Translate this page into:
Assessment of sunscreen effects in photosensitivity under UV exposure during COVID-19 pandemic
⁎Corresponding authors at: Department of Pharmacy, COMSATS University Islamabad, Abbottabd 22060, Pakistan (A. Ali). Department of Environmental Sciences, COMSATS University Islamabad, Abbottabd 22060, Pakistan (A. M. Abbasi). atifali@cuiatd.edu.pk (Atif Ali), amabbasi@cuiatd.edu.pk (Arshad Mehmood Abbasi)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The aim of this work was to assess the effects of typical and optimal use of sunscreens in photosensitivity under UV exposure during the COVID-19 pandemic. First, a cross-sectional study was conducted among 384 participants to find out about photosensitivity in COVID-19 pandemic using a validated questionnaire involving demographic characteristics and Fitzpatrick skin type to measure skin phototypes that also included information about skin reactions upon sun exposure, the incidence of photosensitivity, and photoprotection behaviour. It was further extended by finding photosensitivity among 200 medical staff and patients that were recovered from COVID-19 infection. Next, the study involved 22 participants in two groups: optimal use with 2 mg per cm2 sunscreen and typical use for 7 days. The sunscreen used was an SPF 50+ product with various ingredients. Instrumental measurements were taken at baseline and 7th day visits to quantify skin melanin and erythema values. 54.9 % of participants had a history of photosensitivity, skin redness after sun exposure (38.0 %), skin protection (74.2 %), always using sunscreen (21.1 %), and applying sunscreen twice a day (12.2 %). A significant association between age, photoprotection behaviour, and photosensitivity was found. The incidence rate of photosensitivity in the population was 90/1000. 63.5 % of the participants agreed to specific skin related manifestations of COVID-19; preventive measures for COVID-19 infection made their skin sensitive (65 %); enhanced photosensitivity of the skin after taking preventive measures (53.5 %); use of hand sanitizers made their skin sensitive (63.5 %); and use of sunscreens was helpful in treating photosensitivity (58.5 %). In addition, there was a decrease in skin melanin and erythema values with optimal use of sunscreen and an increase in skin melanin and erythema values with typical use of sunscreen. When the paired sample t test was applied, the result was found to be significant. It was determined that the COVID-19 pandemic had a high incidence of photosensitivity. Skin sensitivity was increased by using hand sanitizers. Additionally, it is important to prioritise using sunscreen optimally to avoid skin photosensitization. More work on large numbers of participants of different populations in various regions is required in the direction of population guidance.
Keywords
COVID-19 pandemic
Photosensitivity
Sunscreen
Public health
1 Introduction
Coronavirus disease 2019, or COVID-19, caused by SARS-CoV-2, became a serious public health issue, and later became a global pandemic. Since severe inflammation and increased proinflammatory cytokines in serum levels cause acute respiratory distress syndrome (ARDS), multiorgan failure, etc. (Hatami et al., 2022; Kutlu, 2020). The ultraviolet radiation from the sun produces health problems such as photosensitivity, sunburn, premature aging, and consequently skin cancer. Photosensitivity is an exaggerated response of the skin to ultraviolet (UV) radiation from the sun. When an exogenous or endogenous chromophore activated by ultraviolet radiation, including UVA and UVB lights, absorbs into the skin, it produces photosensitivity (Oakley and Badri, 2021). Photosensitivity is seen in both males and females of all ages. Genetic and environmental influences may interfere with the prevalence of photosensitivity (Oakley & Badri, 2019). The prevalence of photosensitivity across Europe is 10–20 % of the population. Excessive contact with UV rays also leads to skin cancer (Kim & Chong, 2013). A study in the UK showed that 86 % of skin cancers are induced by exposure to UV radiation from the sun. In the last decade, it is expected that new cases of melanoma will rise by 47 % (Parkin et al., 2011).
The campaigns for social acceptability of masks have the possible effects of reducing and preventing photosensitive disorders, photo-aging, and skin cancer (Doyon et al., 2022). Furthermore, how distancing between individuals, the imposition of masks, and stay-at-home have correlated with UV exposure and COVID-19 remains questionable. Sunscreens are an important aspect of photoprotection (Sambandan and Ratner, 2011; Waldman and Grant-Kels, 2019). However, reduced public access to sunscreen is another problem (Szeto et al., 2022). Their efficacy in reducing photo-carcinogenesis and photo-aging is well accepted (Sambandan and Ratner, 2011).
