Translate this page into:
Effect of energy window width on planer and SPECT image uniformity
*Corresponding author
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Abstract
To detect radiopharmaceutical distribution in patient organs and avoid interpretation mistakes, due to the protocol errors, a gamma camera must work in optimum conditions. One such error is camera non-uniformity. Baron and Chouraqui[Baron, J.M., Chouraqui, P., 1996. Myocardial single-photon emission computed tomographic quality assurance. J. Nucl. Cordial. 3(2), 157–166] have reported the need to ensure consistently high image quality and accuracy using an optimally chosen standardized protocol. It has been reported that single photon emission computed tomography (SPECT) significantly improved contrast over the planer image and has the ability to separate overlapping structures[Critchly, M., 1993. Nuclear Medicine Pocket Handbook, Amersham International Plc, pp. 6–7]. Window width of energy is considered as one of the most important physical parameters affecting the quality of planer and SPECT images. Thus, the effect of widow widths of energy 5%, 10%, 15%, 20% and 25% on planer and SPECT images were investigated using a Tc-99m source at 140 keV. Tc-99m is the most common isotope in nuclear medicine and has one well-defined peakT in comparison with thallium, which has three peaks. In the present study, it was evident that energy window width played a prominent role in flood images uniformity using the Tc-99m source. The calculated integral uniformity percentage (IU%) and differential uniformity percentage (DU%) values of center field of view (CFOV) and useful field of view (UFOV) were markedly changed with a change of energy window width. The optimum energy window width was in the range from 15% to 20%. Moreover, the effect of window widths of energy 5%, 10%, 15%, 20% and 25% on SPECT image on a heart phantom with an artificial defect performed at the anterior wall of the heart was investigated. The SPECT images were clinically examined by a physician who reported a different diagnosis for each energy window width due to vertical long axis cuts, which, in turn, were due to the change in the collected counts. We concluded that the optimum energy window width was also in the range 15–20% for the Tc-99m isotope, which confirmed previous planer results.
Keywords
Diagnostic imaging
Radiopharmaceutical
SPECT
Physical parameter
Gamma camera
1 Introduction
In nuclear medicine imaging techniques, to obtain information on physiological function and radiopharmaceutical distribution in an organ of interest, the patient is injected with a suitable radioactive isotope emitting gamma rays that can be detected by a gamma camera. The scintillation gamma camera is combined with a computer for analyzing and displaying the recorded images (Critchly, 1993). Gamma cameras are used in SPECT imaging where several static images from different angles are recorded SPECT imaging is preferable than planer imaging because it displays the images in three directions, where the camera detects the distribution of the injected radiopharmaceutical from varying angles around the patient’s body at fixed intervals (Iskandrian and Heo, 1987). For SPECT systems, the important acquisition is the area between spatial resolution and sensitivity. Camera systems with two or more heads surrounding the patient with more detectors have offered greater optimal spatial resolution and sensitivity characteristics than those available with a single-head system. Guidelines for quality control (QC) testing and the choice of tests to be performed at certain intervals are given PP in the literature (Graham, 1995). Performance measurements of scintillation cameras and other tests include pixel size calibration, linearity measurements, rotational sensitivity, mechanical alignment, energy distribution and counting rate capabilities (Groch and Erwin, 2000, 2001). The common sources of artifacts were non-uniformity in gamma-camera detectors, center of rotation errors, misaligned cameras on multi-detector scanner systems, errors in image reconstruction, patient motion and radiotracer uptake in non-target organs and attenuation. The best way to avoid these artifacts is to pay very close attention to the technical factors of image acquisition, as well as processing away from attenuation factors (Cerqueira and Matsuoka, 1988). Completed clinical studies must be checked for unacceptable patient movement and incomplete views (DePuey, 1994). Baron and Chouraqui (1996) have reported the need for ensuring consistently high image quality and accuracy using on optimally standardized protocol. The effects of center-of-rotation (COR) shift on contrast and spatial resolution of SPECT systems (Saw, 1986) and shift