A meta-analysis of cohort and pilot studies indicates association of mouthwash use and risk of hypertension in adults
⁎Corresponding authors at: Department of Biotechnology, School of Bio Sciences and Technology (SBST), Vellore Institute of Technology (VIT), Vellore 632014, India (F. Ahmad). Research and Scientific Studies Unit, College of Nursing and Allied Health Sciences, Jazan University, Jazan-45142, Saudi Arabia (S. Haque). faraz.ahmad@vit.ac.in (Faraz Ahmad), shhaque@jazanu.edu.sa (Shafiul Haque)
-
Received: ,
Accepted: ,
This article was originally published by Elsevier and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The relationship between high blood pressure (hypertension) incidence and mouthwash use is a subject of ongoing research. Origin of this link may lie in mouthwash-mediated destruction of oral microflora, and consequently reduced nitric oxide (NO) bioavailability. In this study, we evaluated the association between mouthwash use and the risk of hypertension through statistical meta-analysis of published cohort and cross-sectional studies. The search strategy and selection of research articles was in accord with PRISMA guidelines, and under pre-defined set of inclusion criteria. Primary research studies focused on “association among use of mouthwash and risk of hypertension incidence” were searched on databases such as PubMed, EMBASE, MEDLINE, and Cochrane Library. MesH keywords such as “hypertension”, “mouthwash use”, “risk of HTN”, “HTN incidence”, “nitric oxide bioavailability”, and “cohort studies” were used. Out of 1650 studies, 9 met all the inclusion criteria and were finally selected. RevMan 5.3 software was employed for statistical analyses of data retrieved from these selected studies. About 6384 adults with mild hypertension symptoms were included in this meta-analysis from different cohort, pilot and cross-sectional studies. All participants’ ages ranged between 40 and 60 years with mild symptoms of hypertension. While high statistical heterogeneity was observed, our results indicate a significant association of antiseptic mouthwash use with the risk of developing hypertension. The findings reveal a slightly but significantly elevated risk of development of hypertension among regular antiseptic mouthwash users, in comparison to non-users. However, further studies are needed to confirm and establish this relationship further.
Keywords
Mouthwash
Hypertension
Nitric oxide
Microflora
Meta-analysis
1 Introduction
Hypertension, more commonly known as high blood pressure, is reported as a highly prevalent non-communicable disease, affecting 45.5 % of the adult population and causing approximately 7.7 million premature deaths worldwide (Forouzanfar et al., 2017). About one billion adult individuals are affected by hypertension globally. It is a leading risk factor for multiple conditions, including cardiovascular disease (CVD), diabetes and stroke (Kearney et al., 2005). It is estimated that about 45 % of cardiovascular-linked and 51 % of stroke-linked mortalities occur due to elevated blood pressure (Williams et al., 2018). Due to adverse consequences, hypertension has been increasingly becoming a tremendous burden for the global healthcare system for the last few decades (Wake, 2021). Incidence of high blood pressure may be triggered by different risk factors. These may be associated with lifestyle and poor compliance to treatment, such as high-salt diet (Lim et al., 2012), alcohol consumption (Mills et al., 2016), smoking (Rust and Ekmekcioglu, 2017), and lack of exercise (Chakraborty et al., 2018). Identifying associated risk factors and suggesting preventive measures can play an important role in public health by managing incidence rates of hypertension (Landsberg et al., 2013; Narkiewicz, 2006; Seravalle and Grassi, 2017).
Optimally functioning oral microbiota aids in the transformation of dietary nitrate into nitric oxide (NO), a signaling molecule which is critical for vascular functions and maintenance of blood pressure levels. Indeed, NO bioavailability is thought to be modulated systemically by oral microbes expressing nitrate reductase which converts nitrate to nitrite which triggers NO signaling (Woessner et al., 2016). NO released by endothelial cells is essential for maintaining the structural integrity and homeostasis of the vascular system (McDonagh et al., 2015).
Most commonly used mouthwashes contain bacteriocides, fluoride and chlorhexidine (OʼBrien et al., 2002). During the past few years, it has been proposed that using antiseptic mouthwash daily eliminates the salivary nitrate- and nitrite-metabolizing bacteria (Haraszthy and Sreenivasan, 2017; Marya et al., 2017; Vlachojannis et al., 2016). Frequent mouthwash may reduce oral bacteria, leading to low NO bioavailability and absorption (Govoni et al., 2008). Decreased NO production may result in immediate loss of a vasodilator, resulting in elevations in blood pressure (Bondonno et al., 2015). Disruptions of NO signaling may subsequently alter cellular mechanisms of inflammation and oxidative stress, both of which play major pathogenic roles for inducing hypertension-associated conditions, including CVDs (Siti et al., 2015).