Dermatologists can encourage greater awareness about sun protection for everyday outdoor experiences, indoors, and during colder months, regardless of COVID-19–induced changes and mask-wearing. Skin appearance-based education shows promise in promoting sunscreen use (Tuong and Armstrong, 2014). IMPACT Melanoma’s touch-free automated sunscreen dispensers and extensive virtual or online outreach programs will be advantageous (Pollack et al., 2011; Szeto et al., 2022). Skin melanin is the first line of protection against UV. Melanin absorbs UV radiation and scatters this radiation as heat. Melanin production is regulated by melanocytes, which are found in the skin. Melanin that accumulates in keratinocytes acts as a natural sunscreen that protects the skin from harmful UV radiation (Radiations and Mechanism, 2017). Skin erythema is the reddening of the skin because of external stimuli, one of which is sun exposure. Skin erythema is a sign of dermatological diseases such as acne, psoriasis, melasma, post-inflammatory and hyperpigmentation. No research has yet investigated the use of sunscreens under UV exposure in the COVID-19 situation. Hence, we assessed the effects of typical and optimal use of sunscreens on skin melanin and erythema in photosensitivity under UV exposure during the COVID-19 pandemic.
2 Methodology
2.1 Study setting and data collection
This study was conducted in Abbottabad, Khyber Pakhtunkhwa, which is in the northwestern part of Pakistan's Khyber Pakhtunkhwa (KP) region, at a height of 1256 m above sea level. It has an area of 1967 square kilometers. The region's elevation ranges from 600 to 2800 m as shown in Fig. 1 (Waseem et al., 2021).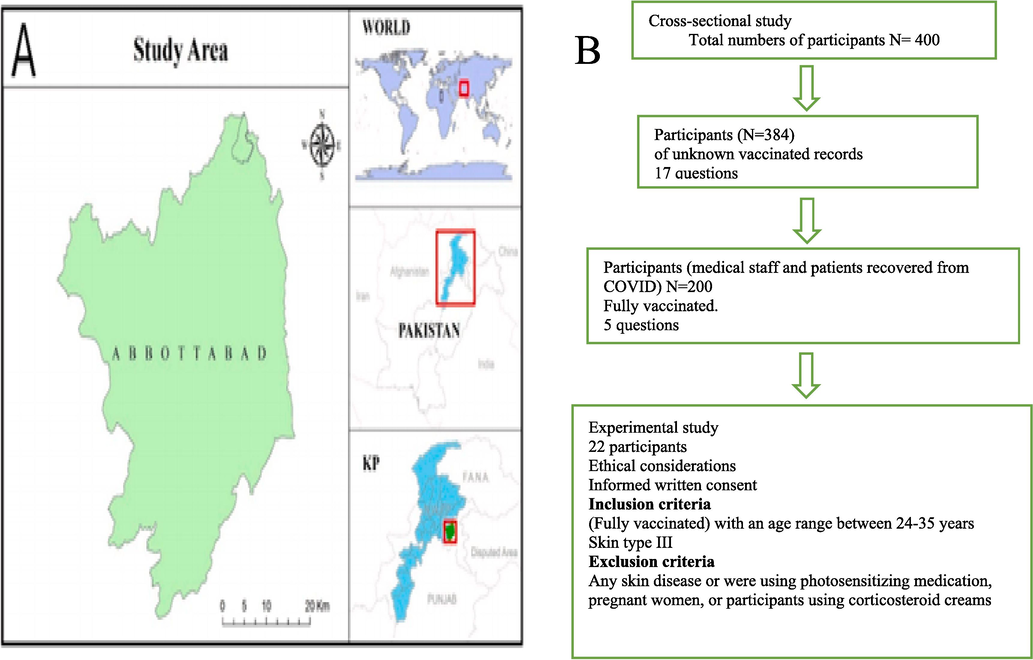
(A) Abbottabad map (B) study flow diagram.
2.1.1 Sampling technique and sample size
A random sampling technique was used for the collection of data from mid - November 2020 to mid - March 2021.The sample size was calculated using the Rao-soft sample size calculator. According to the Pakistan Bureau of Statistics, the total population in Abbottabad in 2017 was 1,332,912 (Census of Pakistan, 2017). For the calculation of sample size, a 95 % confidence interval and a 5 % margin of error were selected. The calculated sample size was 384 unknown vaccination records included in the first phase of the study. A validated questionnaire of 17 questions was randomly handed over to the participants. Participants were then, explained the facts and the nature of the study. The filled-out questionnaires were collected. In the second phase, 200 participants with known vaccinated records (medical staff and patients) recovered from COVID-19 infection were included. Again, a questionnaire of five questions was handed to the second phase of participants, incompletely filled questionnaires were removed and replaced with those of other participants. This cross-sectional study was divided into five parts. (1) Demographic characteristics, (2) Fitzpatrick skin type to measure skin phototypes that also included information about skin reactions upon sun exposure, (3) incidence of photosensitivity, (4) photo-protection behaviour and (5) photosensitivity in medical staff and patients recovering from COVID-19 infection. The study was conducted on the questions, which were statistically evaluated using Cronbach’s alpha for reliability and consistency. The value of Cronbach’s alpha came to be 0.67, which indicated an acceptable level of reliability for the questionnaire (Foering et al., 2013).
