TBIL and DBIL in the observation group before treatment were (139.93 ± 23.66), (281.43 ± 42.15), (150.20 ± 19.17) respectively μmol/L, the levels of IBIL, TBIL, and DBIL after treatment were (41.84 ± 11.53), (90.02 ± 19.34), and (47.08 ± 10.85) μmol/L, respectively. Before treatment, there was no significant difference in the levels of IBIL, TBIL and DBIL between the two groups (P > 0.05) (Table 3). After treatment, the levels of IBIL, TBIL and DBIL in the two groups were lower than those before treatment, The reduction degree of the observation group was better than that of the control group, and the difference was statistically significant (P < 0.05). In the control group, 22 cases were effective, 17 cases were improved, and 11 cases were ineffective, with a total effective rate of 78.00 %; in the observation group, 31 cases were effective, 16 cases were improved, and 3 cases were ineffective, with a total effective rate of 94.00 %. The total effective rate in the observation group was higher than that in the control group, and the difference was statistically significant (P < 0.05).
Group
n
IBIL (μmol/l)
DBIL (μmol/l)
TBIL (μmol/l)
BT
AF
BT
AT
BT
AT
Control
50
142.03 ± 13.05
42.29 ± 4.65
162.19 ± 10.44
81.63 ± 7.55
304.08 ± 27.58
123.25 ± 19.43
Observation
50
142.11 ± 12.98
30.97 ± 3.98
162.23 ± 10.39
68.84 ± 7.27
304.12 ± 27.63
99.27 ± 11.35
t value
0.019
7.947
0.033
11.38
0.043
6.092
P
>0.05
<0.05
>0.05
<0.05
>0.05
<0.05
Group
n
hs-CRP (mg/L)
BT
AF
Control
50
8.03 ± 2.41
1.62 ± 0.45
Observation
50
8.01 ± 2.29
1.18 ± 0.32
t value
0.032
4.825
P
>0.05
<0.05
An important property of bilirubin is its ability to absorb light waves, with an extremely efficient absorption rate for wavelengths between 450 and 560 nm. The peak of blue light is within this frequency band, and the use of blue light to irradiate neonates can oxidize bilirubin in neonates, and then excrete it through urine. For neonates, hyperbilirubinemia will cause certain damage to the central nervous system. Studies have shown that the serum bilirubin and the inflammatory factor hs-CRP in neonates at the onset stage were significantly increased, and the prealbumin was significantly decreased, and the range of increase or decrease was significantly increased with the severity of the disease (Namnabati et al., 2019). The hs-CRP can be used as a sensitive indicator of energy intake disorders in neonates. Some studies have found that the serum TBIL in neonates with severe jaundice and the type of jaundice is infectious jaundice is higher than that of other disease courses and types, and the serum albumin is significantly lower. Once bilirubin accumulates in the body, it will produce certain toxicity, which will have a serious impact on the normal energy metabolism of neurons. Bilirubin is very difficult to be decomposed in the nervous system, and most of it will be deposited, which will cause certain damage to the myelin sheath of the central nervous system. Abnormal expression of hs-CRP levels can be detected in neonatal jaundice caused by infection, and the changes of hs-CRP levels can reflect the degree of bacterial infection and the level of inflammatory damage in neonates.
This study found that comfort care before, during and after blue-light phototherapy can effectively improve the comfort of neonates, reduce crying, ensure the irradiation time, and improve the treatment effects and the satisfaction of the families of neonates with care services. Studies have found that touching is beneficial to the growth and development of neonates, improves the immunity and stress of neonates, promotes digestion and absorption, promotes excretion, reduces crying, and promotes sleep (Swarna et al., 2018). Alternately changing the lying position can not only expand the irradiation area, improve the treatment effects, but also prevent pressure ulcers. A comfortable environment can be seen that comfort care is to strengthen the care of neonates from multiple angles and all directions, which can detect abnormal conditions of neonates at any time, stabilize neonate’s emotions, and help neonates fully recover. The causes of neonatal jaundice are closely related to three aspects: excessive bilirubin production, low liver uptake and combined bilirubin function, and bile excretion disorder. Blue light irradiation is a safe and effective adjuvant therapy for neonatal jaundice. In this treatment process, care is particularly important. Caring staffs are required to understand the pathophysiology of neonatal jaundice and the prognosis of clinical diseases, so that the care work can be carried out smoothly, the changes in the condition can be detected in time, and the therapeutic effects of blue-light phototherapy can be ensured.