According to survey reports in 2017, about 203 million Americans used dental rinses (containing fluoride) once a day, while 17 million used it twice a day (Statista Research Department, 2022a). In the United States, 36 % of the population used mouthwash daily, and over two-thirds used it to treat oral problems or diseases (Statista Research Department, 2022b). The statistics of hypertension incidence showed that two out of three hypertensive patients had been involved in mouth rinsing with mouthwash. It indirectly affects their medication, which is used to manage hypertension (Centers for Disease Control and Prevention, 2023). Moreover, various epidemiological studies found a strong association between antiseptic mouthwash and cardiovascular disease (risk linked directly with long-term hypertension) (Centers for Disease Control and Prevention, 2023). Individuals who use mouthwash with antiseptics daily may have an elevated chance of acquiring hypertension and pre-diabetes/diabetes than those who use mouthwash less frequently or never (Joshipura et al., 2020, 2017). The findings of various such studies have indicated that mouthwash usage have short-term effects on the incidence of hypertension (Govoni et al., 2008; Hezel and Weitzberg, 2015). In this systematic review and meta-analysis, we statistically evaluate the evidences for the association between mouthwash use and hypertension incidence risk using data retrieved from previously published cohort and pilot studies.
2 Materials & methods
Our study was conducted following the guidelines of preferred reporting items for systematic review and meta-analyses (PRISMA) statement (Page et al., 2021).
2.1 Search strategy & study selection
The research papers related to “association among use of mouthwash and risk of hypertension incidence” were searched on scholarly databases such as PubMed, EMBASE, MEDLINE, and Cochrane library. Searches were conducted using MesH keywords such as “hypertension”, “mouthwash use”, “risk of HTN”, “HTN incidence” “nitric oxide bioavailability” and “cohort studies”. Only those research articles were extracted which were based on cohort and pilot studies of HTN population through above mentioned electronic databases. We extracted the studies published up to 2023 for authentic data selection.
2.2 Data extraction
The information collected from the systematically retrieved articles included first author names, study aims and sample, year of publication, type of methodology, and primary outcomes and findings. We designed the PICO model for characterization of the above mentioned research aims for further selection of the retrieved articles. The PICO question comprised of four parts, including population (P), intervention (I), comparison (C) among experimental and control groups and outcome (O) (Cumpston et al., 2021).
The PICO question for our study were as follows:
P—Adult population (40 to 60 years).
I—Use of mouthwash (risk factor).
C—Mouthwash users versus non mouthwash users.
O—Outcomes (hypertension incidence).
2.3 Inclusion criteria
Predefined inclusion criteria were used for screening of research articles after search and extraction (Field and Gillett, 2010). We included only those studies in our meta-analysis which met following criteria:
-
The studies involving adult population with mild hypertension and used medication for management at least once in their lifetime.
-
The studies were cohort, epidemiological, pilot and short clinical trial-based studies.
-
Only those studies were included in which only use of mouthwash was discussed as risk of hypertension rather than toothpaste.
-
The outcomes of included studies were hypertension and linked diseases such as cardiovascular issues as well as stroke.
-
Only primary studies which were published in English between 2010 till 2023 were included.
2.4 Outcomes assessed
Our primary outcome was the short-term risk of hypertension due to mouth rinsing with fluoride-containing mouthwash among adults. Among included cohort studies, most adults already had hypertensive symptoms. Hypertension is defined as a condition in which systolic blood pressure (SBP) prevails ≥ 140 mm of Hg, and diastolic blood pressure (DBP) ≥ 90 mm of Hg, and patients have been using medication to control or manage this issue (Williams et al., 2018). In this meta-analysis, we aimed to appraise the short-term effects of mouthwash use on the risk of hypertension incidence and management by medication among adult population.
2.5 Quality assessment
Two reviewers evaluated the quality of included studies independently by using the risk bias tool of Cochrane Collaboration of RevMan software version 5.3. In events of any disagreements, a third arbitrator was called upon for reconcilement with discussion.
