Translate this page into:
Cross talk between complete blood count and progression of type II diabetes mellitus
⁎Corresponding author. mamoona.noreen@gmail.com (Mamoona Noreen),
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Background
Diabetes mellitus (DM) is a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. The most common type is type II diabetes and is characterized by insulin resistance or relative insulin deficiency.
Objectives
This study was performed to discover whether Complte blood count is a suitable indicator for development of type II diabetes complications.
Methods
137 type II diabetic patients with high blood glucose level were included in this study and their complete blood count was recorded. Demographic and laboratory data were also noted.
Result
WBC, Hb, Hematocrit, MCH had abnormal values. As the results of this study show, higher leukocyte counts was correlated with uncontrolled diabetes. Accompanied by other markers, chronic inflammation that can be shown by this factor could be related to pathogenesis and the progression of these diabetes-related complications.
Conclusion
Complete blood count test could be considered as an appropriate clinical examination for early diagnosis and prevention of microvascular and macrovascular complications thus reducing morbidity and mortality from diabetes mellitus.
Keywords
Diabetes Mellitus
Blood
Complete Blood Count
Blood Cells
Diabetic Complications
1 Introduction
Diabetes Mellitus (DM) is a faction of metabolic disorder indicated by an excessive blood sugar usually resulted from deformity in insulin flow, insulin activity or both. The incurable hyperglycemia of DM is consociated with prolonged harm and other complications such as weak eyesight, renal failure, nervousness, cardiac infraction and vascular disease. (Gilmer et al., 2005; Safi, 2017). The carbohydrate, fat and protein metabolism abnormalities are due to insulin’s inadequate response to body cells and tissues resulting from hyperinsulinaemia. It was predicted that the prevalence of diabetes among people aged 20–79 years was 6.4 percent of about 285 million people worldwide diagnosed with diabetes (Shaw et al, 2010). As demonstrated by International Diabetes Federation (IDF), Pakistan now has the 10th largest population of diabetic individual and will be ranked fourth in 2025. The WHO published the first globally acknowledged classification in 1980. The two major types of diabetes are classified as Type I; Insulin dependent diabetes mellitus (IDDM) and Type II; Non-insulin dependent diabetes mellitus (NIDDM).
If insulin secretion is restricted, the entry of glucose towards cells will be blocked, resulting in hyperglycemia. The same issue can be observed if insulin secretion is regular, but perhaps the target cells are not able to use it effectively. The level of hyperglycaemia may be affected by various hormones. Insulin has the potential to lower hyperglycemia (Meley et al, 2006). DM can occur with particular symptoms such as dry mouth, fatigue, polyuria, blurring of focused vision, exhaustion and weight loss. Most of the symptoms are not dreadful, and might not even appear. (Report of a WHO Consultation, 1999). In those individuals who are at greater risk of having diabetes, activity of beta cells stop, ultimately increases the productivity of impaired glucose tolerance and eventually initiates DM (Bloomgarden, 1998; DeFronzo et al., 1992; Stumvoll et al., 2005).
According to various studies, a number of characteristics, such as obesity, elevated plasma glucose, hypercholesterolemia (high cholesterol and low higher densities lipoprotein (HDL), high triglyceride and hypertension are th key risk factors in progression of DM (Taskinen, 2003; Reaven, 1998). Inflammatory responses of the immune system can be identified by increasing levels of plasminogen activator inhibitor-1 (PAI-1), white blood cell (WBC) count and concentrations of cytokines. Because of it's statistical association among insulin resistance markers and inflammation, it has been noted that dysfunction of immune system may play a significant role in the development of type II DM (Pratley et al, 1995; Pickup and Crook, 1998; Festa et al, 2000; Weyer et al, 2000). Higher WBCs have been shown to play an important role in the advancement of diabetic complications (Tong et al, 2004). WBCs may also be triggered by the inflammatory responses, angiotensin II and glycaemic end-products, which may in turn results from hyperglycemia, and may trigger factors such as interleukin β1 and tumor necrosis factor-α (TNF-α) associated with severe diabetes pathophysiology and health problems. (Andersen et al., 1996; Esposito et al., 1989; Heidland et al., 2001). Data analysis of 20 studies, including 90,000 people, showed a positive interconnection between the elevated WBCs level and the risk of diabetes (Gkrania-Klotsas et al, 2010). The aim of our study was to reveal the possible corelation of CBC as an innovative marker for inflammatory response with vascular complications and chronic disease in diabetic patients of Southern Punjab, Pakistan.