of rotating camera-based SPECT system on the tomography of images (IAEA, 1991) have been reported. SPECT, using a rotating gamma camera, also needs accurate calibration of the electromechanical components, the detection system and reconstruction software (Agostini et al., 1987). Advances in gamma-camera design over the last 10 years have improved all aspects of image quality, particularly for tomographic imaging (Groch and Erwin, 2000, 2001). Advances in gamma-camera design have improved all aspects of image quality, particularly for tomographic imaging (Groch and Erwin, 2000, 2001). Liu et al. (1999) evaluated the integral uniformity (IU), differential uniformity (DU) and corrected relative standard deviation (CRSD). The most sensitive indicator of gamma-camera performance is uniformity, because it is performed on a daily basis as well as being the principle tool in evaluating the status of the camera. Most artifacts related to integrity of the detector head, computer system and hard-copy device can be detected on the uniformity image. The determination of the action level of gamma-camera non-uniformity is difficult as the reproducibilities of quality control measurements, as well as the service adjustments, are usually unknown. Liu et al. (1999) have evaluated the reproducibility of integral uniformity (IU), differential uniformity (DU) and corrected relative standard deviation (CRSD). Nuclear medicine imaging has not reached the level of standardization and automation, due to the large number of physical parameters affecting image uniformity, since each individual parameter must be chosen or been aware of before commencing imaging. Moreover, there is a limited number of reports in this particular field of study as controversy still surrounds the relevance of energy window width on planer and SPECT image uniformity. Thus, as a step toward obtaining a through understanding of the relevance of energy window width on all aspects of image quality, particularly tomographic imaging is required. In this study, we examined the effect of energy window width using a gamma camera on planer and SPECT images uniformity.
2 Materials and methods
2.1 Gamma camera
The gamma camera used in the present study is a dual-head, variable angle system, model E camera, manufactured by Siemens (USA), and installed in the National Cancer Institute (Cairo, Egypt). It consists of a gantry with detectors (including remote hand control units and a display panel mounted on top of the gantry), detectors, collimators, collimator servers, p.
2.2 Tc-99m generator
It produces a sterile solution of Tc-99m as sodium pertechnetate. This solution is eluted using 0.9% sterile and endotoxin-free solution of sodium chloride from an alumina chromatography column. The Mo-99 (TB1=2B = 66.02 h) parent of Tc-99m (TB1=2B = 6.02 h) is adsorbed. The eluant, which consists of nearly pure sodium pertechnetate, is then ready for combining with an agent to form the radiopharmaceutical.
2.3 Dose calibrator
It consists of an ionization chamber (model VIk-304) and AVDC-304 control unit. It has a fixed setting for the well-known isotopes, Tc-99m, Tl-201, I-131, etc. Both the ionization chamber and control unit are microprocessors, which communicate with each other using a communication link. The control unit commands the chamber to perform the actions. Calibration factors for most isotopes can be set on the control unit and are sent to the ionization chamber. The calibration factor for each isotope is used through the microprocessor of the dose calibrator to calculate proper activity.
2.4 Preparation of a point
Ball of cotton with Tc-99m activity in the rage of 74–111 kBq is placed in a small plastic cone to obtain a small concentrated source, to avoid scattering and enable concentrating the radioactivity in a small and uniform size. A small piece of cotton (approximately 3 mm in diameter) is placed into the vial. Then, drops of Tc-99m are placed on the cotton.
2.5 Performing intrinsic flood uniformity calibration
The system updates the intrinsic correction data applied to patient studies only if at least 50 million counts are collected. For SPECT images with 64 × 64 or 128 × 128 matrices, floods of 50 million counts are sufficient to correct images. The patient position monitor (PPM) is used to verify that the count rate is approximately the same at each detector. The pallet position is adjusted until the count rate between the detectors falls within the range of 5%. Non-uniformity is measured from the counts stored in the individual pixel values, is recoded by the computer and calculated as follows:
2.6 The integral uniformity (IU) %
The difference between the higher and the lower pixel value: where Max is the maximum pixel count and Min is the minimum pixel count.