2.2 Evaluating the effects of sunscreen use on skin melanin and erythema contents
2.2.1 Ethical consideration
This study was approved by COMSATS University Islamabad Registrar Secretariat Academic Unit (PS) (Letter No. 334/21/371) and conducted according to the international guidelines of the Helsinki Declaration (Ali et al., 2019). All ethical considerations were followed before the start of the study. Participants were informed about the study and clearly guaranteed that their data could be used only for public health dissemination. The participants had given written consent. They were given the choice to leave the study before signing the consent. No incentive was given to any participant.
2.2.2 The inclusion and exclusion criteria
22 participants (fully vaccinated) with an age range between 24 and 35 years and skin type III screened from Fitzpatrick skin types were included to assess the effects of sunscreen use on skin melanin and erythema contents. Participants who had any skin disease or were using photosensitizing medication, pregnant women, or participants using corticosteroid creams were excluded from the study.
2.2.3 Amended Draize patch testing
Before the evaluation of the effects of sunscreen on skin melanin and skin erythema, an amended Draize patch test was accomplished on both the left and right arms of each participant for skin safety. The patch for the left and right forearms was soaked with sunscreen. After 24 h, any skin irritation was examined visually by an experienced dermatologist. The responses were graded as non-irritating (0–2), slightly irritating (02–4.0), average irritating (4.0–6.0), and highly irritating (6.0–8.0) (Gebrehiwot et al., 2015).
2.2.4 Measurement of skin melanin and erythema
Participants were divided into two groups (11 each) based on the experimental study. The guidelines were the application of 2 mg per cm2 of sunscreens on the forearms tagged as optimal use, and self-applied use of sunscreen on the forearms, tagged as typical use of sunscreens. One group represented optimal use, and the other represented typical use of sunscreen for 7 days. The sunscreen used in this study was the marketed product with SPF 50+ claiming octyl methoxy cinnamate, benzophenone, avobenzone, zinc oxide, cetostearyl alcohol, tocopherol, EDTA, sodium benzoate, butyl hydroxy anisol glyceryl monostearate, pola wax, xanthan gum, emulsifying wax, tween 60, tween 80, and aqua. The instrumental measurements were performed at baseline and on the 7th day of visits to quantify the skin melanin and erythema values using a sophisticated noninvasive probe attached to the multi-skin test center (Courage and Kazaka, Germany).
2.3 Statistical analysis
To summarize and analyze the data, Microsoft Excel 365 was used. The questions were classified on ordinal and nominal scales. The significant difference was determined by Pearson Chi-Square using IBM SPSS version 23.0. A paired sample t-test was performed to find the significant difference between baseline and day 7 visits. The level of significance was set at p < 0.05.
3 Results and discussion
An exaggerated response to ultraviolet (UV) radiation from the sun results in various skin problems, including photosensitivity. Optimal use of sunscreen is crucial to avoid photosensitivity, even after COVID recovery (Narbutt et al., 2019).
3.1 Demographic characteristics
400 questionnaires were distributed for the study, resulting in a response rate of 96 %. 384 participants within the age range of 18 to 50 years of both genders were included, of whom 71.35 % were aged between 18 and 28 years., 23.55 % were aged between 29 and 39 yrs. and 4.16 % were aged 40–50 years, 33.07 % were males, while 66.92 % were females. Among them 38.55 % were married, and 61.45 % were unmarried. 49.47 % of the participants were employed, and 50.52 % were unemployed (Table 1). Photosensitivity was observed in both males and females of all ages.
Variables
N (%)
Age
(18–28)
274 (71.35)
(29–39)
92 (23.95)
(40–50)
16 (4.16)
Gender
Male
127 (33.07)
Female
257 (66.92)
Marital status
Married
148(38.55)
Unmarried
236 (61.45)
Employment Status
Employed
190 (49.47)
Unemployed
194 (50.52)
3.2 Fitzpatrick (FST) skin types
Scores of the frequency distribution for Fitzpatrick skin types among the population of Abbottabad are represented in Table 2 while graphically, it is explained in Fig. 3A. The Fitzpatrick skin classification is commonly used to estimate photo-damage and skin cancer risk (Sharma et al., 2018). According to our study, most of the participants had dark brown eyes, and i.e., 34.9 %, while 31.0 % of the participants had brownish-black eyes. 25.8 % of the participants had hazel or light brown eyes, 5.2 % of the participants had light blue, light gray or light green eyes. 3.1 % of the participants had blue, gray, or green eyes. 46.9 % of the participants had dark brown natural hair color, 43.8 % had black hair color, and 7.6 % had blonde hair, whereas 1.8 % of the participants had red or light blonde hair, while no participants had dark blonde or light brown hair color. 30.5 % of participants had fair to beige skin color, 26.6 % had fair to pale skin, 24.5 % had olive or light brown skin, and 10.2 % of participants had ivory white as their natural skin shade, whereas 8.3 % of participants were dark brown or black skinned. 51.0 % of participants had no freckles on a sun-exposed area of skin, 20.1 % had very few freckles, 17.2 % had a few freckles and 7.8 % had several freckles whereas 3.9 % had many freckles, on the sun-exposed area of skin. 32.0 % showed burns rarely due to sun exposure, 29.7 % showed never burns due to the sun, 25.5 % showed burns moderately, 6.3 % showed often burns, blisters, and peels due to the sun, whereas 4.2 % showed always burns, blisters, and peels due to sun exposure. 31.0 % showed a tan; sometimes burns cause the skin tan, 28.1 % was never burned or tanned, 19.8 % showed it was burned or caused tanning, 14.8 % showed often burned and tanned whereas 6.3 % showed always burn and caused tanning. 38.3 % of participants had experienced a light skin tan, 26 % had experienced mere or no skin tanning, 25.0 % of participants experienced moderate skin tan, 7.6 % experienced deep skin tan, whereas 3.1 % had natural dark coloured skin. 47.1 % of the participants had face sensitivity towards the sun, among which 27.3 % had normal face sensitivity, 10.9 % had very sensitive face skin, 9.9 % were resistant to or never had any problem with sun exposure, and 3.1 % had resistance to sun exposure.