2 Materials and methods
This research was held after the virtual approval from the institute and patients consent. Haleema Medical Complex, Multan was choosen for data collection and study conduction. 160 individuals of both genders were included in this study. Random blood sugar of all participants was tested. For this venous blood sample (3 ml) was taken from individuals. After collection blood was immediately centrifuged for serum separation. Gluose reagent was used for enzymatic detection of serum glucose. Among 160 participants, 137 were diabetic including 77 males and 60 females.
3 Biochemical analysis
Complete Blood Count (CBC) including hematocrit, WBC, MCH, RBC, Hb, mean corpuscular volume (MCV), platelets, eosinophils, monocytes, lymphocytes, polymorphs and MCHC count of 137 patients was checked by hematology analyzer (Sysmex KX-21) from blood plasma.
4 Statistical analysis
GraphPad Prism (Version 5) was used for statistical data analysis. Independent t-test was done and P value < 0.05 was considered as significant.
5 Results
The normal range of WBC is 4000-11000 (cells/mm). Out of total 137 diabetic patients 39 had high (Fig. 1) while 95 had normal WBC count (P < 0.05). 137 patients including 60 women and 77 men had undergone hemoglobin test (Figs. 2 and 3). 4 females and 3 males had high level while 30 males and 30 females had lower level of hemoglobin (P < 0.05). Normal range of Hb for male and female is 13.5-17.5g/dl and 12.0-15.5g/dl respectively. Platelets count of 11 patients was high while 10 had low levels with 116 being normal (Fig. 4). Normal range of platelets is 150,000-450,000. Among total subjects, 102 patients had high value of polymorphs and 34 had normal range (P < 0.05) (Fig. 5). Lymphocytes and monocytes level was also checked in 137 patients (Figs. 6 and 7). All the patients had normal value of eosinophils (Fig. 8); its average range in the blood is 0-6%.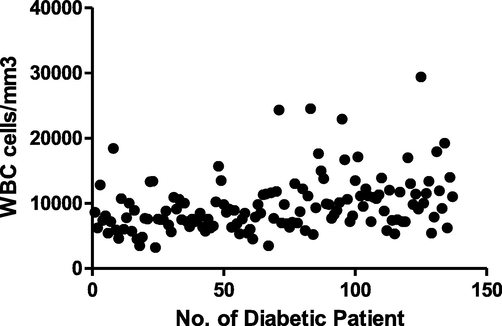
Scatter plot indicating the level of white blood cells among diabetic patients.
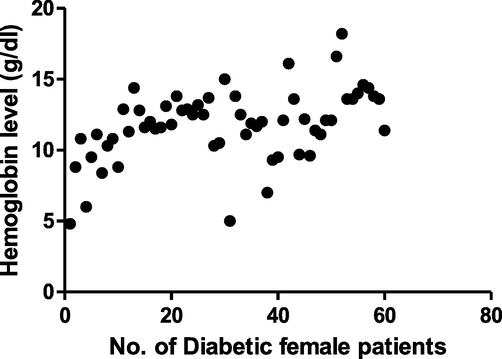
Scatter plot representing the level of hemoglobin in female diabetic patients.
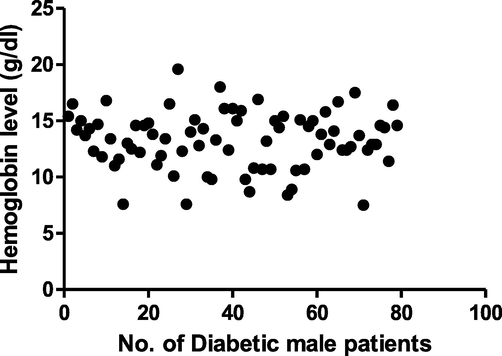
Scatter plot representing the level of hemoglobin in male diabetic patients.