2.7 The differential uniformity (DU) %
The difference between two adjacent pixels: where hi is the max % pixel counts, and low is the min % pixel counts, for all rows and columns within a localized line of pixels; (hi–low) is the largest deviation.
2.8 Effect of energy window width % on uniformity
This study was designed to investigate the relationship between IU% and DU% of CFOV and UFOV and window widths of energy 5%, 10%, 15%, 20% and 25%. Off-peak shift of energy was at 0% during the experiment with the window centered at the middle of the peak. The analyzer is opened to adjust off peak and the energy window width at 5%.
2.9 Acquisition parameters
2.9.1 Camera information
Matrix size 256 × 256, magnification 1.0, off peak 0% and count rate 50 kcuts/s.
2.9.2 Scan information
The collected counts are 50,000,000 counts.
2.10 Effect of energy window width % on SPECT image using a heart phantom
The outer cavity of a heart phantom was filled with approximately 56 kBq Tc-99m. The heart phantom was fixed inside a lung phantom and was filled with water. The cover plate was placed on the phantom, was tighten, and pressure was gently applied by hand to the plate and was carefully screwed in the cover plate screws. The phantom was filled through the filler holes from the top cover plate using syringe; water was injected into the phantom until the solution level nears the cover plate. All the filler plugs were screwed and left one. The phantom was tilted so that the remaining air bubbles were moved toward the open filler hole, water was steadily injected into the open hole until the phantom was completely filled and lastly was screwed in the final filler plug.
This study was done using a heart phantom in multi-SPECT acquisitions, at five different window widths of energy 5%, 10%, 15%, 20% and 25% with the same parameters in each acquisition. The heart lung phantom was prepared as before, the phantom was placed on the patient bed as a patient, all the acquisition parameters were fixed, and then the acquisition of SPECT was started. The energy window widths as 5%, 10%, 15% 20% and 25% were used, and then the previous steps were repeated.
2.10.1 Camera information
The used parameters were matrix size 64 × 64, magnification 1.45, window widths of energy 5%, 10%, 15% 20% and 25% and count rate 50 kcuts/s. We have used matrix sizes of 64 × 64 or 128 × 128, which in SPECT studies is in accordance to the international recommendation for saving computer memory, decreasing the time of collecting counts and obtaining the best quality images. Moreover, the time of investigation the patient was limited and very short, ∼15 min; throughout this period the patient should be fixed without any motion to eliminate image artifacts.
