Translate this page into:
A study of management and biochemical outcomes in AMI patients supported with different mechanical devices in a single center
⁎Corresponding author at: Zhengzhou University People's Hospital, Department of Cardiology Fuwai Central China, Cardiovascular Hospital, Zhengzhou 450000, People's Republic of China. gaocy6802@163.com (Chuanyu Gao)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Peer review under responsibility of King Saud University.
Abstract
Introduction
Patients with myocardial infarction (MI) and cardiogenic shock (CS) have poor outcomes in terms of morbidity and mortality. Many devices act as a ‘bridge’ in case of cardiogenic shock, by providing circulatory support and buy time so that the patient either recovers or receives a transplant or a long-term device.
Materials and methods
This is a retrospective observational study where all patients (n = 286) getting admitted for MI and CS were included. The different variables are compared across the three groups [extracorporeal membrane oxygenation (ECMO), Intra-aortic balloon pump (IABP) and IABP + ECMO]. The fourth group (Impella) had only 6 patients and no statistical analysis has been done for the same, to avoid skewness of results.
Results
There are a total of 286 patients in the study out of which ECMO was used in 99 patients, IABP in 138 patients, both IABP and ECMO in 43 patients, and Impella in 6 patients. The patients differed in terms of diagnosis category, pre-existing hypertension, pre-existing diabetes, pre-existing hyperlipidemia, pre-existing heart failure, and other co-morbidities. The groups also differed in terms of the cardiac findings like heart rate, left ventricular end-diastolic diameter (LVED), and left ventricular ejection fraction (LVEF). Stents were implanted more commonly among the IABP (22.5%) and IABP + ECMO group (25.6%) as compared to the ECMO group (6.1%), and the difference was statistically significant (p Value = 0.0012). The median time for device usage in ECMO group was 147 h, as compared to 130 h among IABP group and 144 h among IABP + ECMO group, and the difference was statistically significant between the ECMO and IABP group (p Value = 0.047). The median time for breathing machine assisted ventilation was also highest in the ECMO group (262 h), as compared to IABP (86 h) and IABP + ECMO group (177 h). Patients in the ECMO group had the higher heart rate than patients in IABP group (median heart rate: 95 vs 86 beats per minute). Left ventricular ejection fraction was highest in the IABP group (41% in IABP group Vs 24.5% in ECMO group & 35% in IABP + ECMO group).
Conclusion
Though the three groups (IABP, ECMO and ECMO + IABP) were heterogenous, there was a clear advantage in terms of outcomes in the group in which more than one device was used. In conclusion we can say that all three devices have their own advantages and disadvantages, and they have a distinct hemodynamic footprint and thus should be used after detailed assessment of the patient.
Keywords
Mechanical circulatory devices
AMI-CS
Outcomes
Impella
IABP
ECMO
1 Introduction
Cardiogenic shock is the most severe form of heart failure, characterized by inadequate pumping of blood by the left ventricle and signs of peripheral tissue hypoperfusion (Werdan et al., 2014). Myocardial contractile dysfunction leads to the left ventricle being unable to maintain minimum cardiac output of 2.2 L/min, despite of a normal circulatory blood volume. Peripheral tissue hypoperfusion is detected by presence of low urine output, altered mentation and/or cold extremities. Recently, many studies have defined an eligibility criteria of the same as the presence of systolic blood pressure of <90 mm of Hg for more than 30 min or a requirement of catecholamines to maintain systolic blood pressure above 90 mm of Hg, in addition to clinical signs of pulmonary congestion and impaired end-organ perfusion, which is further characterized by the presence of the following criteria: (i) altered mental status; (ii) cold, clammy skin and extremities; (iii) oliguria with urine output < 30 mL/h; or (iv) serum lactate > 2.0 mmol/L (Thiele et al., 2012a) (Fig. 1).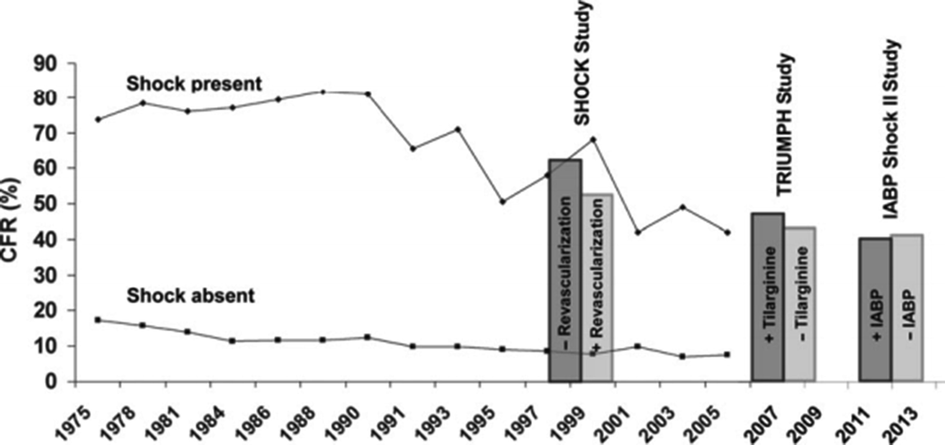
Time trends in hospital case fatality rates (CFR) of patients with acute myocardial infarction (MI), with and without cardiogenic shock. This figure depicts time trends in hospital case fatality rates (CFR) of patients with acute myocardial infarction (MI), with and without cardiogenic shock in the Worcester (MA, USA) metropolitan area. Use of acute interventional reperfusion strategies was popularised following 1990, and there is a clear reduction of mortality of patients suffering from cardiogenic shock, from 70% to less than 50%, following the same. However, as emphasised by the results from the SHOCK study (Shishehbor et al., 2017), the TRIUMPH study (Kolh et al., 2014), and the IABP SHOCK II Trial (Thiele et al., 2012b), the mortality of patients having cardiogenic shock remains unacceptably high at more than 40%. (Figure reproduced from Werdan et al. (2014)).