Score
0
N%
1
N%
2
N%
3
N%
4
N%
Light blue/light-grey/Light green
12 (3.1)
Blue/Grey/Green
20 (5.2)
Hazel/Light Brown
99 (25.8)
Dark brown
134 (34.9)
Brownish black
119 (31.0)
Hair color?
Red or light blonde
7 (1.8)
Dark brown/Light brown
0 (0)
Blonde
29 (7.6)
Dark brown
180 (46.9)
Black
168 (43.8)
Skin Color?
Ivory white
39 (10.2)
Fair or pale
102 (26.2)
Fair to beige
117 (30.5)
Olive or light brown
94 (24.5)
Dark brown/black
32 (8.3)
How many Freckles upon sun exposure?
Many
15 (3.9)
Several
30 (7.8)
A few
66 (17.2)
Very few
77 (20.1)
None
196 (51)
How does your skin respond to the sun?
Always burn, blister and peel
16 (4.2)
Often burn, blister and peel
33 (8.6)
Burn moderately
98 (25.5)
Burn rarely
123 (32)
Never burn
114 (29.7)
Does your skin tan?
Always burn
24 (6.3)
Seldom burn
108 (28.1)
Sometimes burn
119 (31.0)
Often burn
57 (14.8)
Never burn
108 (28.1)
How deeply do you tan?
Not at all/very little
100 (26)
Lightly tan
147 (38.3)
Moderately tan
96 (25.0)
Deeply tan
29 (2.6)
Skin naturally dark
12 (3.1)
How sensitive is your face to the sun?
Very sensitive
42 (10.9)
Sensitive
181 (47.1)
Normal
105 (27.3)
Resistant
18 (4.7)
Very resistant
42 (10.9)
The FST scale may also be used to assess how various skin types respond to popular cosmetic/dermatological treatments, making it a helpful tool in cosmetic dermatology. 58.6 % of participants had skin type III, 29.4 % had type IV, and 9.1 % had type II. According to the study, 47.1 % of participants had sensitive face areas to the sun. Sun damage, photoaging, and the risk of melanoma and non-melanoma skin malignancies are higher in skin types I-III (Sachdeva, 2009).
3.3 The presence of photosensitivity
The presence of photosensitivity in the population of Abbottabad is represented in Table 3. UV and visible light are the most common sources of photosensitivity. This energy is absorbed by chromophores (molecules found in the skin) to cause biological reactions such as photosensitivity (Lankerani and Baron, 2004). This study showed that 54.1 % of the participants had a history of photosensitivity, whereas 44.1 % had no history of photosensitivity. 43.5 % of the participants didn’t experience photosensitivity; 27.9 % experienced it last month, 18.2 % of the participants experienced photosensitivity some days ago; and 10.4 % of the participants experienced it regularly. 38.0 % of the participants experienced skin redness after sun exposure, 28.4 % experienced other issues related to skin after sun exposure, 19.3 % experienced sun burns, and 14.1 % experienced itchiness. 74.2 % of participants protect their skin, whereas 25.8 % of participants do not protect their skin. 71.6 % of the participants did not have any lesions in the sun-exposed area, whereas 28.4 % of participants had lesions in sun-exposed areas.