2.10.2 Scan information
The used parameters were rotation-type step and shoot, orbit-type body contour, number of views per scan: 32 and detectors configuration: 90o.
3 Results
Fig. 1 represents the relationship between the energy of Tc-99m (keV) and the relative number of counts.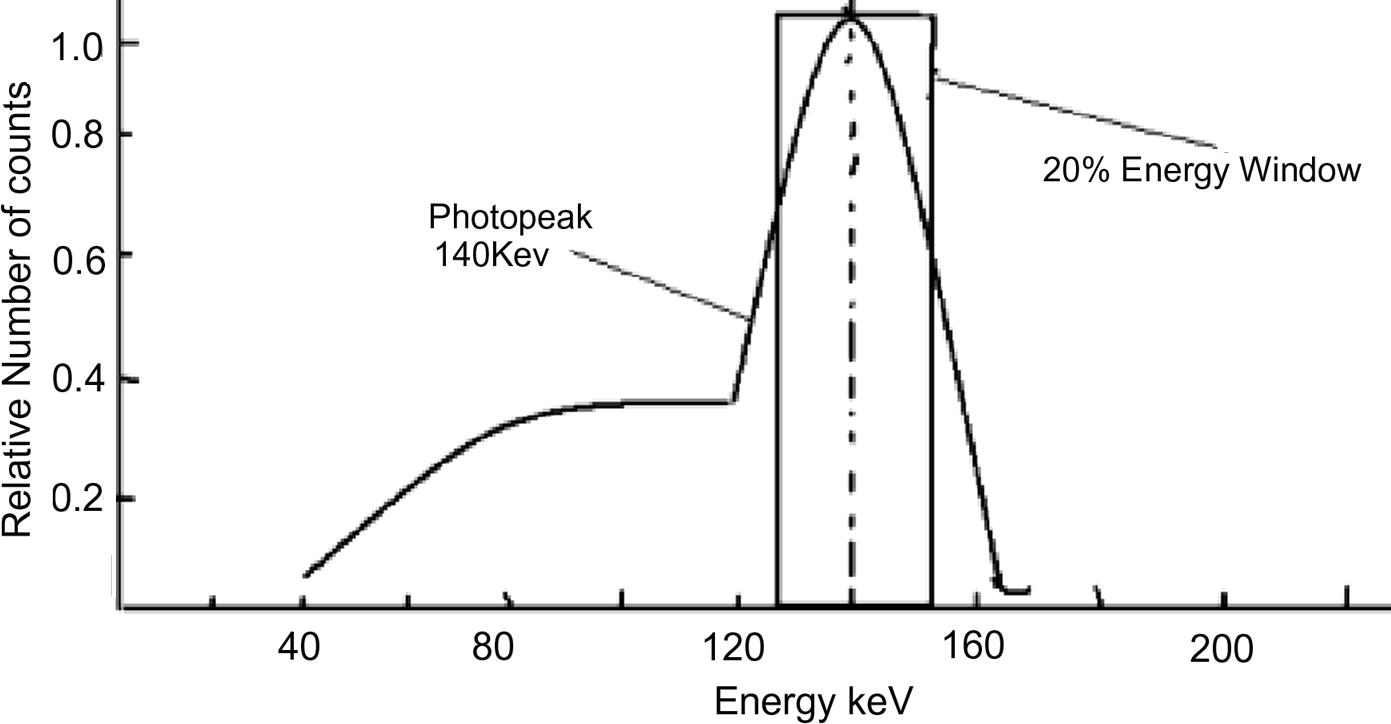
Relationship of energy of Tc-99m (keV) versus the relative number of counts.
3.1 Effect of energy window width % on images uniformity
The calculated IU% and DU% values of CFOV and UFOV for different window widths of energy at off-peak shift of energy 0% are shown in Table 1.
Window width % (keV)
Intergal uniformity (CFOV)
Differentia uniformity (CFOV)
Intergal uniformity (UFOV)
Differentia uniformity (UFOV)
5
2.7
1.95
3.23
2.11
10
2.28
1.81
2.93
2.13
15
2.3
1.6
2.5
1.9
20
2.18
1.82
2.37
1.82
25
2.23
2.05
2.67
2.22
Fig. 2 represents energy window widths at 5%, 10%, 15%, 20% and 25% versus calculated IU% and DU% values of CFOV and UFOV. Fig. 2 shows a decrease in IU% and DU% uniformities of CFOV and UFOV in the range of 5–15%, which indicates a marked change in image uniformity. In the window width range of energy of 15–20%, there