The mortality of the patients of cardiogenic shock as a complication of acute myocardial infarction (CSMI) is unacceptability high at over 40%, despite of advances in anti-thrombotic medications, cardiac intensive care therapy, and revascularization procedures (Hochman et al., 2006; Thiele et al., 2012b). This high fatality rate has forced the interventional cardiology community across the globe to come up with various mechanical circulatory support devices to improve the outcome of patients with acute MI and cardiogenic shock (Reynolds and Hochman, 2008).
1.1 Mechanical cardiac support devices
Many devices act as a ‘bridge’ in case of cardiogenic shock, by providing circulatory support and buy time so that the patient either recovers or receives a transplant or a long-term device (Thiele et al., 2013). These devices can be used alone or in combination depending upon the type of MI and patient status. Various devices currently available include an intra-aortic balloon pump (IABP), TandemHeart, Impella, extracorporeal membrane oxygenation (ECMO), and CentriMag. Which device to use and whether to use them alone or in combination depends on individual patient needs, local expertise, and anatomic and physiologic considerations. We will focus on Impella, IABP and ECMO in this research paper.
Intra-aortic balloon pump (IABP) was used for mechanical support for decades, but it was downgraded from the guideline recommendations after the IABP-SHOCK II trial failed to show any mortality benefit over medical therapy alone (Meyns et al., 2003; Thiele et al., 2015). Impella (Abiomed, Danvers, Massachusetts, USA) is a promising alternative for percutaneous mechanical circulatory support (pMCS) that has been utilised as a bridge to recovery. It consists of a miniaturised axial flow pump fitted onto a pigtail catheter, pumping blood from the left ventricle into the ascending aorta and providing a cardiac output of 2.5 L/min (Impella 2.5) and up to 4.0 L/min (Impella CP) (Sjauw et al., 2008; Kapur et al., 2013). It actively unloads the left ventricle reducing the stroke-work and myocardial oxygen consumption, thereby providing cardioprotection and robust haemodynamic support (Lamy et al., 1975; Peek et al., 2009; Esposito et al., 2018). ECMO technology originated from cardiopulmonary bypassing (CPB) in 1950 and was mainly used in the pediatric population for the treatment of cardiorespiratory failure. The use of ECMO in adults was infrequent until the publication of CESAR trial, which coincided with the H1N1 epidemic in 2009 (Gaudard et al., 2015). The promising study results and rising incidence of fulminant acute respiratory failure led physicians to consider ECMO as a rescue strategy. Table 1 describes the roles, indications, advantages, and disadvantages of the various MCS devices in detail. AMI: Acute Myocardial Infarction; ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump; MCS: Mechanical Circulatory Support; VA-ECMO: Venoarterial Extracorporeal Membrane Oxygenation; Transcatheter aortic valve replacement (TAVR).
Characteristic
IABP
VA-ECMO
Impella
Role in providing Circulatory support (systemic perfusion)
Low support – if LV is dysfunctional then IABP will not work properly
Good support – increases mean arterial pressure and maintain end-organ perfusion
Good support- increases mean aortic root pressure leading to improvement of systemic perfusion
Role in providing Ventricular support (LV unloading)
Some support - Reduces LV afterload and increases LV cardiac output
Negative role - Increases LV pressure, wall stress and myocardial work, LV afterload
Good support- Reduces both LV pressure and volume
Role in Coronary perfusion
Increases the diastolic pressure in the aortic root and enhances the coronary blood flow
Decreases the heart rate so has some role in reducing the myocardial oxygen demand, can not increase coronary blood flow
Increases the trans-myocardial perfusion gradient (aortic diastolic pressure – LV diastolic pressure), leading to improved coronary perfusion
Role in decongestion
No role
No role
No role
Effect on pulmonary circulation
No significant effect on pulmonary congestion (Coyer et al., 2006)
Decreases the pulmonary artery pressure and places the lungs at an acutely elevated risk for ischemia and pulmonary edema (Chen et al., 2003)
Maintains the lung perfusion
Preferred type of patients
Preserved LVEF, MV-CAD, Patients with Aortic Stenosis, Mitral Regurgitation
Profound hypoxemia, cardiac arrest, sepsis, multi-organ failure
Cardiogenic shock, AMI/Shock, High Risk PCI with Low EF
Role in HF-CS
No large, randomized studies have evaluated the utility of IABP therapy in HF-CS
Some role in refractory cardiogenic shock
Major role in refractory cardiogenic shock (Aso et al., 2016)
Major advantages
Reduces in-hospital events (not mortality) like dialysis, new onset of stroke, pneumonia, sepsis (Mao et al., 2016)
Feasibility of implantation, easy access, cost-effectiveness, can be used in situations of circulatory arrest
Fewer device related complications, less invasive, provide greater hemodynamic support
Major disadvantages
Does not function properly in the presence of an irregular ventricular cardiac rhythm, pulselessness or cardiac resuscitation, and contraindicated in acute severe aortic insufficiency.