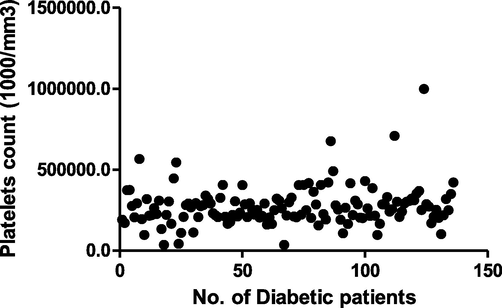
Scatter plot indicating the level of platelets in diabetic patients.
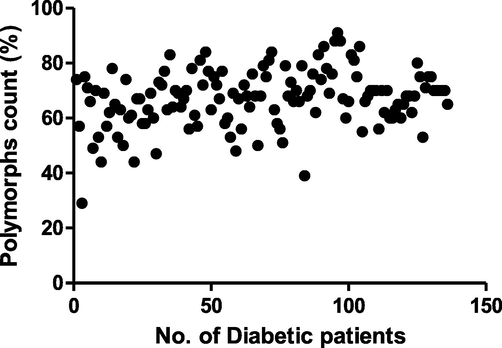
Scatter plot indicating the level of polymorphs in diabetic patients.
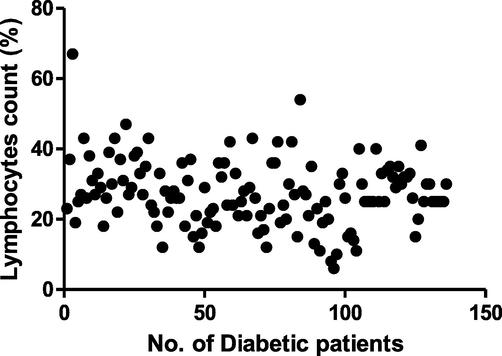
Scatter plot indicating the level of lymphocytes in diabetic patients.
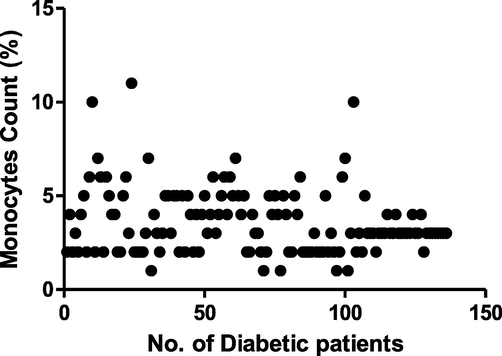
Scatter plot indicating the level of monocytes in diabetic patients.
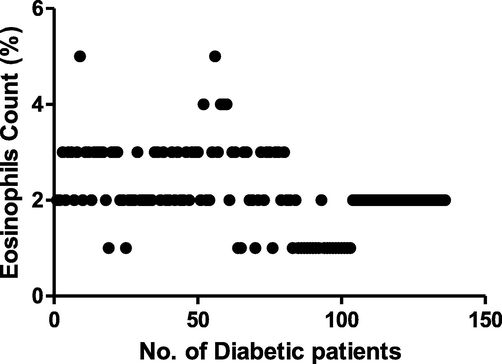
Scatter plot indicating the level of eosinophils in diabetic patients.
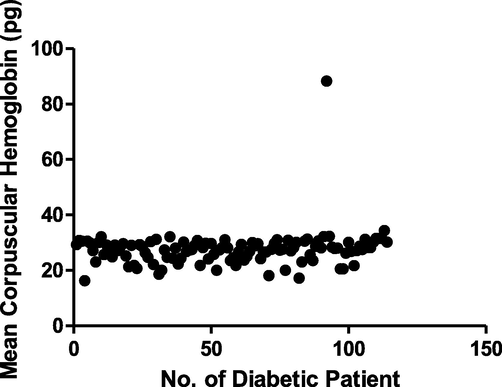
RBC, hematocrit, MCV, MCH and MCHC of 114 (48 female and 66 male) patients were also analyzed. Among total subjects, 34 patients had low MCH values while 79 patients had normal values (Fig. 9). The difference was found to be significant (P < 0.05). Average range of MCH is 26-34 pg. Among 66 male subjects, 9 had high, 6 had low while 51 patients had normal range of RBCs (Fig. 10). Among 48 female subjects, 4 had elevated RBCs, 15 had low while 29 had normal RBCs (Fig. 11). Normal range of RBC for men and women is 4.7-6.1 and 4.2-5.4 million cells per microliter (µl) of blood, respectively. Hematocrit level of 114 patients (63 males and 51 females) was also analyzed (Figs. 12 and 13). 