was no clear change in the calculated values of IU% and DU% in CFOV and UFOV, which indicated optimum energy uniformity. It is evident that an increase in energy window width % indicated loss in the image uniformity.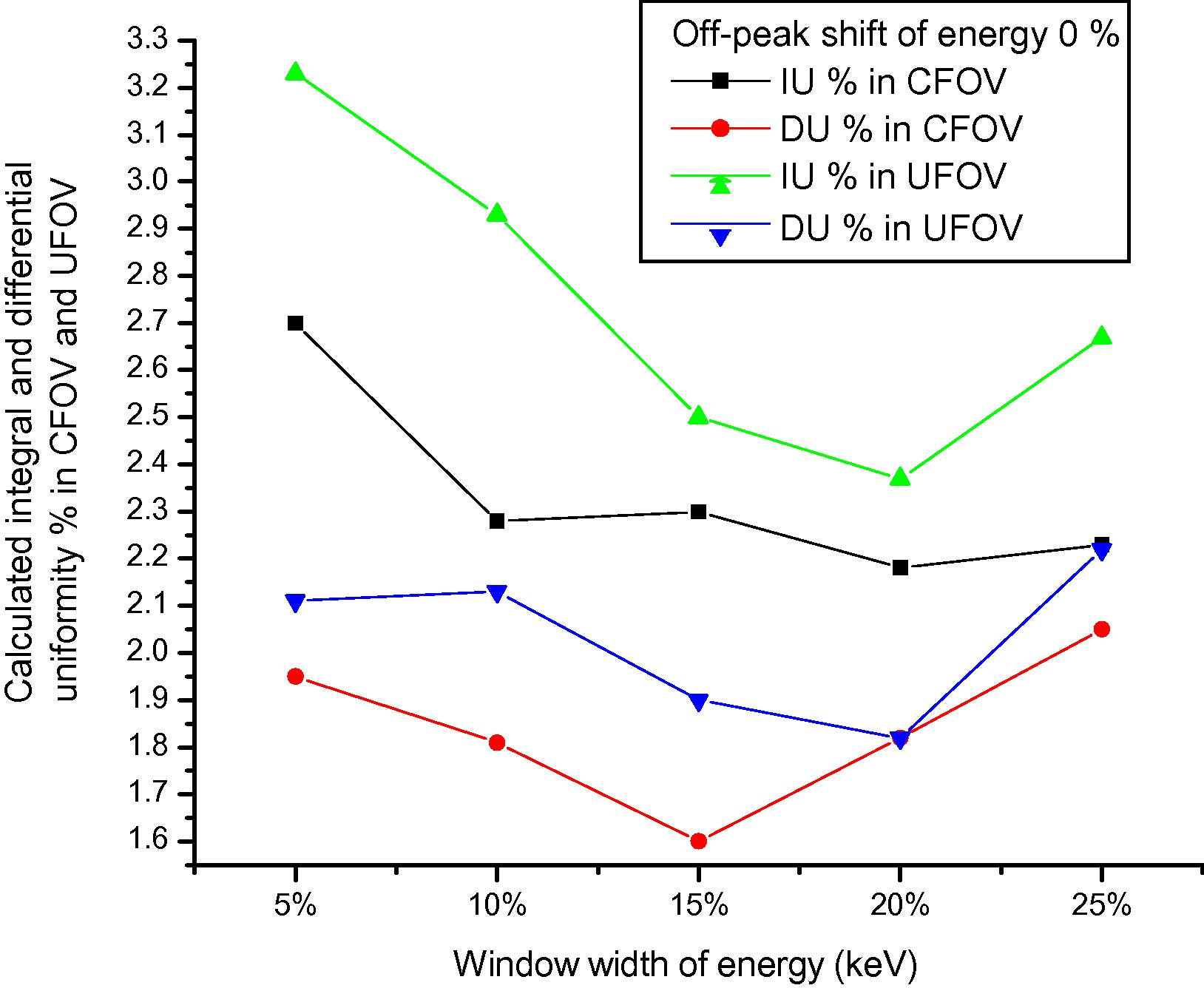
3.2 Effect of energy window width on SPECT image uniformity using a heart phantom
Fig. 3 shows five rows of vertical long axis cuts of a heart phantom SPECT at window widths of energy 5%, 10%, 15%, 20% and 25%, and 0% off-peak shift of energy. The change, from a medical point of view, is due to the vertical long axis cuts, which in turn are due to the change in the collected counts, i.e., change in the diagnosis. From the medical point of view, at energy window width 5%, perfusion at the defect center in the interior wall (sharp defect) is almost absent i.e., impressive myocardial infarction. At window widths of energy 10%, there are moderate to marked hypoperfusion of defect, i.e., likely reversible ischemia. At window width of 25%, the defect indicated hypoperfusion, while the rest of the anterior and inferior wall appears mildly hypoperfused.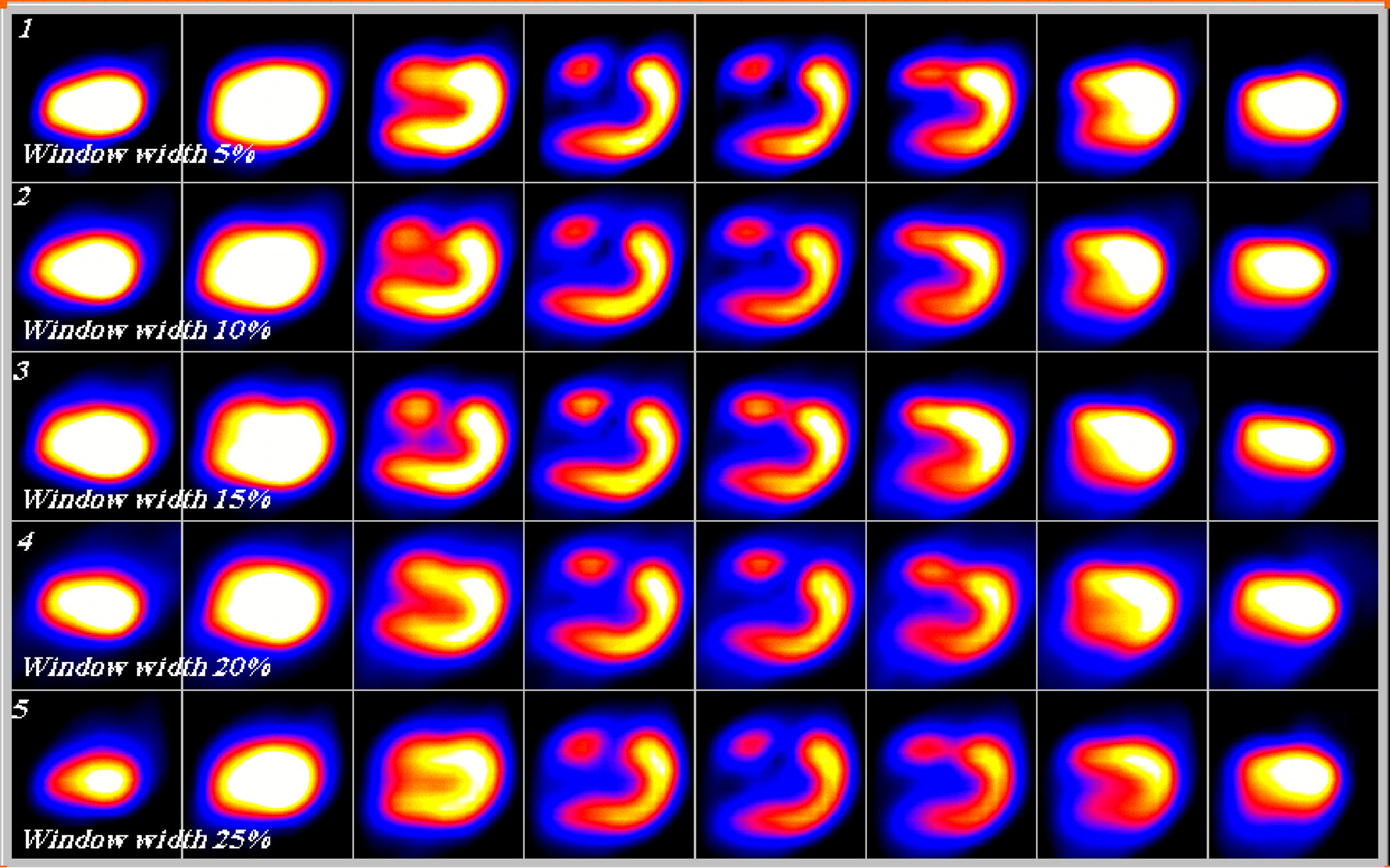
Five rows (1–5) of vertical long axis cuts of a heart phantom SPECT at window widths of energy 5%, 10%, 15%, 20% and 25%, and 0% off-peak shift.
