Bisoprolol oral treatment of heart failure rats: Involvement of calmodulin
⁎Corresponding author. fzbxinnei@sina.com (Zhanbin Feng)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Objectives
The current study is to estimate the bisoprolol (BOP) oral treatment of rats against the myocardial infarction (MI) administrated by using isoproterenol (ISO).
Methods
Treatment of rats are MI administration by subcutaneous for two successive days of ISO (85 mg/kg). The tissue of heart is removed without delay, it is washed used isotonic chilled saline in this study. Plasma is separated from the collected rat blood and further analysis of biochemical parameters were carried out.
Results
Group of ISO-treated rats have increased levels of glucose in blood, also observed the activity of lipids in plasma along fibres of muscle with hyalinization, compared to BOP treated rats, and ISO + BOP treated rats. The parameter values of BOP administered rat were close to control rats. Reports clearly state that ISO + BOP treated rat tissue of heart damage is reduced when compared to ISO treated rats.
Conclusions
Rats were treated with ISO + BOP to defend against hyperlipidaemia and tissue of cardiac damage and followed by MI. Hence, to investigate the biochemical and biophysical BOP mechanism against MI risk in rats.
Keywords
Bisoprolol
Heart failure
ISO
Glucose
Lipids
- BOP
bisoprolol
- MI
myocardial infarction
- ISO
isoproterenol
- LDL-C
cholesterol with lesser density
- HDL-C
high density of lipoprotein cholesterol
- CVD
cardiovascular diseases
- LV
left ventricular
- COPD
chronic obstructive pulmonary disease
- CaM
calmodulin
- NCLAS
national centre for laboratory animal sciences
- AC
air condition
- TG
triglycerides
- CK
creatinine kinase
- LDH
lactate dehydrogease
- AST
aspartate transaminase
- ALT
alanine transaminase
- NAD
nicotinamide adenine dinucleotide
- DNPH
2,4-dinitrophenylhydrazine
- CaCaM
canonical Ca2+ loaded CaM
Abbreviations
1 Introduction
The disproportion of myocardial demand of oxygen supply directs to necrosis of heart muscle known as MI. The higher levels of hypercholesterolemia and hyperlipoproteinemia of low density lipoprotein cholesterol (LDL-C), lower levels of high density lipoprotein cholesterol (HDL-C) are the leading risk factors for MI (Khader et al., 2003). The stress in the heart muscle is induced by ISO which is catecholamine that leads to necrosis of myocardium (Sushamakumari et al., 1989). The blockage in the arteries along with cardiovascular diseases (CVD) is caused by ISO elevates lipoproteins and lipids specifically LDL-C seen in blood circulation (Goldstein and Brown, 1984). MI is caused due to the release of oxygen free radicals by ISO (Singal et al., 1982). These oxygen free radicals and oxidative stress jointly leads to atherosclerotic lesions generation by formation of oxidized LDL from LDL, which is the base cause of MI (Libby, 2003). The failure of heart, neurohumoral axes gets active, along with the sympathetic nervous system. Myocardial remodelling, prognosis (Elser et al., 1997) and cardiac dysfunction levels have an effect on sympathetic activity. The sympathetic and inflammatory activities may partially antagonized by beta blockers, affecting hypertrophy and cardiomyocyte apoptosis which leads to attenuated development of ventricular remodelling and raise in ejection fraction (Fringerio and Roubina, 2005). Some experimental studies have established on how the beta-blockers shows an effect in falling mortality rate among patients with failure of heart in different functional classes (Domanski et al., 2003), and with recommend guidelines that left ventricular (LV) systolic dysfunction of the patient shall be treated with beta-blockers (ACC/AHA, 2005). To control the high blood β1-adrenergic blocking agent is used which is BOP a cardiac selective (Albouaini et al., 2007). To minimise the multiple doses of antihypertensive drugs instead it can be used once in a day for a long half life. Generally BOP is well suitable, due to the β1-adrenergic selectivity receptor and acts as a substitute to non-selective and β-blocker drugs use to treat of hypertension induced zebeta. Report clearly mentioned this use alone or in combination/alone with another drugs to manage hypertension (Albouaini et al., 2007). The patients suffer with COPD (chronic obstructive pulmonary disease) is useful for selective receptors in patients. Clinical and hemodynamic status was improved by BOP therapy, and the heart failure of different etiologies, cardiac function in COPD patients, it includes Chagas’ disease, though, improvement of exercise capacity and is not done. Other studies mentioned BOP was safe and tolerated well in different etiologies, in cardiac patients. Another study from the placebo-controlled and tolerated the medication rate is 76.5% (CIBIS, 1994) which is not different from the other report. Medication in Chagas’ disease tolerates the dose up to 10 mg, the symptoms are improved and functions of ventricular comparison to other etiologies patients. BOP and Chagas’ disease is the first report to use and attention of possibility of myocardiopathy and interaction of BOP mechanism. Oxidative modifications in specific sites are identified Ca-ATPase expressed and calmodulin (CaM) in membrane sarcoplasmic reticulum, it arise oxidative stress response (Gao et al., 1998b; Viner et al., 1999). CaM is oxidized to their equivalent methionine sulfoxides, and biological aging methionine and loss of functions where as specific nitration of tyrosines in the Ca-ATPases and related sites. The oxidation of methionines and regulatory role in signaling of calcium coupling and calcium are two types of modifications post translation and CaM function and cellular redox conditions (Sun et al., 1999; Squier and Bigelow, 2000; Yermolaieva et al., 2000). The present study to investigate the ISO induced heart failure rats and BOP dose response in plasma lipid profile, cardio marker enzymes and involvement of CaM mechanism.