2.6 Statistical analysis
RevMan 5.3 software was employed for statistical analyses of data extracted from the retrieved primary studies. While there are other comparable softwares (Wang and Leeflang, 2019), RevMan 5.3 is user friendly and simplifies the processes of study selection, data extraction, risk of bias assessment, and calculations involved in meta-analyses. Further, the output is also detailed and easy to comprehend. A p-value < 0.05 was considered statistically significant, results were presented as odds ratio (ORs) with a 95 % confidence interval (CI). Moreover, heterogeneity assessment was done via the Q test and I2 statistics. A fixed-effects model and a random-effects model were applied in case no significant difference was detected from the heterogeneity test.
3 Results
3.1 Included studies
The research articles were selected and screened for recent meta-analysis according to research aims and PRISMA guidelines. About 1650 research articles were searched from the above-mentioned electronic databases. Only 100 research articles were found eligible for screening after quality assessment. Of those, 9 studies met the preset inclusion criteria and were analyzed for final results, as mentioned in Fig. 1 and Table 1.
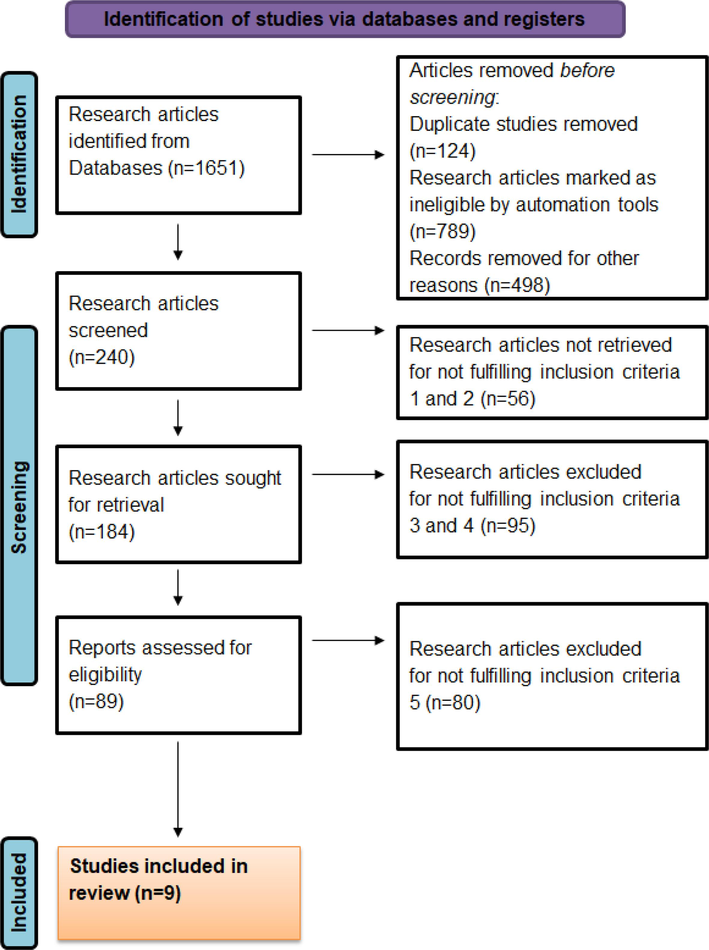
- PRISMA flow chart of screening and selection of studies.