4 Discussion
The most sensitive indicator of gamma-camera performance is uniformity, because it is carried out on a daily basis. Moreover, it is the principle tool in evaluating the status of a gamma camera. Most artifacts, related to the effect of integrity of the detector head, computer system and hard-copy device on image uniformity, have been investigated (Groch and Erwin, 2000, 2001). The common sources of artifacts are non-uniformity in gamma-camera detectors, center of rotation errors, misaligned cameras on multi-detector scanner systems, errors in image reconstruction, patient motion and radiotracer uptake in non-target organs and attenuation (Young et al., 1990). In the present study, we investigated the effect of widow widths of energy 5%, 10%, 15%, 20% and 25% on Planer and SPECT images using a Tc-99m source at energy 140 keV. IU% and DU% of CFOV and UFOV and window widths of energy 5%, 10%, 15%, 20% and 25% were calculated. Off-peak shift of energy was at 0% during all experiments with the window centered at the middle of the peak. We conclude that the calculated IU% and DU% of CFOV and UFOV showed changes at window widths 5%, 10% and 25%, which indicated marked changes in image uniformity. For window width of energy 15–20%, there was no clear change in the calculated values of IU% and DU% of CFOV and UFOV, which indicated optimum energy uniformity. Moreover, energy window width ⩾25% indicated loss in image uniformity. It is evident that energy window width plays a prominent role in flood image uniformity using a Tc-99m source.
To elucidate the effects of energy window width % on SPECT images, a heart phantom with an artificial defect in the anterior wall of the heart at five different window widths of energy 5%, 10%, 15%, 20% and 25% with the same parameters in each acquisition was investigated. SPECT images were clinically interpreted by a physician who reported different diagnosis for each energy window width due to changes in perfusion. Among possible significant factors not dealt with in the present study, an investigation of the effects of thallium-201 on planner and SPECT image uniformity is recommended, as thallium-201, at least in Europe, is still a frequently used tracer for heart studies.
References
- Proposal for a quality control procedure for rotating gamma camera tomographic systems. Radiol. Med.. 1987;74(1–2):109-115.
- [Google Scholar]
- Myocardial single-photon emission computed tomographic quality assurance. J. Nucl. Cordial.. 1996;3(2):157-166.
- [Google Scholar]
- The influence of collimators on SPECT center of rotation measurements; artifact generation and acceptance testing. J. Nucl. Med.. 1988;29(8):1393-1397.
- [Google Scholar]
- Nuclear Medicine Pocket Handbook. Amersham International Plc; 1993. pp. 6–7
- How to detect and avoid myocardial perfusion SPECT artifacts. J. Nucl. Med.. 1994;35(4):699-702.
- [Google Scholar]
- Single-photon emission computed tomography. Instrumentation and quality control. J. Nucl. Med. Technol.. 2001;29:12-18.
- [Google Scholar]
- IAEA, 1991. Quality control of nuclear medicine instrumentation.
- Thallium imaging with single photon emission computed tomography. Am. Heart J.. 1987;114(4):852-865.
- [Google Scholar]
- Quantification of SPECT myocardial perfusion images; methodology and validation of the Yale_CQ method. J. Nucl. Cardiol.. 1999;6(2):190-204.
- [Google Scholar]
- Effects of centre-of-rotation shift on contrast and spatial resolution of the SPECT system. Nucl. Med. Commun.. 1986;7(5):373-379.
- [Google Scholar]
- Reproducibility and action levels for gamma camera uniformity. Nucl. Med. Commun.. 1990;11(2):95-101.
- [Google Scholar]
Further reading
- Text Book of Nuclear Medicine Technology (4th ed.). London: Mosby; 1995. pp. 180–248
- NEMA, 1994. Performance Measurements of Scintillation Cameras, Standards Publication 1.
- Instrument and computer-related problems and artifacts in nuclear medicine. Semin. Nucl. Med.. 1996;26(4):256-277.
- [Google Scholar]
- Physics in Nuclear Medicine (second ed.). New York: Grune and Stratton; 1987.
- Spies, S.M., 2000. Oral communications. An example of an initial bone scan using the Starbrite TM crystal system.
- Increased sensitivity through use of overlapping 180 degrees orbits in clinical myocardial perfusion imaging. Eur. J. Nucl. Med.. 1995;22(6):543-547.
- [Google Scholar]