4 Correlation analysis between serum TBIL and hs-CRP levels in neonatal jaundice
4.1 Effect of comfort care combined with blue-light phototherapy on neonatal jaundice
Before treatment, there was no significant difference in serum TBIL, DBIL and IBIL levels between the two groups (P > 0.05). On the 7th day after treatment, the serum TBIL, DBIL and IBIL levels of the two groups of neonates were lower than those after treatment and the difference was statistically significant (P < 0.001). This study found that serum hs-CRP in neonates with neonatal pathological jaundice was higher than that in the control group and neonates with physiological jaundice. However, there was no significant difference in serum TBIL, DBIL and IBIL levels between the two groups on the 7th day after treatment (P > 0.05). At the same time, the incidence of diarrhea, dehydration, body temperature increase, decreased milk volume, crying and irritability in the observation group was lower than those of the control group, and the difference between the two groups was statistically significant (P < 0.05), indicating that neonates receiving intermittent blue-light phototherapy had good clinical efficacy and lower incidence of adverse reactions (Table 5 and 6). In this study, the corresponding analysis of the contents of molecules related to neurological function in serum showed that the contents of TBIL and hs-CRP were significantly lower for neonates in the combined group. The application of touch therapy to neonates exposed to blue light can not only meet the needs of neonate’s caress, but also be an effective auxiliary means to treat neonatal jaundice and promote growth and development (Ketsuwan et al., 2017).
Group
Condition
n
TBIL (μmol/l)
hs-CRP (mg/L)
Control
Mild
13
274.38 ± 26.19
3.44 ± 0.98
Moderate
25
311.27 ± 30.55
7.89 ± 2.27
Severe
12
372.49 ± 56.93
13.58 ± 5.54
Observation
Mild
14
261.49 ± 39.47
4.08 ± 1.14
Moderate
26
309.58 ± 41.09
8.48 ± 3.04
Severe
10
380.06 ± 74.38
14.05 ± 4.86
Group
Condition
n
TBIL (μmol/l)
hs-CRP (mg/L)
Control
Mild
13
98.57 ± 13.58
0.86 ± 0.13
Moderate
25
125.17 ± 20.08
1.58 ± 0.39
Severe
12
174.27 ± 36.38
2.57 ± 0.48
Observation
Mild
14
71.45 ± 10.04
0.57 ± 0.08
Moderate
26
100.33 ± 13.93
1.13 ± 0.29
Severe
10
148.36 ± 17.48
1.96 ± 0.52
The abnormal increase of the above indicators is closely related to the appearance of neonatal pathological jaundice and the severity of the disease. The reason may be that after the neonatal liver cells are damaged, the changes in their liver function lead to the level of bilirubin. Metabolism is abnormal, which in turn leads to an abnormal increase in the above indicators. In addition, in this study, TBIL and hs-CRP levels were significantly different between neonates with breast milk jaundice and neonates with hemolytic jaundice; TBIL and hs-CRP among neonates with breast milk jaundice and neonates with hemolytic jaundice, etc. The levels were significantly lower than those of neonates with obstructive jaundice; TBIL and hs-CRP levels in neonates with breast milk jaundice, hemolytic jaundice and obstructive jaundice were significantly lower than those in neonates with infectious jaundice. This suggests that the above indicators also have a certain reference value in the etiological diagnosis of neonatal pathological jaundice, and help to formulate a more reasonable treatment plan for neonates (Ekwochi et al., 2018). The results of this study also showed that the complete disappearance of jaundice in neonates with full-term neonatal jaundice in the observation group was shorter than that in the control group, indicating that the combined treatment can not only effectively reduce the bilirubin level of neonates, but also shorten the treatment time. There was no significant difference in the incidence of adverse reactions between the two groups in this study, indicating that comfort care combined with blue-light phototherapy has certain safety.
The principle of blue-light phototherapy is to irradiate the skin with light, change the structure of fat-soluble un-conjugated bilirubin, and decompose it into optical bilirubin that is non-toxic to the brain, so that it is easily soluble in water and can be quickly excreted in bile or urine and increase the excretion of bilirubin. Through the comfort care of neonatal jaundice blue light treatment, the incidence of complications during treatment is reduced, the awareness of all neonate-centered services is strengthened, the quality of care is improved, and the satisfaction of sick neonates and their families with care services is improved. Neonates who are exposed to the unfamiliar environment of the phototherapy box for the first time are prone to crying and sweating a lot. In the course of treatment, due to the sudden change of diet and the need to lie on a flat and hard glass reclining board for treatment, it will cause the neonate to feel physically uncomfortable. Therefore, caring staffs should take targeted and comfort care measures to intervene (Turnbull and Petty, 2012). Caring staffs should try to avoid the symptoms of crying and irritability in neonates during the treatment process and they should dry the sweat in time to keep the skin clean and dry to avoid getting cold. Excessive crying will cause skin abrasions and hyperventilation, sweltering syndrome, vomiting and other symptoms, so caring staffs should try to complete the care and treatment operations in the box.