2 Experimental methodology
2.1 Experimental design and procuring animals
60 days old thirty two albino Wistar strain of male rats, body weight ranging from l20-140, were taken from NCLAS, Hyderabad, Telangana, India and quarters in cage separately Air Condition (AC) room (25 + 1 °C) during 7.00 a.m to 7.00p.m. Experimental animals divided into four groups in each one 8 rats. Group I consisted of normal/control rats equivalent amounts of distilled water instead of BOP (Antihypertensive Drug), Group II we design to develop a heart failure MI model in rats e. g. ISO induced heart failure model rats 85 mg/kg body weight/day (Rajadurai et al., 2006) do not consider this hypertrophy. Group III which received markedly available BOP is available under the following brand name: Zebeta was given 14 days or 30 min after MI, body weight per day 60 mg/kg). Group IV ISO administrated + BOP treated rats. All the rats were recorded daily weight and intake of food and water was followed on days of alternate. The finishes of the investigational period, in each group of rats were fasted overnight and then by using of cervical dislocation rats were sacrificed. Collected tissues and immediately for further analysis for processed. The animal study, we are followed all procedures of including the whole surgical, feeding, and raising process were based on approved methods by the committee of animal ethical clearance for the treatment of animals and approved for the study protocol was obtained subsequent the guiding principle. Current study was also accepted by institutional ethical committee, Ninth Hospital of Xi’an, Ethic Number: 201917.
2.2 Blood collection and sample processing
Blood was collected from rats by cardiac puncture allows the collections of large amount of blood during the time at 7–10 a.m. in heparinised tubes, total proteins and albumins in plasma (Lowry et al., 1951), uric acid were analyzed using auto analyzer kit methods, urea, creatinine (Slot, 1965) were estimated using kit method in spectrophotometer. Plasma TG (triglycerides) using (Fossati and Principe, 1982) method Cholesterol estimation using by (Allian et al., 1974) estimated glucose was (Trinder, 1969). Phospholipids by (Connerty et al., 1961). Plasma Creatinine Kinase (CK), activity, was estimated by using (Sharma and Nand, 2006). Free fatty acids estimation by Moore and Stein (1948).
2.3 LDH AST and ALT activities
Estimation of (LDH) Lactate dehydrogease by the method of (Goldberg et al., 1988). 1 ml of substrate buffer is taken in a tube and adds 0.1 ml of sample along with NAD solution after which it has to be incubated for 15 min. Added reagent of 1 ml DNPH arrest the reaction. Again it is incubated at 37 °C for 15 min and added serum 0.1 ml to empty test tube with DNPH reaction was arrested, colour developed after added 7 ml of sodium hydroxide solution at 420 nm measured. AST (Babson et al., 1962), ALT (Matsuzawa and Katunuma, 1966) activities are assayed in separate tubes; one ml of substrate buffer added to the sample of 0.1 ml incubates it for 30 min at 37 °C. The reaction is arrested after adding the reagent 1 ml DNPH. Let the tubes rest for 15 min and sodium hydroxide of 10 ml added and absorbed at 520 nm.