2 females and 3 males exceeded normal level while 33 females and 36 males had drastically low level of hematocrit (P < 0.05). Its normal range in female is 37-48% while in males its range is 45-52%. Among total patients, 45 had low MCV level whereas 69 patients had normal range. None of them had high level MCV (Fig. 14). Standard range of MCV is 79-98 fl. 10 diabetic individuals had elevated MCHC, 33 had low and 71 had normal range (Fig. 15). Normal range of MCHC is 32-36 g/dl.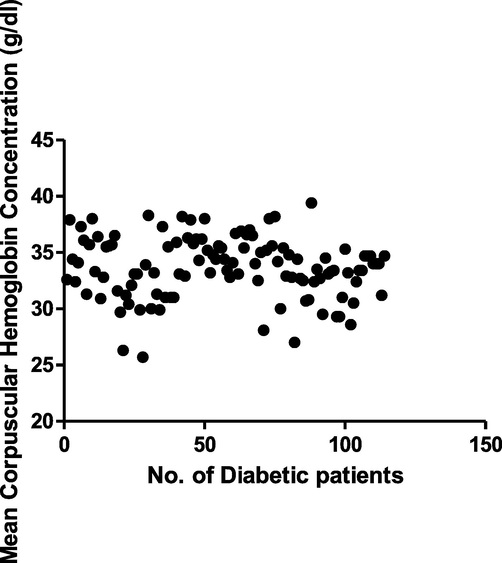
Scatter plot representing the level of mean corpuscular hemoglobin concentration in diabetic patients.
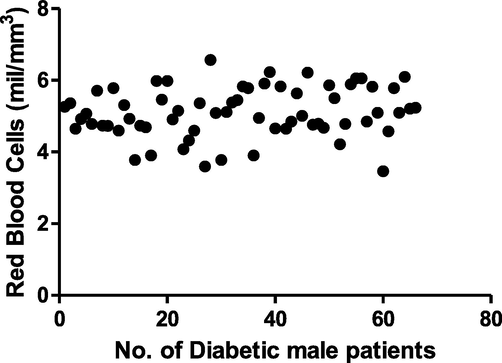
Scatter plot showing the level of red blood cells in diabetic male patients.
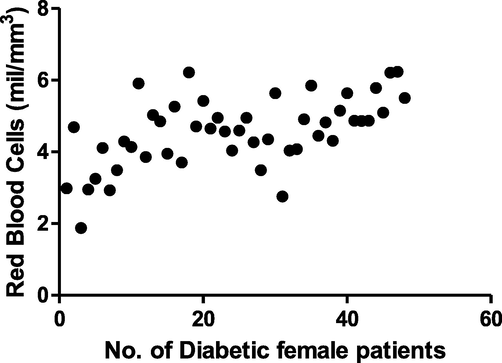
Scatter plot showing the level of red blood cells in diabetic female patients.
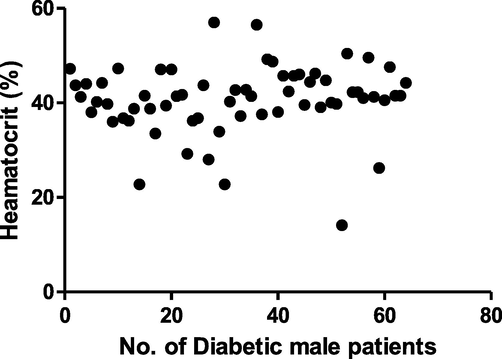
Scatter plot representing the level of hematocrit in male diabetic patients.
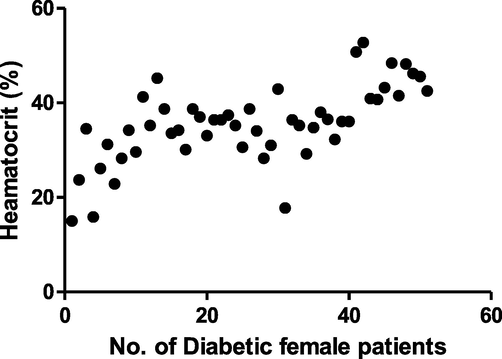
Scatter plot showing the level of hematocrit in female diabetic patients.