Some studies have associated its use with a higher mortality (many patients fail an IABP before they are put on other devices leading to loss of critical time) (Khan and Siddiqui, 2019)Can cause severe side effects including limb ischemia, lower limb amputation, fasciotomy or compartment syndrome, stroke, pulmonary edema, and acute kidney injury (Makdisi and Wang, 2015)
Bleeding complications, cannot be used during valve deployment procedures or when TAVR device has to be placed.
Despite of many MCS devices available for CSMI patients, the data available on comparison of outcomes of the three MCS devices is heterogenous and inconclusive.
We performed this study to further add to the outcome research of MCS devices. To the best of our knowledge, this is the first and only study comparing the outcomes of three MCS devices i.e. IABP, ECMO, Combination of IABP and ECMO, and Impella, in such a huge number of patients in Henan, China. However, it is notable that tandem heart device was not used among the patients, based on the treating surgeon’s discretion.
2 Methods
This study was conducted in a Cardiovascular Hospital, which is a national heart center. This is a retrospective observational study carried out between June 2018 to June 2020, where all patients getting admitted for MI and CS were included in the study. Patients who were too ill to consent or whose relatives did not give consent were excluded from the study. All the variables were recorded in Microsoft excel. Statistical software (SPSS version 22) was used for the statistical analyses. All the variables were tested for normality using Kolmogorov-Smirnov test. The different variables are compared across the three groups (ECMO, IABP and IABP + ECMO). The fourth group (Impella) had only 6 patients and no statistical analysis has been done for the same, to avoid skewness of results. Categorical variables are summarized as frequencies and percentages, while continuous variables as medians and interquartile range (IQR; 25th to 75th percentiles), for the sake of consistency. Univariate association of different categorical variables across the groups was assessed using the chi-square statistic or Fischer exact test. The different continuous variables across the three groups were compared using one-way Analysis of Variance (ANOVA) followed by post hoc Bonferroni test to determine the differences between the two groups. All tests were 2-sided, and p < 0.05 was considered statistically significant. The study was approved by the medical ethics committee of the hospital.
3 Results
There are a total of 286 patients in the study out of which ECMO was used in 99 patients, IABP in 138 patients, both IABP and ECMO in 43 patients, and Impella in 6 patients. The patients differed in terms of diagnosis category (AMI/ respiratory/ other cardiac anomalies/ other indications), pre-existing hypertension, pre-existing diabetes, pre-existing hyperlipidemia, pre-existing heart failure, and other co-morbidities. IABP patients were significantly older than those in ECMO group. The use of various MCS devices was at the discretion of the treating surgeon and we assume that no bias was introduced due to the ongoing study. The median (IQR) age of patients in the four groups were: ECMO group: 51 (34–62) years; IABP group: 64 (56–70) years; IABP + ECMO group: 56 (40–64) years; and Impella group: 77.5 (71.3–80) years. There was a significant difference between the median age of patients between ECMO and IABP (p Value < 0.001; no statistical analysis done for the Impella group). Table 2 describes the demographic and clinical findings among the patients. STEMI: ST-segment–elevation myocardial infarction; AMI: Acute myocardial infarction; ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump; TIA: Transient ischemic attack. ^1 patient had both. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p value
Impella
Gender
Male
63 (63.6%)
93 (67.4%)
30 (69.8%)
0.734
5 (83.3%)
Female
36 (36.4%)
45 (32.6%)
13 (30.2%)
1 (16.7%)
Diagnosis category
AMI + CS
12 (12.1%)
52 (38%)
20 (47.6%)
<0.0001
4 (66.7%)
Respiratory
60 (60.6%)
2 (1.5%)
2 (4.8%)
0 (0%)
Other cardiac abnormalities/ Other indications
27 (27.2%)
83 (60.6%)
20 (47.6%)
2 (33.3%)
AMI type
STEMI
2 (16.7%)
13 (25%)
7 (35%)
0.7389
4 (100%)^
Non-STEMI
2 (16.7%)
8 (15.4%)
4 (20%)
1 (25%)^
Undiagnosed
8 (66.7%)
31 (59.6%)
9 (45%)
0 (0%)
Cardiac arrest before hospital arrival
No
98 (99%)
120 (99.2%)
43 (100%)
0.8113
6 (100%)
Yes
1 (1%)
1 (0.8%)
0 (0%)
0 (0%)
Pre-existing Hypertension
No
72 (72.7%)
77 (55.8%)
35 (81.4%)
0.0016
1 (16.7%)
Yes
27 (27.3%)
61 (44.2%)
8 (18.6%)
5 (83.3%)
Pre-existing Diabetes
No
85 (85.9%)
99 (71.7%)
32 (74.4%)
0.0345
4 (66.7%)
Yes
14 (14.1%)