3 Results and discussion
Observed results that exposed in ISO treated rat leads to heart injury with significant increased change in the cardiac marker enzymes CK, LDH, AST and ALT. In ISO + BOP treated group IV results were nearly normal levels and BOP treated alone group also same when compared to controls rats in (Fig. 1). Blood glucose, serum urea, uric acid, creatinine in group II ISO treated rats has a significant increase and it showed a significant increase in the levels of these parameters. Plasma protein contents increase in experimental subjects of ISO, ISO + BOP rats but not BOP group III when compared to control group I (Fig. 2). Anandan et al. reported (2007) involvement of lipids plays important role in cardivalcular disease (CVD). Hypercholesterolaemia and hyperlipidaemia are the very important factors in cardiac risk and MI progress. ISO treated and MI includes elevated lipid levels are circulatory. Our reports, ISO treated rat’s shows increase levels of TGs, Total cholesterol significantly in plasma levels with increase free fatty acids (Fig. 3). Cardiovascular disturbances and MI is the primary risk factors to increased level of TGs (Sushama Kumari et al., 1990). Increased levels significant in plasma phospholipids of ISO treated rats and ISO + BOP treated rats were clearly observed that the levels are decreased near to normal control range which might be appropriate to the decrease of hypolipidemic and hypocholesterolaemic activities in present reports are supported to previous results (Anandan et al., 2007). ISO create hypoxia or relative ischemia with the effect of coronary hyperactivity in myocardium and hypotension in heart (Bloom and Davis, 1991), the overload of cytosolic Ca2+ induces myocardial ischemia in ISO group (Singal et al., 1983). The level of glucose in blood increased while comparing with the controls. The difference increase may be appropriate to the improved lipolysis and glycogenolysis, with the start of phosphorylase kinase enzyme and β-adrenergic receptor. On testing enzymes in the heart tissue is at a low level and microscopic myocardial necrosis and gross is produced by ISO treated rats. Though there are many beneficial effects and drugs are well standardized model studies to cardiac functions in clinical and mimics of MI due to ischemia in rats induces ISO (Harada et al., 1993). In CVD lipids are major role played by not only development of atherosclerosis and hyperlipidaemia, and modification of cell composition and stability of structure of cell membranes (Rajadhurai and Prince, 2005). Increased lipid values in plasma that are administrated rats with ISO. The ISO treated rat’s shows increase in plasma triglycerides and cholesterol this might be due to increase in adenosine monophosphate in cardiac cycle followed by biosynthesis of lipids (Paritha and Devi, 1997). The key role of eukaryotic cells in deciphering the signalling of Ca2+ is due to the CaM that acts as primary indicator of intracellular calcium (Ca2+). Being the secondary messenger, the CaM interacts/reacts with large number of proteins which is not unusual (Fig. 4). Every lobe is exposed with hydrophobic patches this firm changes are due to the binding of CaM and it helps to bind hydrophobic anchor residues in large that is present in canonical Ca2+ loaded CaM (CaCaM) which is a target binding sequences. The channels NaV1.5 are huge, consisting subunit (a) pore-forming (∼220 kDa) and subunit (b) one of four auxiliary (b1–4, 30–35 kDa) in heterooligomeric assemblies which involve in function and channel trafficking. The cytosolic subunit (b) joins as the linker region in connecting DI and DII, adapt CaV1.2 voltage dependent activation and inactivation in ISO + BOP administrated rats (Yamniuk and Vogel, 2004; Bodi et al., 2005; Nerbonne and Kass, 2005; Abriel, 2010; Catterall, 2011).