Photosensitivity
N
%
History of photosensitivity
No
169
44.1
Yes
215
54.9
Last experience photosensitivity
Regularly
41
10.4
Didn’t experience
169
43.5
Last month
107
27.9
Some days ago,
71
18.2
Effects after sun exposure
Others
109
28.4
Itchiness
54
14.1
Skin redness
146
38.0
Sunburn
74
19.3
Skin protection
No
99
25.8
Yes
285
74.2
Lesion on the sun exposed area
No
275
71.6
Yes
109
28.4
3.4 Photoprotection behaviour
Photoprotection behaviour found in the population of Abbottabad is represented in Table 4. The use of sunscreen products has increased as the incidence of photo-damaging effects induced by UV radiation has increased (Serpone et al., 2007). From the data obtained, it was detected that most of the participants used sunscreen for their skin protection, with 38.0 % using sunscreen sometimes when they were exposed to the sun, 24.5 % never using sunscreen, and 21.1 % always using sunscreen when they were exposed to the sun, whereas 16.4 % usually use sunscreen when they are exposed to the sun. 40.4 % of participants were using SPF 30+, 24.2 % of participants were using SPF 50+, and 23.9 % were using SPF 30, whereas 11.6 % were using SPF 20. Most of the participants applied sunscreen before going out, i.e., 27.3 %. 20.4 % of participants applied once a day, 14.3 % applied sunscreen rarely, and 12.2 % applied sunscreen twice a day. 32.2 % of participants did not use sunscreen because they did not remember to use it. 25.8 % of participants thought that they did not get any sunburns, and 20.1 % of participants had other reasons for not using sunscreen, 9.4 % of participants felt uncomfortable while using sunscreen. 8.1 % of participants did not use sunscreen because it is expensive, whereas 4.2 % did not use sunscreen because it causes skin allergies.
Photo-rotection precautions
N
%
Sunscreen use
Always
81
21.1
Never
99
24.5
Sometimes
144
38.0
Usually
62
16.4
Use of SPF grades
SPF-20
33
11.6
SPF-30
68
23.9
SPF-30+
115
40.4
SPF-50+
69
24.2
The applications of sunscreen
Before going out
105
27.3
Don’t use
99
25.8
Once a day
78
20.4
Rarely use
55
14.3
Twice a day
47
12.2
Reason of don’t use sunscreen
Cause skin allergy
16
4.2
Don't get sunburn
99
25.8
Don't remember to use
125
32.6
Expensive
31
8.1
Others
77
20.1
Uncomfortable to use
36
9.4
3.5 Photosensitivity cases (2020–2021)
The association between gender and photosensitivity is represented in Fig. 2A. After the application of the chi square test, it was found to be insignificant. The association between age categories and photosensitivity is represented in Fig. 2B. After the application of the chi square test, it was found to be significant, i.e., P < 0.001. The association between marital status and photosensitivity is represented in Fig. 2C. After application of the chi square test, it was found to be insignificant, i.e., p = 0.3. The association between sun protection and photosensitivity is represented in Fig. 2D. After the application of the chi square test, it was found to be significant. The observed cases, risk ratio, and incidence of photosensitivity among different age categories are represented in Table 5. The age, categories, and incidence of photosensitivity, Abbottabad in 2021 are represented in Fig. 3B. The association between photoprotection behaviour and photosensitivity is represented in Table 6. After application of the chi square test, it was found to be significant.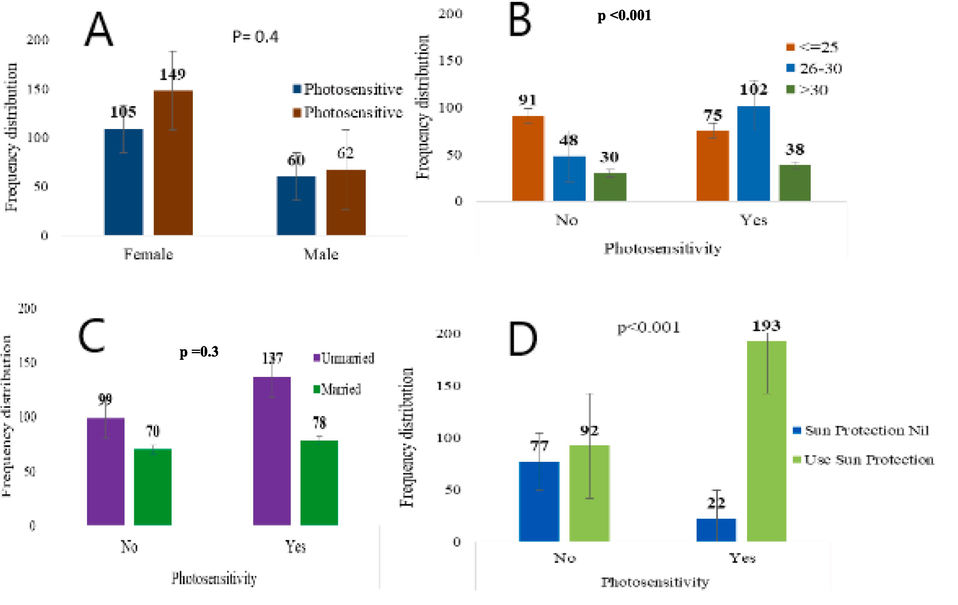
(A). Association between gender and photosensitivity. (B). Association between age categories and photosensitivity. (C). Association between marital status and photosensitivity. (D). Association between sun protection and photosensitivity.