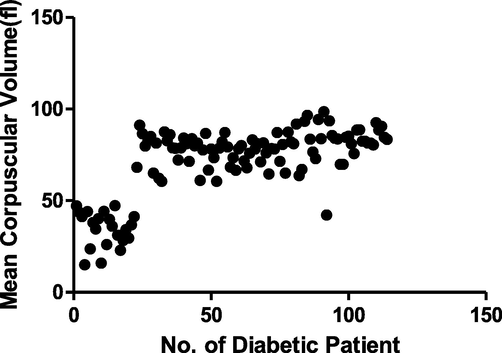
Scatter plot indicating the level of mean corpuscular volume in diabetic patients.
Scatter plot indicating the level of mean corpuscular hemoglobin concentration in diabetic patients.
6 Discussion
Diabetes mellitus (DM) can occur due to obesity and sedative choices of lifestyle. Changing lifestyles, including a balanced diet, moderate exercise and a weight status according to BMI, are essential for diabetic patients. This current study aims to evaluate the connection of CBC as an innovative marker for inflammatory response with vascular complications and chronic disease in diabetic patients. CBC is a financially and comfortably available laboratory test that can demonstrate chronic inflammation. This study was conducted to investigate hematological parameters and metabolic reactions among patients with diabetes. 137 people with diabetes were included and the CBC was checked. CBC includes WBC count, RBCs, hemoglobin level, platelet count, polymorphs, lymphocyte count. hematocrit, MCV, MCH and MCHC. WBC count is a vital biomarker of inflammatory process, damaged tissue and other degenerative diseases. Research has shown that the increase in WBC count is strongly correlated with progressive coronary artery disease (Friedman et al., 1974). It also increases the frequency, fatality rate and incidence of CVD (Kannel et al., 1992). The increase in WBC count is strongly related to chronic complications of DM. In this study WBC, Hb, polymorphs and MCH from normal range was seen to be significantly associated with DM (P < 0.05).
Various markers of inflammation can be demonstrated by a CBC factor that can be associated with the initiation and progression of DM.
Of the 137 diabetic patients, the majority had low hemoglobin levels (Fig. 2, Fig. 3). Hematocrit was found to be considerably low in both male and female patients (Fig. 12, Fig. 13). But many patients had normal values for MCV, MCH and MCHC however, few patients had unusually low levels of MCH and MCHC (Fig. 9, Fig. 15). Out of 137 people with diabetes, most patients had a healthy level of platelet counts whereas 11 patients had absurdly high and 10 patients had decreased platelet counts (Fig. 4). Increase in the average platelet volume is a significant predictor for impaired micro as well as macrovascular complications among diabetic patients (Hekimsoy, 2004). Platelet functional abnormality begins at the onset of diabetes even before the occurrence of vascular pathology. In our study, the majority of patients had extraordinarily high polymorphs (Fig. 5). The increase in the number of polymorphs is associated with the development of thrombus and ischemic damage (Haumer et al., 2005; Stewart, 1993; Arruda-Olson et al., 2009). Different subtypes of WBC may show various aspects of inflammatory reactions or acute infectious diseases. Previous research suggests that high levels of polymorphs and comparative low levels of lymphocytes in the blood are an independent fatality rate risk factor with chronic cardiac arrest in people with diabetes (Arruda-Olson et al., 2009; Rudiger et al., 2009).
It's also associated with this current study that lymphocytes were abnormally low in most diabetics, although few patients had elevated lymphocyte levels (Fig. 6). Almost all patients had perfectly natural monocyte and eosinophilic value (Figs. 7 and Fig. 8).
Multiple researches have shown that the function of differential leukocyte counts is regarded to be an independent risk factor of diabetes (Prentice et al., 1982; Olivares et al., 1993; Sweetnam et al., 1997). Despite this, it is still unknown that which subtype of the WBC does play more significant role. Researches have been trying since several years to identify the inflammatory biomarker as an independent prognostic for complications related to diabetes. (Stamler et al., 1993; Ross, 1999; Weijenberg et al., 1996; Tong et al., 2004; Heidland et al., 2001). In addition to regular physician check-ups, the WBC test may be added to diabetes standard precautions as an early predictor of diabetes. The CBC test may show the inflammatory activity of the entire body. The results of this study revealed that higher WBCs were independently interlinked with micro and macro-vascular diabetic complications. CBC can therefore be regarded as an economic test which can help to assess that diabetic people are at an increased risk of developing diabetic complications and can help in preventing them from dying and suffering from disease complications.