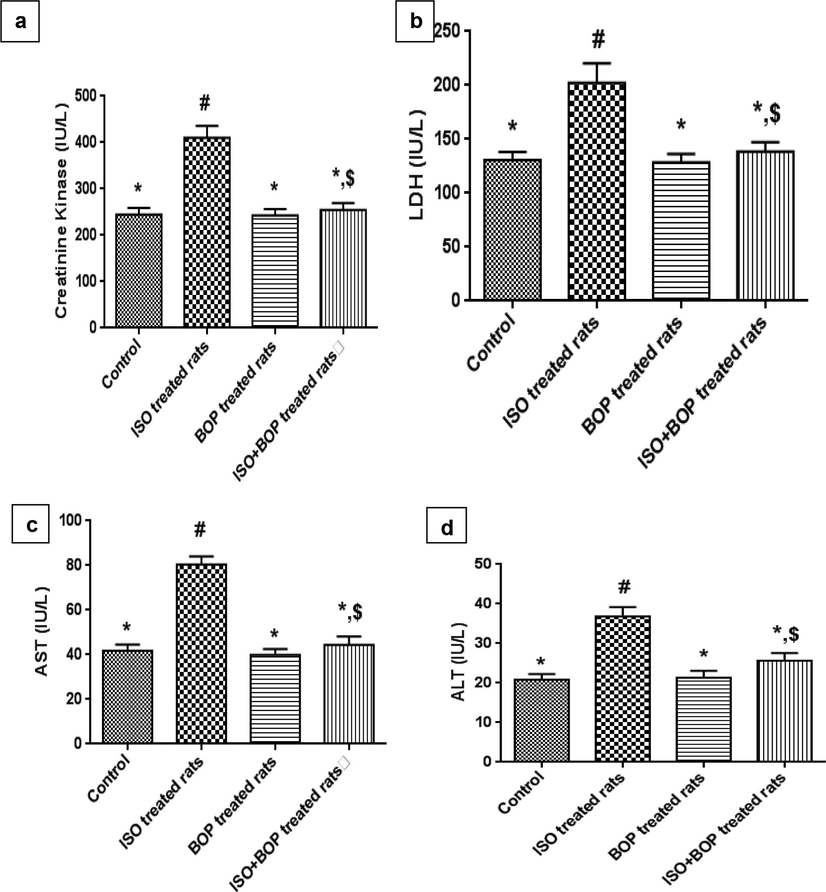
- Effect of isoproterenol and bisoprolol administration on cardiac marker enzymes. Values are expressed as Mean ± SEM, on each bar followed by the same symbol are not significantly different (P ≤ 0.05) from each other according to Duncan’s Multiple Range (DMR) test, n = 8, Control = Control rats.
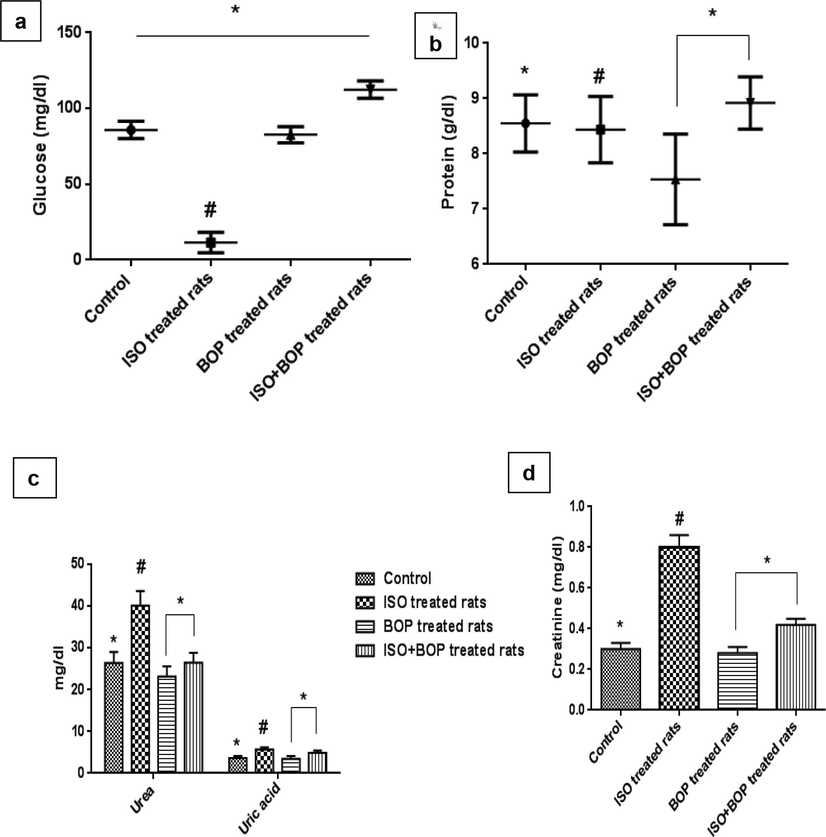
- Effect of isoproterenol and bisoprolol administration on plasma components Values are expressed as Mean ± SEM, on each figure/bar followed by the same symbol are not significantly different (P ≤ 0.05) from each other according to Duncan’s Multiple Range (DMR) test, n = 8, Controls = Control rats.