| First Author | Year of publication | Sample size | Study Aims | Type of methodology | Primary outcomes | Findings | Citation |
|---|---|---|---|---|---|---|---|
| Muñoz Aguilera, Eva | 2021 | 250 with periodontitis & 250 control individuals | To investigate association among periodontitis | Nested Case Control study | Mean difference in systolic blood pressure = 3.36 mm of Hg & diastolic pressure = 2.16 mm of Hg | Periodontitis (decreased oral micro flora) is linked to higher systolic blood pressure | (Muñoz Aguilera et al., 2021) |
| Janket, Kaumudi | 2023 | 256 patients with CVD and 250 control | To investigate association among mouth rinsing and hypertension which causes CVD | Longitudinal study | Hazard ratio of mouthwash use on CVD mortality HR = 0.49 [0.27–0.87] | The advantages that result from mouthwash use did not demonstrate any long-term negative or positive impact on CVD mortality. | (Janket et al., 2023) |
| Joshipura, Kaumudi | 2019 | 540 participants in experimental group; 241 in control | To investigate relationship among mouthwash use and hypertension | Longitudinal Study | About 66 out of 540 developed hypertension after twice use of mouthwash in a day | Utilization of over-the-counter mouthwash frequently was linked to a higher probability of hypertension | (Joshipura et al., 2020) |
| Bondonno, Catherine P. | 2015 | 11 patients with hypertension, others 4 in control | To evaluate effect of antibacterial mouthwash use on NO metabolism and blood pressure | Short clinical trial | Mean difference in systolic blood pressure = 2.3 mm of Hg | Use of mouthwash is associated with high blood pressure through disruption of NO pathway | (Bondonno et al., 2015) |
| Del Pinto, Rita | 2022 | 4506 participants | To assess the association oral hygiene habits (flossing, mouthwash use and toothbrush) with hypertension | Cross sectional Survey | Mean difference in systolic pressure is 6.80 mm of Hg and in diastolic pressure is 2.98 mm of Hg | Manual tooth brushing and other means of oral hygiene means (such as tooth brushing) lead to hypertension rather than electric tooth brushing | (Del Pinto et al., 2022) |
| Kapil, Vikas | 2013 | 19 healthy individuals in experimental group & control group | To evaluate suppression of oral microflora by mouthwash use which lead to hypertension | Cross sectional study | Mean difference in systolic and diastolic among experimental and control group = 2–3.5 mm of Hg | The 7 day follow up of mouthwash use increased systolic and diastolic blood pressure due to low circulating NO concentration | (Kapil et al., 2013) |
| Petersson, Joel | 2009 | 20 individuals in experimental group & 15 in control group | To investigate the effect of microflora and dietary nitrites on blood pressure through use of mouthwash | Cross sectional study | Mean difference in systolic and diastolic among experimental and control group = 5–7.5 mm of Hg | The biological activity of nutritional nitrate may be decreased by frequent use of antiseptic mouthwashes, raising blood pressure | (Petersson et al., 2009) |
| McDonagh, S.T.J. | 2015 | 12 healthy volunteers | To investigate the effect of strong and weak antiseptic agents on plasma nitrate levels | Cross sectional study | Mean difference in systolic blood pressure = 3.45 mm of Hg & diastolic pressure = 2.65 mm of Hg | High blood pressure results from the suppression of the rise in plasma [NO2] by both potent and ineffective antibacterial drugs. | (McDonagh et al., 2015) |
| Shaw, Karrol Anne | 2019 | 10 healthy volunteers | To assess the effects of sodium intake and antiseptic mouthwash use on blood pressure | Randomized controlled & cross over trial | Mean difference in systolic blood pressure = 4.87 mm of Hg & diastolic pressure = 3.34 mm of Hg | Use of mouth wash and sodium intake are strongly associated with hypertension | (Shaw, 2019) |
3.2 Study characteristics
About 6384 adults with mild hypertension symptoms were included in recent meta-analysis from different cohort, pilot and cross-sectional studies. All participants' ages ranged from 40 to 60 years.
3.3 Risk bias
The risk bias plot of the included studies was obtained from Cochrane library of Review manager. Figs. 2 and 3 depict the risk bias summary and graph, respectively.
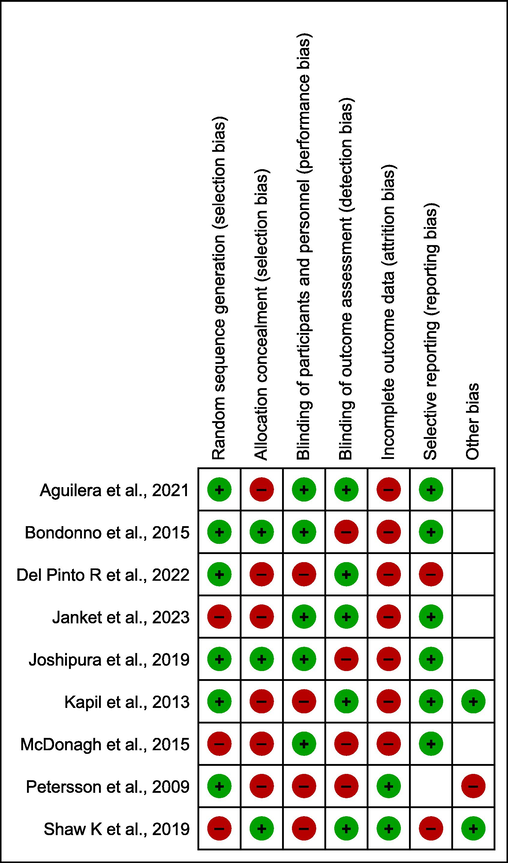
- Risk bias summary of included studies.