39 (28.3%)
11 (25.6%)
2 (33.3%)
Pre-existing Hyperlipidemia
No
98 (99%)
117 (84.8%)
41 (95.3%)
0.0004
5 (83.3%)
Yes
1 (1%)
21 (15.2%)
2 (4.7%)
1 (16.7%)
Smoking
No
61 (61.6%)
80 (58%)
24 (55.8%)
0.771
5 (83.3%)
Yes
38 (38.4%)
58 (42%)
19 (44.2%)
1 (16.7%)
Drinking
No
76 (76.8%)
115 (83.3%)
38 (88.4%)
0.2073
4 (66.7%)
Yes
23 (23.2%)
23 (16.7%)
5 (11.6%)
2 (33.3%)
Pre-existing Heart failure
No
99 (100%)
129 (94.2%)
43 (100%)
0.014
5 (83.3%)
Yes
0 (0%)
8 (5.8%)
0 (0%)
1 (16.7%)
History of TIA
No
98 (99%)
136 (99.3%)
43 (100%)
0.8064
6 (100%)
Yes
1 (1%)
1 (0.7%)
0 (0%)
0 (0%)
Taking medicines for co-morbidities
No
73 (73.7%)
80 (58%)
33 (76.7%)
0.012
1 (16.7%)
Yes
26 (26.3%)
58 (42%)
10 (23.3%)
5 (83.3%)
The laboratory and radiological findings have been described in terms of median and inter-quartile range. Hb, platelet count, albumin level, high density lipoprotein (HDL) and low density lipoprotein (LDL) levels were highest in the IABP group and the difference was statistically significant. Creatinine levels and potassium levels were highest in IABP + ECMO group. Majority of the patients in the IABP and IABP + ECMO group (76.1% and 62.8% respectively) had undergone echocardiography as compared to the ECMO group (8.1%) and the difference was statistically significant (p < 0.0001). All the six patients in the Impella group had their echocardiography test done. The groups did not differ significantly in terms of urine protein and resting ECG (p Value = 0.452 & 0.102 respectively). Urine RBC was detected in 49.5% of patients in ECMO group, as compared to those in IABP and IABP + ECMO group (29.7% & 39.5% respectively) and the difference was statistically significant (p Value = 0.0083). It is notable that 50% of patients in the Impella group too had urine RBC detected (no statistical analysis done).
Other laboratory and radiological findings have been given in detail in Table 3. *: significant difference between ECMO and IABP. ^: significant difference between IABP and IABP + ECMO. $: significant difference between ECMO and IABP + ECMO. Hb: Hemoglobin; RBC: Red blood cell; WBC: White blood cell; TG: Triglyceride; TCH: Total cholesterol; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; CK-MB: Creatine kinase-MB; cTNT: Cardiac troponin T; cTNI: Cardiac troponin I; NT-BNP: N-terminal-pro hormone B-type natriuretic peptide; HbA1c: hemoglobin A1c; µ: micro; L: liter; mmol: millimoles; IU: International unit; gm: gram; dl: decilitre; mm3: cubic meter; U: Unit; ng: nanogram; pg: pictogram; mg: milligram; ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump; IQR: Interquartile range. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p values
Impella
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
Hb (mg/dl)*^
96
108.5 (96.25–132)
137
128 (113–140)
42
117 (101–132.75)
<0.001
6
139 (123–142.3)
RBC (106/mm3)*^
96
3.54 (3.1–4.34)
137
4.21 (3.81–4.7)
42
3.65 (3.29–4.43)
<0.001
6
4.22 (4.02–4.61)
WBC (103/mm3)^$
97
9 (5.54–15.2)
137
8.57 (6.27–13.04)
42
11.54 (7.58–18.97)
0.032
6
10.35 (7.12–13.05)
Platelet (103/mm3)*^
96
159.5 (114–226.5)
136
208.5 (162.25–258.75)
42
168.5 (92.75–224.75)
<0.001
6
202.5 (182.75–242.5)
Urine RBC (no.)*^$
54
25.35 (11–100.08)
96
5 (5–92.74)
24
13 (5–376.16)
0.001
Not available
G bilirubin (µ mol/L)
73
11.7 (8–21.1)
95
13.9 (8.3–23.3)
25
15.1 (10.4–28)
0.308
6
10.1 (9.35–14.9)
Albumin (gm/L)*
74
30.35 (26–34.33)
95
38.3 (34.6–41.4)
26
33.8 (29.1–42.58)
<0.001
6
42.2 (38.3–45.35)
TG (mmol/L)
35
1.27 (0.87–1.83)
88
1.27 (0.94–1.72)
21
1.46 (0.77–2.59)
0.835
6
0.99 (0.9–1.39)
TCH (mmol/L)
33
3.52 (2.52–4.36)
88
3.56 (3.02–4.5)
21
2.99 (1.68–4.53)
0.156
6
3.14 (2.77–3.66)
HDL (mmol/L)*^
34
0.79 (0.62–1.12)
88
0.99 (0.82–1.24)
21
0.85 (0.45–1.05)
0.003
6
1.14 (0.98–1.3)
LDL (mmol/L)*^
34
1.82 (1.23–2.42)
88
2.15 (1.72–2.89)
20
1.97 (1.22–2.72)
0.036
6
1.77 (1.51–2.14)
Creatinine (mmol/L)^$
88
0.79 (0.51–1.25)
135
0.79 (0.61–1.24)
39
1.23 (0.69–1.72)
0.005
6
0.82 (0.68–1.17)
Potassium (mmol/L)*$
88
4.13 (3.8–4.7)
137
4.38 (4.05–4.71)
39
4.48 (4.05–5.12)
0.021
6
4.4 (3.95–4.72)
Sodium (mmol/L)*^
89
139 (135–143.5)
137
137 (134–140)
39
139 (133–143)
0.008
6
136.5 (135.25–137.75)
CK-MB (U/L)^$
54
30 (16–72)
65
24 (14.25–85)
25
59 (22.75–244)
0.037
6
39.8 (16.6–94.65)
cTNI (ng/ml)
16
10 (7.99–148.74)
2
76.5 (10–143)
4
1600 (0.01–19550)
0.958
1
634.6 (634.6–634.6)
cTNT (ng/ml)
5
75 (19.78–905.7)
45
63.87 (24.96–528)
5
61.69 (20.22–1920.4)
0.996
2
3484 (1799–5169)
NT-BNP (pg/ml)
11
975 (191–8980)
54
1692 (932.25–3619)
6
900 (182–1856)
0.245
5
1665 (576–3614)
HbA1c (%)
14
6.55 (5.46–8.98)
54
6.31 (5.71–7.42)
13
6.26 (5.51–7.33)
0.946
6
6.05 (5.58–6.81)