4.2 Effect of comfort care combined with blue-light phototherapy on TBIL and hs-CRP levels
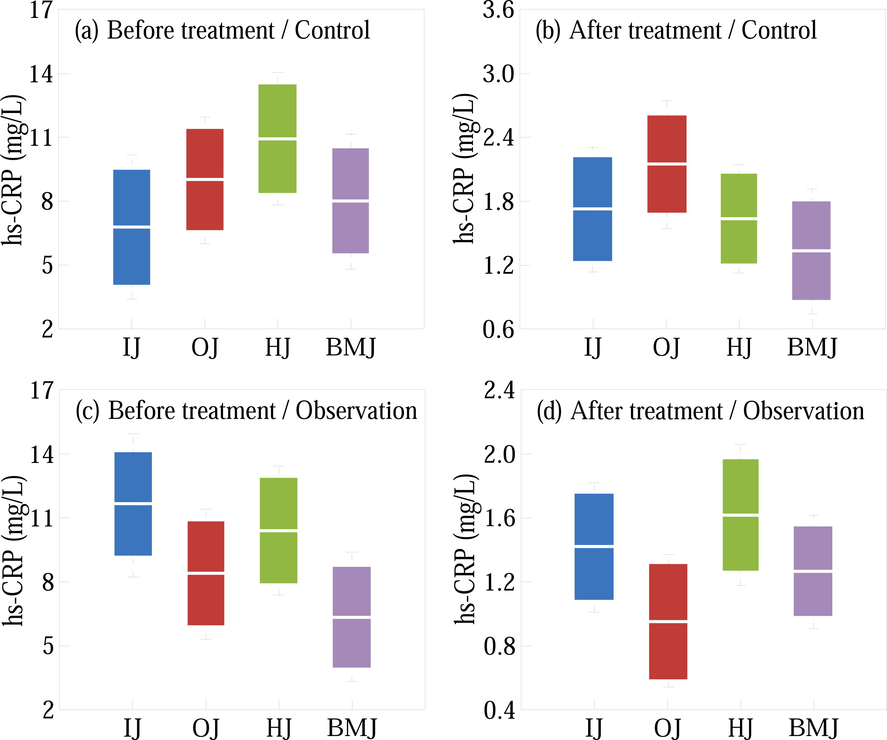
After treatment, the serum hs-CRP levels in the two groups were significantly lower than those before treatment, and the observation group was significantly lower than the control group (Table 4). Therefore, it is preliminarily believed that comfort care combined with blue-light phototherapy plays a certain role in the detection and diagnosis of neonatal jaundice. It is believed that the detection of TBIL and serum albumin can be used for the early judgment of the course and type of neonatal jaundice. Has positive clinical significance. In the control group, there were 2 cases of mild diarrhea, 2 cases of rash, and 3 cases of elevated body temperature, and the incidence of adverse reactions was 14.00 %. There was no significant difference in the incidence of adverse reactions between the two groups (P > 0.05). The results confirm that the combined therapy has a good effects and treatment effects in the treatment of neonates with hyperbilirubinemia, and it can effectively reduce the damage to nerve function. This shows that continuous blue-light phototherapy and comfort care combined with blue-light phototherapy have obvious effects on neonatal pathological jaundice, and the total therapeutic efficacy in the observation group was significantly higher than that in the control group. The correlation analysis found that hs-CRP expression was positively correlated with TBiL and DBiL in neonates with pathological jaundice, suggesting that hs-CRP can reflect neonatal severity of pathological jaundice in neonates (Garg et al., 1995). Fig. 1 shows the serum TBIL levels of the neonates with different conditions in the control and observation group before and after treatment.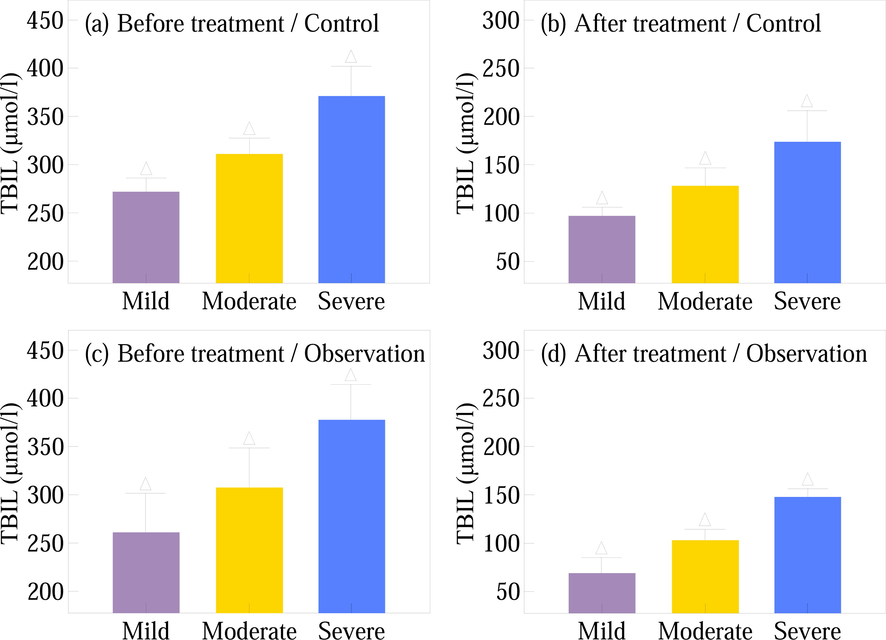
The hs-CRP levels of the neonates with different conditions in the control and observation group before and after treatment are shown in Fig. 2. In this study, the levels of TBIL and HS-hs-CRP in neonates in the physiological group and neonates in the pathological group before treatment were significantly higher than those in the neonates in the control group. The levels of TBIL and HS-hs-CRP in neonates in the physiological group before treatment were significantly lower than those in the pathological group. The levels of TBIL and HS-hs-CRP in the pathology group before treatment were significantly higher than those after treatment, which