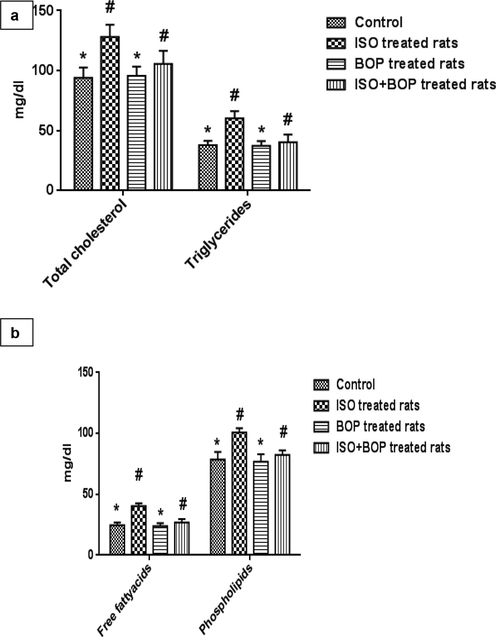
- Effect of isoproterenol and bisoprolol administration on plasma lipid profile. Values are expressed as Mean ± SEM, on each bar followed by the same symbol are not significantly different (P ≤ 0.05) from each other according to Duncan’s Multiple Range (DMR) test, n = 8, Controls = Control rats.
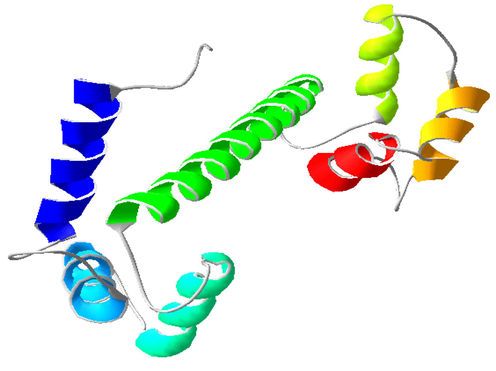
- 3D structure of Ca2+ bound calmodulin (PBD:1OSA).
4 Conclusion
Rats were administered BOP parameters were close to control rats. Reports clearly stated that ISO treated rat tissue of heart damage was reduced when compared to treated ISO + BOP rats. The models were treated with ISO + BOP to defend against hyperlipidaemia and tissue of cardiac damage followed by MI. Hence, to investigate biochemical BOP mechanism against MI risk in rats. More in strength studies are needed to interact of BOP and ISO treated experimental animals.
5 Statistical investigation
The consequences are states that mean ± SEM. (DMR) impact was set at (P ≤ 0.05).
Acknowledgements
The authors are thankful to the Xi'an Municipal Health Planning Commission Bureau Level Research Fund (J201802035) for financial assistance.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Cardiac sodium channel Na(v)1.5 and interacting proteins: physiology and pathophysiology. J. Mol. Cell. Cardiol.. 2010;48:2-11.
- [Google Scholar]
- ACC/AHA., 2005. Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. Circulation. 112, e154-e235.
- Beta-blockers use in patients with chronic obstructive pulmonary disease and concomitant cardiovascular conditions. Int. J. Chron. Obstruct. Pulmon. Dis.. 2007;2(4):535-540.
- [Google Scholar]
- Protective effect of n-3 polyunsaturated fatty acids concentrate on isoproterenol induced myocardial infarction in rats. Prostaglandins Leukot. Essent. Fatty Acids.. 2007;76:153-158.
- [Google Scholar]
- The use of a diazonium salt for the determination of glutamic-oxalacetic transaminase in serum. Clin Chim Acta.. 1962;7:199-205.
- [Google Scholar]
- Calcium as mediator of isoproterenol-induced myocardial necrosis. Am. J. Pathol.. 1991;69:459-470.
- [Google Scholar]
- The L-type calcium channel in the heart: the beat goes on. J. Clin. Invest.. 2005;115:3306-3317.
- [Google Scholar]
- Voltage-gated calcium channels. Cold. Spring. Harb. Perspect. Biol.. 2011;3:a003947
- [Google Scholar]
- Investigators and Committees. A randomized trial of beta-blockade in heart failure. The Cardiac Insufficiency Bisoprolol Study (CIBIS) Circulation. 1994;90:1765-1773.
- [Google Scholar]
- Simplified determination of the lipid components of blood serum. Clin. Chem.. 1961;7:37-53.
- [Google Scholar]
- BEST Investigators. A comparative analysis of the results from 4 trials of beta-blocker therapy for heart failure: BEST, CIBIS-II, MERIT-HF, and COPERNICUS. J. Card. Fail.. 2003;9(5):354-363.
- [Google Scholar]
- Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin. Chem.. 1982;28:2077-2080.
- [Google Scholar]
- Drugs for left ventricular remodeling in heart failure. Am. J. Cardiol.. 2005;96:10L-18L.