The groups also differed in terms of the cardiac findings that have been depicted in Table 4. Patients in the ECMO group had the higher heart rate than patients in IABP group (median heart rate: 95 vs 86 beats per minute). Left atrium measurements, left ventricle end diastolic diameter, systolic BP, and diastolic BP were higher in IABP group as compared to the group in which both IABP and ECMO were used. Left ventricular ejection fraction was highest in the IABP group (41% in IABP group Vs 24.5% in ECMO group & 35% in IABP + ECMO group). *: significant difference between ECMO and IABP. ^: significant difference between IABP and IABP + ECMO. $: significant difference between ECMO and IABP + ECMO. HR: Heart rate; SBP: Systolic Blood pressure; DBP: Diastolic Blood pressure; LA: Left Atrium; LVEDd: Left-ventricular end-diastolic diameter; LVEF: Left ventricular ejection fraction; mm: millimetre; mm Hg: millimetre of mercury; ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p values
Impella
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
HR (baseline; per minute) *
98
95 (80–115.25)
133
86 (75–104.5)
42
91.5 (78.75–105.5)
0.015
6
82 (75.25–89.5)
SBP (baseline; mm Hg)
93
120 (106.5–136)
133
120 (100–135)
41
104 (91.5–126)
0.055
6
124 (120.75–125)
DBP (baseline; mm Hg)
93
71 (62.5–80)
133
72 (63.5–85)
41
68 (55.5–78)
0.145
6
76 (66.5–81.75)
LA (baseline; mm)^
8
36.5 (26.75–39.75)
99
40 (35–45)
27
35 (29–42)
0.005
5
34 (33–43)
LVEDd (baseline; mm)^
8
49.5 (46–55.5)
99
55 (48–63)
27
49 (42–57)
0.022
6
50 (46.75–56.25)
LVEF (baseline; %)*
8
24.5 (17.5–52.5)
104
41 (36–51.75)
27
35 (25–49)
0.02
6
42.5 (38.25–46)
HR (per minute) take out day*$
89
95 (80–116)
127
86 (76–96)
39
81 (74–103)
<0.001
5
70 (68–72)
SBP (mm Hg) take out day^
85
115 (100.5–129.5)
123
120 (105–133)
40
109 (94.25–119.5)
0.003
5
122 (120–127)
DBP (mm Hg) take out day^$
85
69 (59–76)
123
65 (56–72)
40
57 (45–63)
<0.001
5
70 (61–74)
Drug-eluting stents were implanted more commonly among the IABP (22.5%) and IABP + ECMO group (25.6%) as compared to the ECMO group (6.1%), and the difference was statistically significant (p Value = 0.0012). The groups also differed in the number of stents implanted but the difference was not statistically significant (Table 5). ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p value
Impella
Stent implanted
No
93 (93.9%)
107 (77.5%)
32 (74.4%)
0.0012
1 (16.7%)
Yes
6 (6.1%)
31 (22.5%)
11 (25.6%)
5 (83.3%)
No. of stent
1, 2
4 (66.7%)
25 (80.6%)
8 (72.7%)
0.7014
4 (80.0%)
>=3
2 (33.3%)
6 (19.4%)
3 (27.3%)
1 (20.0%)
The median time for device usage in ECMO group was 147 h, as compared to 130 h among IABP group and 144 h among IABP + ECMO group, and the difference was statistically significant between the ECMO and IABP group (p Value = 0.047). The median time for breathing machine assisted ventilation was also highest in the ECMO group (262 h), as compared to IABP (86 h) and IABP + ECMO group (177 h) (Table 6). *: significant difference between ECMO and IABP. ^: significant difference between IABP and IABP + ECMO. $: significant difference between ECMO and IABP + ECMO. ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump; IQR: Interquartile range; PCI: Percutaneous coronary intervention; CABG: Coronary artery bypass graft. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p values
Impella
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
N
Median (IQR)
Device used time (hours)*
99
147 (113–260)
138
130 (66.5–206.25)
43
144 (84–256)
0.047
6
125 (105–175)
Second device used time (hours)
–
–
–
–
41
140 (119–227.5)
NA
–
–
PCI/CABG taking time (minutes)
6
80 (38.75–315)
59
80 (50–120)
19
65 (35–100)
0.738
5
120 (100–130)
Breathing machine assisted ventilation (hours)
94
262.75 (128.88–374.12)
106
86 (34–186.98)
38
177 (64.75–340.42)
<0.001
1
180 (180–180)
Urgent CABG PCI procedures were carried out more frequently in the IABP and IABP + ECMO groups (42% and 44.2% respectively), as compared to the ECMO group (4%), and the difference was statistically significant. Breathing machine assisted ventilation was most commonly used in the ECMO group (94.9%) as compared to the IABP (76.8%) and IABP + ECMO group (88.4%). Temporary pacemakers were most commonly needed in the IABP group (28.3%), as compared to the ECMO (1%) and IABP + ECMO group (7%), and the difference was statistically significant (p Value < 0.0001). Table 7 includes the details of the complications that occurred among the various groups and their comparison. ECMO: Extracorporeal membrane oxygenation; IABP: Intra-aortic balloon pump; PCI: Percutaneous coronary intervention; CABG: Coronary artery bypass graft; CRRT: Continuous renal replacement therapy. Since impella group had only 6 patients, no statistical analysis was conducted for that group.