was consistent with the results of previous studies. This suggests that TBIL and HS-hs-CRP indicators have good reference value for the early diagnosis and treatment prognosis of neonates with neonatal pathological jaundice. Whether it is physiological jaundice or pathological jaundice, the best treatment plan is formulated according to the specific condition of the neonate. In addition, in this study, the level of hs-CRP was positively correlated with the levels of IBIL and TBIL, which further affirmed the value of TBIL and HS-hs-CRP in the clinical diagnosis and treatment of neonates with neonatal jaundice (Kazemian et al., 2016). As a common clinical inflammatory index, the level of hs-CRP can more effectively reflect the inflammation in the patient's body, and the detection process of this index is relatively simple, so it is widely used. When a neonate's liver is damaged and compensatory hyperplasia occurs, the hs-CRP level in the neonate will also increase rapidly in a short period of time.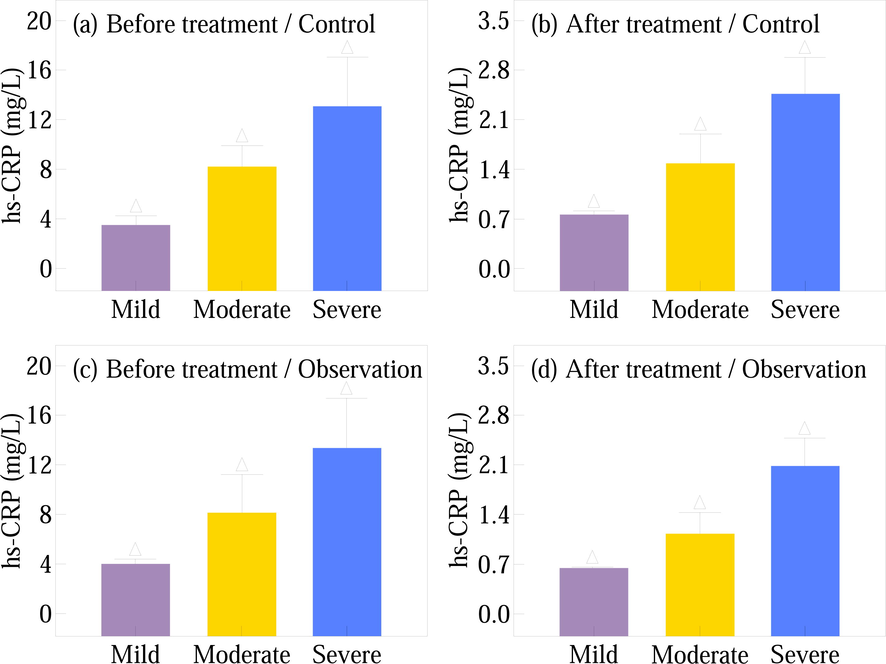
The main cause of jaundice is abnormal serum TBIL levels; blue-light phototherapy can rapidly metabolize TBIL into photorubin, which is excreted through bile and urine, reducing clinical symptoms. Continuous blue-light phototherapy has significant effects, but there are many complications. Short-term blue-light phototherapy can make the bilirubin in the body of the neonate slowly rise to the surface of the skin, and then the light is applied, which saves the light time and improves the treatment efficiency. At the same time, establishing an early warning mechanism in jaundice care work is helpful to comprehensively assess the severity of jaundice in neonates and strengthen care early (Mohamed and Elashry, 2022). During care intervention, by measuring the risk, early warning and preventive interventions are proposed to improve clinical efficacy. Regarding the cause of its pathogenesis, it is relatively general to say that the regulation mechanism of bilirubin is disordered in clinic. According to the reports, there are infectious factors, as well as congenital metabolic defects. However, the increase in bilirubin circulation causes serum bilirubin abnormally elevated hormone levels are the mainstream view. Furthermore, the abnormal metabolism of bilirubin in neonates also reflects the problems of bilirubin uptake, binding and excretion in neonates, so the phenomenon of jaundice occurs, which also provides ideas for clinical treatment.