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research at the King Saud University for funding this work through research group no. RG-1441-356.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Interleukin-1B-induced nitric oxide production from isolated rat islets is modulated by D-glucose and 3-isobutyl-1-methylxanthine. Eur. J. Endocrinol.. 1996;134(2):251-259.
- [Google Scholar]
- Neutrophilia predicts death and heart failure after myocardial infarction: a community-based study. Circ. Cardiovasc. Qual. Outcomes. 2009;2(4):656-662.
- [Google Scholar]
- Endothelial receptor-mediated binding of glucose-modified albumin is associated with increased monolayer permeability and modulation of cell surface coagulant properties. J. Exp. Med.. 1989;170(4):1387-1407.
- [Google Scholar]
- Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102(6):42-47.
- [Google Scholar]
- The leukocyte count as a predictor of myocardial infarction. N. Engl. J. Med.. 1974;290(3):1275-1278.
- [Google Scholar]
- Predictors of health care costs in adults with diabetes. Diabetes Care. 2005;28(1):59-64.
- [Google Scholar]
- Differential white blood cell count and type 2 diabetes: systematic review and metaanalysis of cross-sectional and prospective studies. PLoS ONE. 2010;5(2):13405.
- [Google Scholar]
- Association of neutrophils and future cardiovascular events in patients with peripheral artery disease. J. Vasc. Surg.. 2005;41(5):610-702.
- [Google Scholar]
- Advanced glycation end products and the progressive course of renal disease. Am. J. Kidney Dis.. 2001;38(4):100-106.
- [Google Scholar]
- Mean platelet volume in Type 2 diabetic patients. Journal of Diabetes and its Complications. 2004;18(3):173-176.
- [Google Scholar]
- White blood cell count and cardiovascular disease: insights from the Framingham Study. JAMA. 1992;267(2):1253-1256.
- [Google Scholar]
- Monocyte count: a risk factor for coronary heart disease? Am. J. Epidemiol.. 1993;137(4):49-53.
- [Google Scholar]
- Is type II diabetes mellitus a disease of the innate immune system? Diabetologia. 1998;41(10):1241-1248.
- [Google Scholar]
- Relation of the white blood cell count to obesity and insulin resistance: effect of race and gender. Obes. Res.. 1995;3(1):563-571.
- [Google Scholar]
- Leukocyte counts and coronary heart disease in a Japanese cohort. Am. J. Epidemiol. 1982;116(3):496-509.
- [Google Scholar]
- Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1998;37(12):1595-1607.
- [Google Scholar]
- Rudiger, A., Burckhardt, O.A., Harpes, P., Muller, S.A., and Follath, F. (2006); (2009). The relative lymphocyte count on hospital admission is a risk factor for long-term mortality in patients with acute heart failure. Am. J. Emerg. Med., 5(3) :451–4.
- Alteration in Ocular Blood Flow and Its Effect on the Progression of Glaucoma. International eye science. 2017;17(3):394-398.
- [Google Scholar]
- Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract.. 2010;87(1):4-14.
- [Google Scholar]
- Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16(2):434-444.
- [Google Scholar]
- Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365(9467):1333-1346.
- [Google Scholar]
- Total and differential leukocyte counts as predictors of ischemic heart disease: the Caerphilly and Speedwell studies. Am. J. Epidemio. 1997;145(6):416-421.
- [Google Scholar]
- Diabetic dyslipidaemia: from basic research to clinical practice. Diabetologia. 2003;46(6):733-749.
- [Google Scholar]
- White blood cell count is associated with macro and microvascular complications in Chinese patients with type 2 diabetes. Diabetes Care. 2004;27(4):216-222.
- [Google Scholar]
- White blood cell count and the risk of coronary heart disease and all-cause mortality in elderly men. Arterioscler. Thromb. Vasc. Biol.. 1996;16(5):499-503.
- [Google Scholar]
- Insulin action and insulinemia are closely related to the fasting complement C3, but not acylation stimulating protein concentration. Diabetes Care. 2000;23(4):779-785.
- [Google Scholar]