Variables
ECMO
IABP
IABP + ECMO
p value
Impella
Urgent CABG PCI procedure
No
95 (96%)
80 (58%)
24 (55.8%)
<0.0001
6 (100%)
Yes
4 (4%)
58 (42%)
19 (44.2%)
0 (0%)
Breathing machine assisted ventilation
No
5 (5.1%)
32 (23.2%)
5 (11.6%)
0.0005
5 (83.3%)
Yes
94 (94.9%)
106 (76.8%)
38 (88.4%)
1 (16.7%)
Type of assisted ventilation
Invasive
73 (77.7%)
12 (11.3%)
14 (36.8%)
<0.0001
1 (100%)
Non-invasive
21 (22.3%)
94 (88.7%)
24 (63.2%)
0 (0%)
CRRT replace treating
No
98 (99%)
134 (97.1%)
37 (86%)
0.0009
6 (100%)
Yes
1 (1%)
4 (2.9%)
6 (14%)
0 (0%)
Temporary pacemaker
No
98 (99%)
99 (71.7%)
40 (93%)
<0.0001
6 (100%)
Yes
1 (1%)
39 (28.3%)
3 (7%)
0 (0%)
Mortality in hospital
No
94 (94.9%)
131 (94.9%)
42 (97.7%)
0.7348
5 (83.3%)
Yes
5 (5.1%)
7 (5.1%)
1 (2.3%)
1 (16.7%)
Cause of death
Brain death
0 (0%)
0 (0%)
1 (100%)
0.0131
0 (0%)
Cardiac death
0 (0%)
3 (42.9%)
0 (0%)
1 (100%)
Multiple organ failure/ Other reasons of death
5 (100%)
4 (57.2%)
0 (0%)
0 (0%)
4 Discussion
Despite of many MCS devices available for CSMI patients, the data on their outcome is scant. What seems evident that the mortality of MI patients with cardiogenic shock has reduced over the years but is still unacceptably high.
The above literature suggests that the data available on comparison of outcomes of the three MCS devices is heterogenous and inconclusive. We performed this study to further add to the outcome research of MCS devices. To the best of our knowledge, this is the first and only study comparing the outcomes of three MCS devices i.e., IABP, ECMO, Combination of IABP and ECMO, and Impella, in single center, national heart center experience of Henan, China.
It is noteworthy that the four groups were heterogenous and differed from each other in terms of patient severity and pre-existing co-morbid conditions. Thus, direct comparison of the outcomes of the groups, in terms of morbidity and mortality, should be done with caution. The fourth group, having six Impella patients was not included in statistical analysis as it would have skewed the data even more.
The IABP group had highest proportion of patients having pre-morbid conditions like hypertension, diabetes, hyperlipidemia, and a history of heart failure, and the difference was significant when compared to ECMO and ECMO + IABP groups. Five out of six patients in Impella group also had pre-existing hypertension, diabetes, and hyperlipidemia. Interestingly, the blood parameters were worse in the ECMO group (like Hb level, Platelets level, Serum albumin and HDL), as compared to the IABP and ECMO + IABP group. As far as the cardiac findings are concerned, the patients in the IABP group had a lower heart rate, higher left atrium size and left ventricular end diastolic diameter as compared to the ECMO and ECMO + IABP group, and the difference was statistically significant. The left ventricular ejection fraction was highest in IABP and Impella group. Almost one-fourth of the patients in the IABP and ECMO + IABP groups and five out of six patients in the Impella group had undergone implantation of stents.
The MCS device was used for the least amount of time in the IABP and Impella group, and longer among the ECMO and ECMO + IABP groups. The time of breathing machine assisted ventilation was also higher in the ECMO group. An urgent CABG PCI procedure was carried out in most of the patients in IABP and ECMO + IABP groups, as compared to those in ECMO and Impella group.