5 Discussions
5.1 Mechanisms for comfort care helping improve neonatal jaundice
Touching in comfort care can increase the excitability of the vagus nerve, thereby increasing the secretion of gastrin and insulin, increasing the amount of breastfeeding of the neonates, enhancing the digestive function, promoting the digestion and absorption of food, shortening the retention time of feces, thereby accelerating the meconium and the combined gallbladder. The excretion of rubin reduces the reabsorption of bilirubin in the small intestine, reduces serum bilirubin levels, reduces the risk of kernicterus and reduces the incidence of neonatal pathological jaundice. Neonatal meconium in the observation group was earlier than that in the control group, and jaundice appeared later than that in the control group. The duration of jaundice and the degree of jaundice of neonates in the observation group were shorter than those in the control group. This shows that comfort care can significantly shorten the first yellowing of neonatal meconium and help reduce the jaundice index at the peak of neonatal physiological jaundice, that is, reduce serum bilirubin levels and reduce the occurrence of neonatal pathological jaundice rate and the risk of kernicterus (Fig. 3). Comfort care combined with blue-light phototherapy can promote the early completion of meconium in neonates, and significantly reduce neonatal jaundice index and neonatal hyperbilirubinemia, which is an effective new auxiliary technology for the prevention and treatment of neonatal jaundice and is worthwhile for clinical application (Gams, 2012).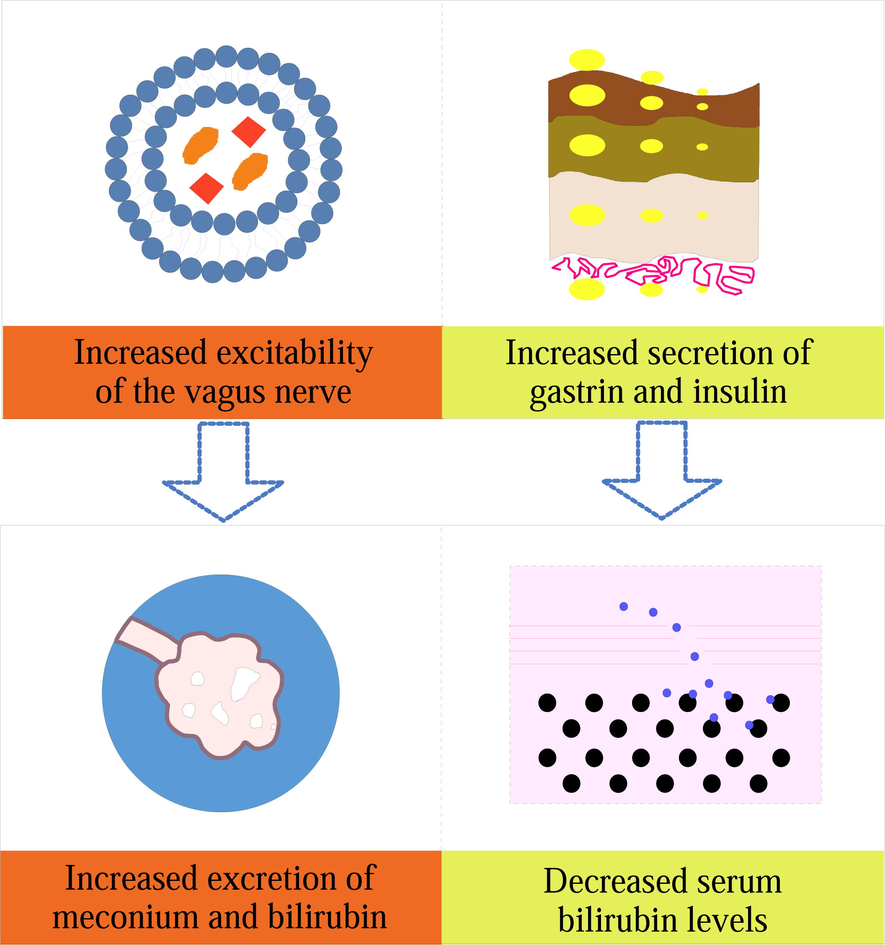
Comfort care focuses on the care of neonates before, during and after treatment, whose advantages include: (1) Eliminate the anxiety of family members, reduce the psychological pressure of family members, increase the treatment confidence of the patient's family members, and establish the relationship between the family members of neonates and the family members, and a sense of trust between caring staffs so that the treatment process can go smoothly; (2) Protect the sensitive parts of the neonate before treatment, and avoid light to make crying and noise affect the progress of the treatment process; other parts can be exposed to ensure that all parts of the neonate except the sensitive parts receive cold light source blue light; (3) Observe and record the physical response characteristics of the neonate at any time during the treatment for comparison and analysis after the treatment; breastfeeding should be performed every 2 h, and the head of the neonate should be turned to one side during feeding; avoid inhaling vomitus, but also ensure the neonate's body's demand for water at any time, so as to avoid the neonate's restlessness due to insufficient water, which affects the continuation of the treatment process; (4) After the treatment, check the neonate's body to see if there is any damage on the neonate's body, and do a good job of cleaning and care the skin of the neonate to prevent the skin from being infected by bacteria and affecting the subsidence of jaundice and the disinfection of the treatment box for the next use.