Observed cases
Risk Ratio
Incidence/1000
Male
<25
15
0.33
90
25–30
31
0.51
207
>30
9
0.43
132
Female
<25
80
0.66
482
25–30
63
0.71
420
>30
17
0.36
250
Participants
<25
95
0.99
572
25–30
94
1.22
627
>30
26
0.79
382
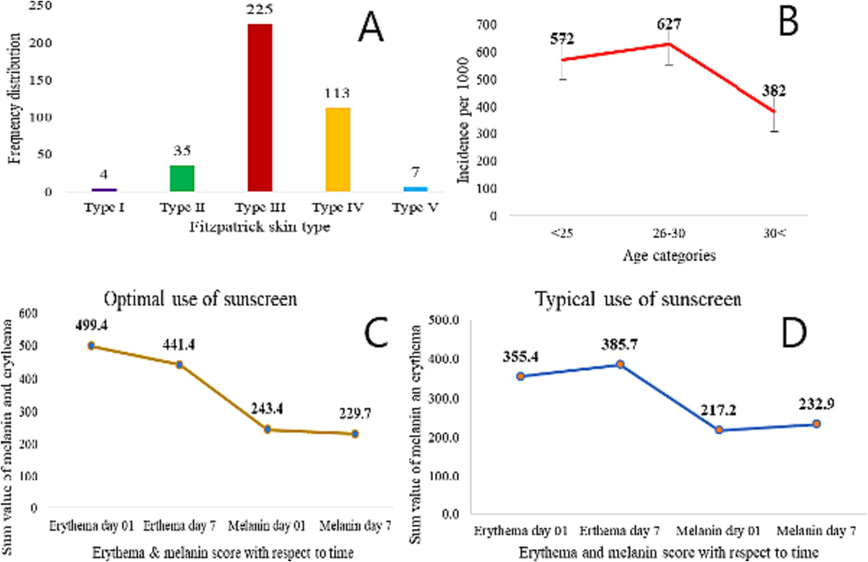
(A). Frequency distribution of Fitzpatrick skin types among the population of Abbottabad (N = 384) (B). Age categories and Incidence rate 20–21. (C). Skin erythema and melanin contents with optimal use (N = 22) (D). Skin erythema and melanin contents with typical use (N = 22).
Photo-protection precaution
Photosensitivity
No
Yes
p-value
n (%)
n (%)
Sunscreen use
Always
27 (16)
54 (25.1)
<0.001
Sometimes
49 (29)
97 (45.1)
Usually
15 (8.9)
48 (22.3)
SPF grade
SPF-20
18 (10.7)
15 (7)
<0.001
SPF-30
27 (16)
41 (19.1)
SPF-30+
34 (20.1)
95 (44.2)
SPF-50+
18 (10.7)
51 (23.7)
The application of sunscreen
Before going out
37 (21.9)
78 (36.3)
<0.001
Once a day
33 (19.5)
51 (23.7)
Rarely use
30 (17.8)
25 (11.6)
Twice a day
5 (3)
48 (22.3)
3.6 The incidence
Photosensitivity is seen in both males and females of all ages. Genetic and environmental influences may interfere with the prevalence of photosensitivity (Oakley and Badri, 2019). The prevalence of photosensitivity across Europe is 10–20 % of the population. Excessive contact with UV rays also leads to skin cancer (Kim and Chong, 2013). A study in the UK showed that 86 % of skin cancers are induced by exposure to UV radiation coming from the sun (Parkin et al., 2011).
Self-reported photosensitivity refers to any skin-specific or systemic unpleasant responses that a person has in response to sun exposure over a period (Foering et al., 2012). Excessive exposure to UV radiation without protection plays an important role in photosensitivity (Narbutt et al., 2019). Table 5 showed that among males, there were 15 observed cases of photosensitivity under the 25-year age group with a risk ratio of 0.33, and the incidence rate of photosensitivity was 90/1000 of the population. There were 31 observed cases under the age category 25–30 with a risk ratio of 0.51, and the incidence rate of photosensitivity was 207/1000. In the above 30 age categories, there were 9 observed cases with a risk ratio of 0.43. The incidence rate of photosensitivity was 132/1000. Among females, there were 80 observed cases with a risk ratio of 0.66 under age 25. The incidence rate was 482/1000. Between the age groups 25–30, there were 63 observed cases of photosensitivity, with a risk ratio of 0.71 showing an incidence rate of 420/1000. Whereas, at an age above 30, there were 17 observed cases with a risk ratio of 0.36. The incidence rate was 250/1000. At an age below 25, observed cases were 95, a risk ratio of 0.99, and the incidence rate was 572/1000. Between age group 25–30, total observed cases were 94 a risk ratio of 1.22. The incidence rate was 627/1000. In the total population, above the age of 30, the observed cases of photosensitivity were 26, a risk ratio of 0.79. The incidence rate was 382/1000.