Mortality rate lowest in the group where both ECMO and IABP devices were used, however, there was no statistical significance in mortality between the groups. In the Impella group, one out of six patients suffered from a cardiac death. The reason of death of the patient from ECMO + IABP group was brain death, while three patients in IABP suffered from a cardiac death, one from multi-organ failure and three from other reasons. In the ECMO group one patient died from multi-organ failure and four patients died from other reasons. Other studies have also reported similar baseline mortality risk among the patients in which different MCS devices are used like: Impella and IABP (Mao et al., 2016); Imeplla, Tandem heart and IABP (Patel et al., 2014); and IABP and ICP heart pump (Thiele et al., 2017). However, a RCT was conducted comparing outcomes in patients undergoing non-emergent high risk PCI receiving IMPELLA RECOVER LP 2.5 System Versus Intra Aortic Balloon Pump (IABP), and the study reported that the outcomes in terms of major adverse events (MAE) and major adverse cardiac and cerebral events (MACCE [death, stroke, myocardial infarction, and repeat revascularization]) were better in the Impella arm as compared to the IABP arm (MAE, 37% vs 49%, p [0.014 respectively]; MACCE, 22% vs 31%, p [0.034 respectively]) (Sabra et al., 2020). However, there was no difference in mortality in the two arms. Similarly, another retrospective, two-centre study comparing mortality among Impella CP/5.0 or ECMO support groups concluded that though mortality was similar in the two groups, the patients on Impella support had significantly fewer device-related complications (Karami et al., 2020).
A study done on inpatients that underwent percutaneous coronary intervention (PCI) and non-elective Impella or ECMO placement for AMI-CS between 2015 and 2017 in USA reported that the ECMO cohort had a significantly higher in-hospital mortality and the Impella group was associated with better clinical outcomes (Lemor et al., 2020). A study by Grajeda et al also suggests that Impella can be used as an unloading strategy in patients on VA-ECMO and the simultaneous use of them in a category of patients decreased mortality (Grajeda Silvestri et al., 2020). Another study reported similar findings (Cheng et al., 2013).
It is noteworthy that Impella was most frequently used CMS device in our setting as majority of the patients were candidates for high risk-PCI/CABG procedures and many patients also had cardiogenic shock. Application of IABP is instrumental in curbing mortality among complicated AMI patients, and facilities using a higher number of IABPs report lower mortality among patients as compared to facilities which do not use IABPs (Chen et al., 2003; Coyer et al., 2006). In our study, patients requiring a longer cardiovascular support were put on ECMO and the maximum number of deaths amongst our study population was amongst this group. However, the difference was not statistically significant. Least number of deaths were in the group receiving support both from IABP and ECMO. Another study involving 1,650 cardiogenic shock adult patients compared in-hospital mortality among IABP/VA-ECMO-group (n = 604) and the VA-ECMO-alone-group (n = 1,064) and it was noted that in-hospital mortality were significantly lower in the IABP/VA-ECMO-group than in the VA-ECMO-alone-group (Aso et al., 2016).
The biochemical outcomes such as serum levels of NT-pro-Btype Natriuretic Peptide (NT-BNP), CK-MB, and troponin of the patients were varied but outside normal limits. When evaluated in ACS, serum concentrations of BNP and NT-proBNP have a graded relationship with risk for short- and long-term mortality (Omland et al., 2002; Morrow et al., 2003). Regarding the other biochemical assays, the total CK level is insensitive and a nonspecific test to be used to diagnose AMI, however CK-MB mass assay is highly specific, and an abnormal value (particularly when it exceeds 5% of the total CK value) at any time in a patient with chest pain is highly suggestive of AMI (Gupta, 2009). Cardiac troponin levels (troponin-T and troponin-I) have a greater sensitivity and specificity than CK-MB levels in detecting MI. Positive troponin levels are considered virtually diagnostic of MI, as they are without equal in combined specificity and sensitivity in this diagnosis (Gupta, 2009).
The current study has many limitations like its retrospective nature with short follow up restricted us from following the patients and observe clinical outcomes over a long period of time. The clinical outcomes assessed were also very limited. The fourth group in which Impella was used was too small to be included in statistical analysis. However, despite of these limitations this is a novel study done in Henan that sheds light on outcomes amongst patients of AMI in which various mechanical devices have been used. Though the other three groups (IABP, ECMO and ECMO + IABP) were heterogenous, there was a clear advantage in terms of outcomes in the group in which more than one device was used. In conclusion we can say that all three devices have their own advantages and disadvantages, and they have a distinct hemodynamic footprint and thus should be used after detailed assessment of the patient. A multi-centric study with longer follow up is needed to get more robust and generalizable results.
Conflicts of interest/competing interests
Authors declare that no conflict of interest exists.
Ethics approval
The study was approved by the medical ethics committee of Fuwai Central China Cardiovascular Hospital.
Consent to participate
All authors consent to participate in this manuscript.
Consent for publication
All authors consent to publish this manuscript in Journal of King Saud University-Science.
Availability of data and material
Data will be available on request to corresponding or first author.
Code availability
Not Applicable.