Comfort care is a holistic, individualized, creative and effective care mode, which enables neonates to achieve the most pleasant state, or shorten or reduce their unpleasantness in physical, psychological, social and spiritual. Blue light irradiation is a simple, easy, safe and effective method to treat neonatal jaundice and reduce serum bilirubin. However, during the treatment process, due to the separation of mother and baby, changes in feeding methods, and sleeping naked on the hard board of the phototherapy box, black cotton cloth covers the eyes (Carceller-Blanchard et al., 2009). Such changes in comfort level will cause physical and mental discomfort in neonates and affect the therapeutic effects of blue-light phototherapy. Therefore, comfort care combined with blue-light phototherapy provides a better method for the treatment of neonatal jaundice. Touching can increase the excitability of the vagus nerve, thereby increasing the secretion of gastrin and insulin, increasing the milk intake of the neonates, promoting the digestion and absorption of food, shortening the excretion time of meconium, thereby accelerating the excretion of meconium and conjugated bilirubin, reduce the incidence of bilirubin encephalopathy and reduce the incidence of neonatal pathological jaundice. In addition, touching can enhance the immunity and stress of infants, which is conducive to the growth and development of neonates, and can promote digestive function, reduce crying, stabilize emotions, and improve sleep. Therefore, the application of touch therapy to neonates exposed to blue light can not only meet the needs of neonate’s caress, but also be an effective auxiliary means to treat neonatal jaundice and promote growth and development.
5.2 Clinical value of comfort care combined with blue-light phototherapy in the treatment of neonatal jaundice
The most fundamental needs of human beings are comfort. Usually, neonates can satisfy their own comfort needs under normal conditions. Neonates with neonatal jaundice experience discomfort both psychologically and physically when they receive blue-light phototherapy. After leaving the mother's body, the neonate often has feelings of insecurity, fear, etc., and often expresses his uncomfortable feeling by crying. Treatment in the board can cause physical discomfort to the neonate and caring staffs should take targeted and comfort care measures to intervene. Caring staffs should try to avoid the symptoms of crying and irritability in neonates during the treatment process. Excessive crying will cause skin abrasions, sweltering syndrome, vomiting and other symptoms, so care and treatment operations should be completed in the box as much as possible (El-Kurdy et al., 2021). The results of this study showed that the number of crying in the observation group was significantly less than that in the control group, and the neonate’s jaundice reduction index, weight gain, and quiet sleep time were significantly different from those in the control group (Fig. 4). Therefore, the use of comfort care intervention during the blue-light phototherapy treatment of neonatal jaundice neonates can effectively improve the comfort level of neonates and improve the treatment effects of neonates, which has great clinical significance.Fig. 5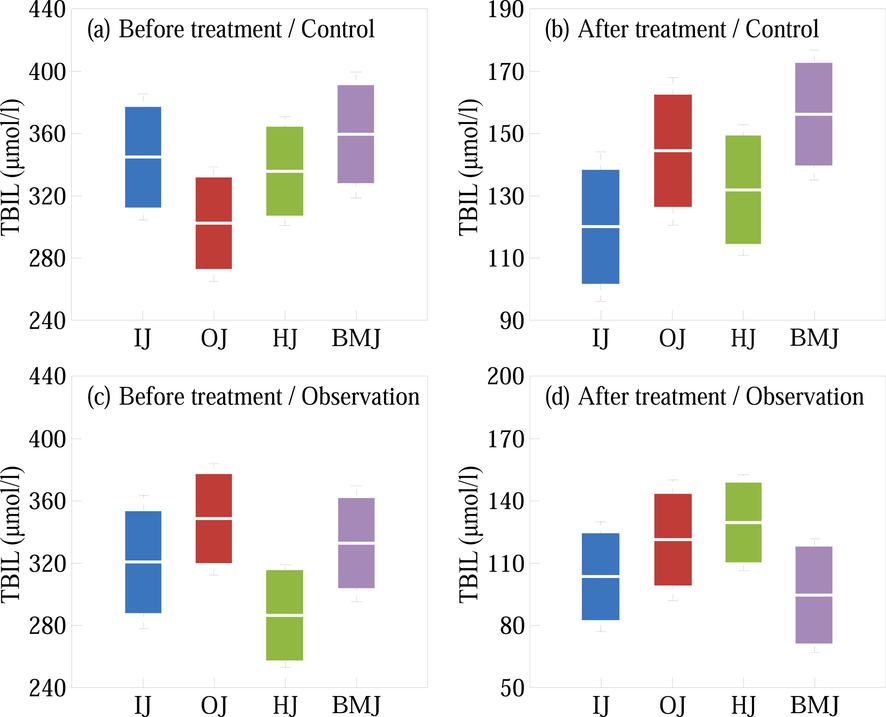
When the neonate's stomach is full and still crying, a comfort pacifier can be given, because the comfort pacifier can reduce the neonate's response to pain and also reduce the neonate's response to discomfort. From the results of this study, it can be seen that targeted comfort care was provided to neonates in the observation group during the blue-light phototherapy treatment, such as maintaining a comfortable position, adding touch therapy, increasing the frequency of feeding, and giving comfort pacifiers. The quiet sleep time was significantly longer than that of the control group who received routine care (P < 0.05), the weight and weight of neonates increased significantly within 3 days (P < 0.05), and the jaundice index by skin test was significantly decreased after 3 days (P < 0.05), indicating comfort care. It can reduce the psychological stress of neonates, make them quiet and comfortable, and improve sleep; comfort care can stimulate the functions of the digestive system and nervous system, increase the effects of blue-light phototherapy, significantly reduce the jaundice index, and increase body weight rapidly. At the same time, the comfort care model reflects the connotation of holistic care and the comprehensive quality of caring staffs, truly embodies neonates-centered humanized service concept, and conforms to the transformation of the medical model.