3.7 Photoprotection in medical staff and patients that were recovered from COVID-19 infection (N = 200)
Our study was able to provide a comprehensive overview of the photosensitivity among COVID-19 recovered participants, although it also had limitations. Sunlight aids in the healing of a variety of illnesses, including respiratory infections such as influenza and severe acute respiratory syndrome (Cory and Kling, 2018; Geier et al., 2018). Longer periods of sunlight exposure are linked to greater incidences of COVID-19 recovery among patients because sunlight increases vitamin D production, which boosts the immune system (Asyary and Veruswati, 2020; Ventenilla et al., 2018). The data was collected from the medical staff and the patients that recovered from COVID-19 infection. Table 7 shows that 63.5 % of the participants agreed to specific skin related manifestations of COVID-19, and 36.5 % did not agree. 65 % of the participants agreed that preventive measures for COVID-19 infection made their skin sensitive, whereas 35 % did not agree. 53.5 % of the participants showed enhanced photosensitivity of the skin after taking preventive measures, while 46.5 % showed no response. 63.5 % of participants agreed that the use of hand sanitizers made their skin sensitive while 36.4 % did not agree. 58.5 % of participants agreed that the use of sunscreens was helpful in treating photosensitivity, whereas 41.5 % of participants did not agree.
Photoprotection in medical staff and patients that were recovered from COVID infection
N (%)
Does specific skin-related manifestation (indication) of COVID-19 exist?
No
73 (36.5 %)
Yes
127 (63.5 %)
Do preventive measures of COVID-19 make their skin sensitive?
No
70 (35 %)
Yes
130 (65 %)
What is the response of skin to sun exposure after taking preventive measures?
No response
93 (46.5 %)
Enhance photosensitivity
107 (53.5 %)
Does the excessive use of hand sanitizer make skin sensitive to the sun?
No
73 (36.5 %)
Yes
127 (63.6 %)
Does the use of sunscreens effective in treating photosensitivity?
No
83 (41.5 %)
Yes
117 (58.5 %)
3.8 The effects on skin melanin and erythema
Fig. 3C and D represents effects on skin melanin and erythema contents with optimal and typical use of sunscreens with respect to time. There was a decrease in skin melanin and erythema values with optimal use of sunscreen SPF 50+ and an increase in skin melanin and erythema values with typical use of sunscreen SPF 50+ with time. After the application of the paired sample t-test, there was a significant difference between them. Many people are unaware of the optimal use of sunscreen and guidelines (Narbutt et al., 2019). Sunscreen application by consumers is frequently insufficient for ultraviolet radiation protection according to the advertised sun protection factor (SPF). Although sunscreen SPFs are labelled based on testing at a 2 mg/cm2 application density, actual protection is generally much lower due to consumer application densities ranging from 0.5 to 1 mg/cm2 (Li et al., 2019).
4 Limitations
The data collection was difficult due to the Corona virus pandemic in the region so some demographic characteristics such as impact of income, occupation, the residence (rural or urban) on the use of sunscreen were the limitations of study.
5 Conclusion
Our investigation found that the COVID-19 pandemic had a significant rate of photosensitivity. The most effective application of sunscreen and photosensitivity are related. As opposed to the typical application of sunscreen that does not provide photoprotection, the sunscreen inhibits photosensitivity when applied at 2 mg per cm2 on the sun-exposed areas. Therefore, when used properly, sunscreens are successful in treating photosensitivity.
Acknowledgment
The authors extend their appreciation to the Researchers Supporting Project number (RSP2023R418), King Saud University, Riyadh, Saudi Arabia. We would like to extend our gratitude to Higher Education Commission of Pakistan (HEC) for providing equipment facility to conduct this work under project No. 7741/Federal/NRPU/R&D/HEC/2017 and thankful to Head and Chairman, Department of pharmacy, COMSATS University Islamabad, Abbottabad, Pakistan.
Authorship contribution
SM did formal analysis, investigation, validation, and wrote original draft, AA involve in conceptualization, project administration, methodology, resources, supervision, validation, visualization, writing - review & editing, HMS involve in formal analysis, resources, RMA provided financial assistance, involve in review and editing, ANA provided financial assistance, involve in review and editing, HK did review & editing, formal analysis, AMA involve in review, editing, conceptualization, financial assistance, validation, visualization. MN involves revision, editing, setting and review.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Anti-pollution cosmetic-based one-step formation of w/o/w multiple emulsion containing D-biotin for skin protection: fabrication and in vitro and in vivo evaluation. Drug Deliv. Transl. Res.. 2019;9:1117-1132.