- [Google Scholar]
- Progressive decline in the ability of calmodulin isolated from aged brain to activate the plasma membrane Ca-ATPase. Biochemistry. 1998;37:9536-9548.
- [Google Scholar]
- The Diagnostic accuracy of three recommended methods for serum aspartate aminotransferase assays in patients suspected of myocardial infarction and hepatobiliary diseases. Clin. Biochem.. 1988;21:323-328.
- [Google Scholar]
- Progress in understanding the LDL receptor and HMG-CoA reductase, two membrane proteins that regulate the plasma cholesterol. J. Lipid. Res.. 1984;25:1450-1461.
- [Google Scholar]
- Effect of KRN 2391, a novel vasodilator, on various experimental anginal models in rats. Jpn. J. Pharmacol.. 1993;63:35-39.
- [Google Scholar]
- Oral contraceptives use and the risk of myocardial infarction: a meta-analysis. Contraception. 2003;68:11-17.
- [Google Scholar]
- Vascular biology of atherosclerosis: overview and state of the art. Am. J. Cardiol.. 2003;91:3A-6A.
- [Google Scholar]
- Colorimetric assays for serum alanine transaminase and lactic dehydrogenase using diazonium zinc salt. Anal. Biochem.. 1966;17:143-153.
- [Google Scholar]
- Phytometric ninhydrin methods for use in the chromatography of amino acids. J. Biol. Chem.. 1948;176:367-388.
- [Google Scholar]
- Effect of α-tocopherol on isoproterenol-induced changes in lipid and lipoprotein profile in rats. Ind. J. Pharmacol.. 1997;29:399-404.
- [Google Scholar]
- Comparative effect of Aegle marmelos extract and alphatocopherol on plasma lipids, lipid peroxides and cardiac marker enzyme levels in rats with isoproterenol-induced myocardial infarction, Singapore. Med. J.. 2005;46:72-78.
- [Google Scholar]
- Rajadurai, M., Stanely Mainzen Prince, P., 2006. Preventive effect of naringin on lipids, lipoproteins and lipid metabolic enzymes in isoproterenolinduced myocardial infarction in Wistar rats. J. Biochem. Mol. Toxicol. 20, 191-197.
- Evaluation of enzymes in pyogenic and tuberculous meningitis. J. Assn. Physicians, India. 2006;54:118-121.
- [Google Scholar]
- Potential oxidative pathways of catecholamines in the formation of lipid peroxides and genesis of heart disease. Adv. Exp. Med. Biol.. 1983;161:391-401.
- [Google Scholar]
- Role of free radicals in catecholamine-induced cardiomyopathy. Can. J. Physiol. Pharmacol.. 1982;60:1390-1397.
- [Google Scholar]
- Plasma creatinine determination. A new and specific Jaffe reaction method. Scand. J. Clin. Lab. Invest.. 1965;17:381-387.
- [Google Scholar]
- Protein oxidation and agedependent alterations in calcium homeostasis. Frontiers. Biosci.. 2000;5:1-23.
- [Google Scholar]
- Repair of oxidized calmodulin by methionine sulfoxide reductase restores ability to activate the plasma membrane Ca-ATPase. Biochemistry. 1999;38:102-112.
- [Google Scholar]
- Protective action of aspirin in experimental myocardial infarction induced by isoproterenol in rats and its effect on lipid peroxidation. Indian. J. Exp. Biol.. 1990;28:480-485.
- [Google Scholar]
- Effect of carnitine on malondialdehyde, taurine and glutathione levels in heart of rats subjected to myocardial stress by isoproterenol. Ind. J. Exp. Biol.. 1989;27:134-137.
- [Google Scholar]
- Determination of glucose by glucose oxide method. Ann. Clin. Biochem.. 1969;6:24-26.
- [Google Scholar]
- Viner, R.I., Ferrington, D.A., Williams, T.D., Bigelow, D.J., Scho¨neich, C., 1999. Protein modification during biological aging: selective tyrosine nitration of the SERCA2a isoform of the sarcoplasmic reticulum Ca 21-ATPase in skeletal muscle. Biochem. J. 340, 657-669.
- Calmodulin’s flexibility allows for promiscuity in its interactionswith target proteins and peptides. Mol. Biotechnol.. 2004;27:33-57.
- [Google Scholar]
- Reactive oxygen species and nitric oxide mediate plasticity of neuronal calcium signaling. Proc. Natl. Acad. Sci. U.S.A.. 2000;97:448-453.
- [Google Scholar]