Specific parts of the human body surface have a close correspondence and connection with various internal organs of the human body. Through comfort care, intestinal peristalsis can be promoted and normal metabolism of neonates can be ensured. For example, in the study of this group, the care effects of neonates in the observation group was significantly better than that in the control group, and the difference was significant, and the yellowing time of neonates in the observation group was significantly shortened, thus effectively reducing the incidence of pathological jaundice in neonates. In this paper, comfort care is applied throughout the whole process of blue-light phototherapy treatment (Lam et al., 2008). The observation group effectively improved the neonate’s sleep and feeding status, increased the frequency of defecation, and promoted the excretion of bilirubin, which is conducive to the subsidence of jaundice. In every detail of the care work, it reflects the beauty of care skills, pays attention to improving the comfort of the neonate and the mother, and has won the trust and praise of the parents. At the same time, the neonates-centered care model promotes the self-worth of caring staffs, increases the autonomy of caring staffs and the sense of responsibility for care neonates, so that caring staffs have a love to actively provide care for neonates. The implementation of the comfort care model has effectively promoted the development of high-quality care services, which is worthy of clinical application and in-depth research.
6 Conclusions
This paper selected 100 neonates diagnosed with neonatal jaundice to explore effects of comfort care combined with blue-light phototherapy on neonatal jaundice and TBIL and hs-CRP levels. The neonates in control group were given blue-light phototherapy, while the neonates in observation group were given comfort care combined with blue-light phototherapy. The results of this study show that the total effective rate was 96.0 % (48/50) in the observation group and 82.0 % (41/50) in the control group, with statistically significant difference between the two groups (P < 0.05); the indexes of the neonates’ jaundice decline, crying times and sleep times in the observation group were significantly better than those of the neonates in the control group (P < 0.05); before treatment, there was both no significant difference in TBIL and hs-CRP levels between the neonates of the two groups (P > 0.05); after treatment, the TBIL and hs-CRP levels in the two groups were both lower than those before treatment, while the reduction degree of those in the observation group was better than that of the control group with statistically significant difference (P < 0.05). Therefore, the comfort care combined with blue-light phototherapy can achieve more ideal treatment effects than that of single use of blue-light phototherapy, which proves that the two treatment methods have certain synergy and provides a new potential technology for the prevention and treatment of neonatal jaundice. Touching can increase the excitability of the vagus nerve, thereby increasing the secretion of gastrin and insulin, increasing the milk intake of the neonates, promoting the digestion and absorption of food, shortening the excretion time of meconium, thereby accelerating the excretion of meconium and conjugated bilirubin, reduce the incidence of bilirubin encephalopathy and reduce the incidence of neonatal pathological jaundice. Therefore, the application of touch therapy to neonates exposed to blue light can not only meet the needs of neonate’s caress, but also be an effective auxiliary means to treat neonatal jaundice and promote growth and development. The results of this research provide a reference for further research on the effects of comfort care combined with blue-light phototherapy on neonatal jaundice and TBIL and hs-CRP levels.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Point of care testing: transcutaneous bilirubinometry in neonates. Clin. Biochem.. 2009;42(3):143-149.