Author contributions
RAB, SM, SMA, AR,WX, YZ, and CG drafted the experimental design and performed the experiments. HXF and CG helped in data collection, data analysis and initial draft of manuscript text. All authors read the manuscript before communication.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
We would like to thank our professors, colleagues and data collection personnel.
References
- The effect of intraaortic balloon pumping under venoarterial extracorporeal membrane oxygenation on mortality of cardiogenic patients: an analysis using a nationwide inpatient database. Crit. Care Med.. 2016;44:1974-1979.
- [Google Scholar]
- Relation between hospital intra-aortic balloon counterpulsation volume and mortality in acute myocardial infarction complicated by cardiogenic shock. Circulation. 2003;108:951-957.
- [Google Scholar]
- Impella to unload the left ventricle during peripheral extracorporeal membrane oxygenation. ASAIO J.. 2013;59:533-536.
- [Google Scholar]
- Australasian trends in intra-aortic balloon counterpulsation weaning: results of a postal survey. Crit. Care Resuscitation. 2006;8
- [Google Scholar]
- Left ventricular unloading before reperfusion promotes functional recovery after acute myocardial infarction. J. Am. Coll. Cardiol.. 2018;72:501-514.
- [Google Scholar]
- Management and outcome of patients supported with Impella 5.0 for refractory cardiogenic shock. Crit. Care. 2015;19:1-12.
- [Google Scholar]
- Impella to unload the left ventricle in patients undergoing venoarterial extracorporeal membrane oxygenation for cardiogenic shock: a systematic review and meta-analysis. J. Card. Surg.. 2020;35:1237-1242.
- [Google Scholar]
- Laboratory approach to the management of clinical emergencies: a diagnostic series. J. Lab. Phys.. 2009;1:027-030.
- [Google Scholar]
- Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511-2515.
- [Google Scholar]
- Mechanically unloading the left ventricle before coronary reperfusion reduces left ventricular wall stress and myocardial infarct size. Circulation. 2013;128:328-336.
- [Google Scholar]
- Mechanical circulatory support in cardiogenic shock from acute myocardial infarction: Impella CP/5.0 versus ECMO. Eur. Heart J.: Acute Cardiovascular Care. 2020;9:164-172.
- [Google Scholar]
- Intra-Aortic Balloon Pump. Treasure Island (FL): StatPearls Publishing; 2019.
- Effects of extracorporeal membrane oxygenation (ECMO) on pulmonary hemodynamics, gas exchange and prognose. Trans.-Am. Soc. Arti. Internal Organs. 1975;21:188-198.
- [Google Scholar]
- Impella versus extracorporeal membrane oxygenation for acute myocardial infarction cardiogenic shock. Cardiovasc. Revascularization Med.. 2020;21:1465-1471.
- [Google Scholar]
- Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J. Thoracic Dis.. 2015;7:E166.
- [Google Scholar]
- Benefits of intraaortic balloon support for myocardial infarction patients in severe cardiogenic shock undergoing coronary revascularization. PLoS ONE. 2016;11:e0160070
- [Google Scholar]
- Left ventricular support by Catheter-Mountedaxial flow pump reduces infarct size. J. Am. Coll. Cardiol.. 2003;41:1087-1095.
- [Google Scholar]
- Evaluation of B-type natriuretic peptide for risk assessment in unstable angina/non–ST-elevation myocardial infarction: B-type natriuretic peptide and prognosis in TACTICS-TIMI 18. J. Am. Coll. Cardiol.. 2003;41:1264-1272.
- [Google Scholar]
- Prognostic value of N-terminal pro-atrial and pro-brain natriuretic peptide in patients with acute coronary syndromes. Am. J. Cardiol.. 2002;89:463-465.
- [Google Scholar]
- Temporal trends in the use of intraaortic balloon pump associated with percutaneous coronary intervention in the United States, 1998–2008. Am. Heart J.. 2014;168(363–373):e312
- [Google Scholar]
- Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351-1363.
- [Google Scholar]
- Cardiogenic shock: current concepts and improving outcomes. Circulation. 2008;117:686-697.
- [Google Scholar]
- The postoperative use of Impella as a ventricular assist device in high-risk patients undergoing coronary artery bypass surgery: a case series and comparison. J. Card. Surg.. 2020;35:113-117.
- [Google Scholar]
- Left ventricular unloading in acute ST-segment elevation myocardial infarction patients is safe and feasible and provides acute and sustained left ventricular recovery. J. Am. Coll. Cardiol.. 2008;51:1044-1046.
- [Google Scholar]
- Percutaneous short-term active mechanical support devices in cardiogenic shock: a systematic review and collaborative meta-analysis of randomized trials. Eur. Heart J.. 2017;38:3523-3531.
- [Google Scholar]
- Intraaortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock: design and rationale of the Intraaortic Balloon Pump in Cardiogenic Shock II (IABP-SHOCK II) trial. Am. Heart J.. 2012;163:938-945.
- [Google Scholar]
- Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013;382:1638-1645.
- [Google Scholar]
- Intraaortic balloon support for myocardial infarction with cardiogenic shock. N. Engl. J. Med.. 2012;367:1287-1296.
- [Google Scholar]
- Mechanical circulatory support in cardiogenic shock. Eur. Heart J.. 2014;35:156-167.
- [Google Scholar]