- [CrossRef] [Google Scholar]
- Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource center is hosted on Elsevier Connect, the company’s public news and information. Sci. Total Environ. Journey 2020
- [Google Scholar]
- Interactions between sunlight and microorganisms influence dissolved organic matter degradation along the aquatic continuum. Limnol. Oceanogr. Lett.. 2018;3:102-116.
- [CrossRef] [Google Scholar]
- An added benefit of masks during the COVID-19 pandemic: Ultraviolet protection. J. Cutan. Med. Surg.. 2022;26:63-70.
- [CrossRef] [Google Scholar]
- Prevalence of self-report photosensitivity in cutaneous lupus erythematosus. J. Am. Acad. Dermatol.. 2012;66:220-228.
- [CrossRef] [Google Scholar]
- Characterization of clinical photosensitivity in cutaneous lupus erythematosus. J. Am. Acad. Dermatol.. 2013;69:205-213.
- [CrossRef] [Google Scholar]
- Evaluation of the wound healing property of Commiphora guidottii Chiov. ex. Guid. BMC Complement. Altern. Med.. 2015;15:1-11.
- [CrossRef] [Google Scholar]
- A longitudinal ecological study of seasonal influenza deaths in relation to climate conditions in the United States from 1999 through 2011. Infect. Ecol. Epidemiol.. 2018;8
- [CrossRef] [Google Scholar]
- Serious health threat of mucormycosis during the ongoing COVID-19 pandemic: what dermatologists need to know in this regard. Int. J. Dermatol. 2022:1-3.
- [CrossRef] [Google Scholar]
- Photosensitivity in cutaneous lupus erythematosus. Photodermatol. Photoimmunol. Photomed.. 2013;29:4-11.
- [CrossRef] [Google Scholar]
- Analysis of dermatologic conditions in Turkey and Italy by using Google Trends analysis in the era of the COVID-19 pandemic. Dermatol. Ther.. 2020;33:1-6.
- [CrossRef] [Google Scholar]
- Photosensitivity to exogenous agents. J. Cutan. Med. Surg.. 2004;8:424-431.
- [CrossRef] [Google Scholar]
- Sunscreen application, safety, and sun protection: the evidence. J. Cutan. Med. Surg.. 2019;23:357-369.
- [CrossRef] [Google Scholar]
- Sunscreen applied at ≥ 2 mg cm −2 during a sunny holiday prevents erythema, a biomarker of ultraviolet radiation-induced DNA damage and suppression of acquired immunity. Br. J. Dermatol.. 2019;180:604-614.
- [CrossRef] [Google Scholar]
- Photosensitivity. Treasure Island (FL): StatPearls Publishing; 2019.
- Photosensitivity. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
- [Google Scholar]
- Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br. J. Cancer. 2011;105:S66-S69.
- [CrossRef] [Google Scholar]
- Melanoma survival in the United States, 1992 to 2005. J. Am. Acad. Dermatol.. 2011;65:S78.e1-S78.e10.
- [CrossRef] [Google Scholar]
- Ultraviolet radiations: Skin defense-damage mechanism. Adv. Exp. Med. Biol.. 2017;2017(996):71-87.
- [CrossRef] [Google Scholar]
- Fitzpatrick skin typing: Applications in dermatology. Indian J. Dermatol. Venereol. Leprol.. 2009;75:93-96.
- [CrossRef] [Google Scholar]
- Sunscreens: An overview and update. J. Am. Acad. Dermatol.. 2011;64:748-758.
- [CrossRef] [Google Scholar]
- Inorganic and organic UV filters: Their role and efficacy in sunscreens and suncare products. Inorg. Chim. Acta. 2007;360:794-802.
- [CrossRef] [Google Scholar]
- Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin. Exp. Dermatol.. 2018;43:274-280.
- [CrossRef] [Google Scholar]
- An analysis of public sunscreen distribution in the United States during the COVID-19 pandemic. J. Am. Acad. Dermatol.. 2022;86:e241-e243.
- [CrossRef] [Google Scholar]
- Effect of appearance-based education compared with health-based education on sunscreen use and knowledge: A randomized controlled trial. J. Am. Acad. Dermatol.. 2014;70:665-669.
- [CrossRef] [Google Scholar]
- Psychosocial aspects associated with use of sunscreen, natural sunlight exposure, and artificial tanning. Wien. Med. Wochenschr.. 2018;168:236-242.
- [CrossRef] [Google Scholar]
- The role of sunscreen in the prevention of cutaneous melanoma and nonmelanoma skin cancer. J. Am. Acad. Dermatol.. 2019;80:574-576.e1.
- [CrossRef] [Google Scholar]
- Influence of urban sprawl on microclimate of abbottabad, pakistan. Land (Basel). 2021;10:1-22.
- [CrossRef] [Google Scholar]