- [CrossRef] [Google Scholar]
- An osteopathic approach to reduction of readmissions for neonatal jaundice. Osteopath. Fam. Physician.. 2013;5(1):17-23.
- [CrossRef] [Google Scholar]
- Determinants of delay in presentation and clinico-laboratory features of newborns admitted for neonatal jaundice in a tertiary hospital in south-east Nigeria. J. Trop. Med.. 2018;20(2):128.
- [CrossRef] [Google Scholar]
- Effect of antenatal sessions on postnatal knowledge and practices regarding neonatal jaundice among high-risk primigravidas. Egypt. J. Health Care.. 2021;12(3):1077-1092.
- [Google Scholar]
- A multifunction infant incubator monitoring system with phototherapy and ESP-32 based mechanical swing. Int. J. Sci. Technol. Manag.. 2020;1(4):371-381.
- [Google Scholar]
- Operationalizing palliative care processes through a perinatal palliative care program. J. Obstet. Gynecol. Neonatal Nurs.. 2012;41:S44-S45.
- [CrossRef] [Google Scholar]
- A controlled trial of high-intensity double-surface phototherapy on a fluid bed versus conventional phototherapy in neonatal jaundice. Pediatrics. 1995;95(6):914-916.
- [CrossRef] [Google Scholar]
- Evaluation of the Beneficial Effects of rooming-in care, in icteric hospitalized neonates. Iran. J. Neonatol.. 2016;7(4):7-10.
- [CrossRef] [Google Scholar]
- The association of breastfeeding practices with neonatal jaundice. J Med Assoc Thai. 2017;100(3):255-261.
- [Google Scholar]
- Evaluation of a point-of-care transcutaneous bilirubinometer in Chinese neonates at an accident and emergency department. Hong Kong Med. J.. 2008;14(5):356-360.
- [Google Scholar]
- Equipment needs for premature babies in special care or intensive care. Br. J. Hosp. Med.. 2017;78(12):695-698.
- [CrossRef] [Google Scholar]
- Continuous coloured light altered human brain haemodynamics and oxygenation assessed by systemic physiology augmented functional near-infrared spectroscopy. Sci. Rep.. 2017;7(1):1-11.
- [CrossRef] [Google Scholar]
- Effect of swaddle bathing versus traditional bathing on physiological stability and comfort level among neonates. Assiut Sci. Nurs. J.. 2022;10(28):68-79.
- [CrossRef] [Google Scholar]
- Effectiveness and safety of two phototherapy devices for the humanised management of neonatal jaundice. An. Pediatr.. 2020;92(2):79-87.
- [CrossRef] [Google Scholar]
- The effect of home-based phototherapy on parental stress in mothers of infants with neonatal jaundice. J. Neonatal Nursing. 2019;25(1):37-40.
- [Google Scholar]
- Optimization of phototherapy machine for advanced treatment of neonatal jaundice. Abyssinia J. Eng. Comput.. 2021;1(1):22-25.
- [CrossRef] [Google Scholar]
- POF-yarn weaves: controlling the light out-coupling of wearable phototherapy devices. Biomed. Opt. Express.. 2017;8(10):4316-4330.
- [CrossRef] [Google Scholar]
- Influence of changes in the evaluation of neonatal jaundice. Am. J. Perinatol.. 2014;31(03):203-208.
- [CrossRef] [Google Scholar]
- Fundamentals of phototherapy for neonatal jaundice. Adv. Neonatal. Care.. 2011;11:S10-S21.
- [CrossRef] [Google Scholar]
- The smart phone study: assessing the reliability and accuracy of neonatal jaundice measurement using smart phone application. Int. J. Contemp. Pediatr. 2018;5(2):285-289.
- [CrossRef] [Google Scholar]
- Early onset jaundice in the newborn: understanding the ongoing care of mother and baby. Br. J. Midwifery. 2012;20(9):615-622.
- [CrossRef] [Google Scholar]