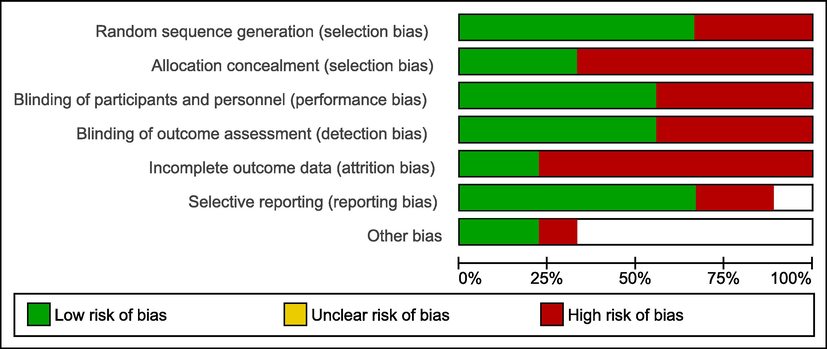
- Risk bias graph of included studies.
3.4 Risk of hypertension with mouthwash use
6 out of 9 studies were included in the pooled analysis, while the other 3 studies could not get the statistical significance to be included in recent meta-analysis. Overall, the pooled estimate showed that mouthwash use significantly triggered the risk of hypertension (Fig. 4) with a relative risk ratio of 1.41 (95 % CI 1.13–6.72; p-value < 0.001), and statistical heterogeneity was observed (Z = 10.14; I2 = 97 %).
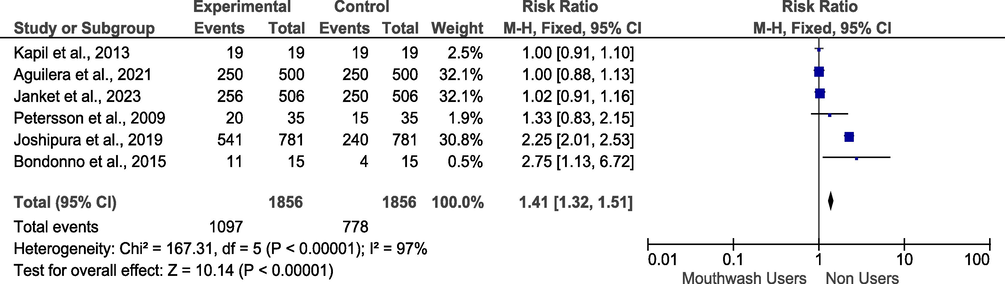
- Risk ratio of hypertension among mouthwash users or non-users.
3.5 Mean difference of SBP
The mean difference in SBP among mouthwash users and non-users was evaluated from the mean difference (Fig. 5). A pooled analysis of 8 included studies among experimental and control groups showed increased SBP with a hazard ratio of 1.53 [95 % CI 1.52–1.54] among mouthwash users.
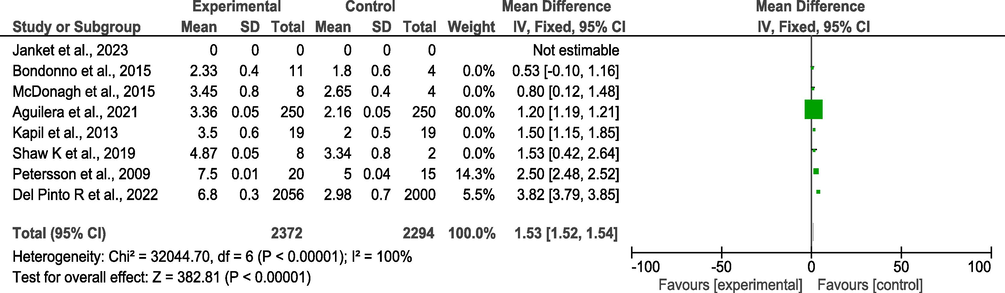
- Mean difference of systolic blood pressure in experimental and control group.
4 Discussion
Mouthwash is recommended for benefits against gum disease, halitosis, or dental cavities; nevertheless, medications are only good for a limited time. Contrarily, mouthwash is often utilized over a lengthy period of time and promoted as a component of daily dental hygiene. Based on evidence of positive benefits and limited toxicity, the American Dental Association (ADA) has approved certain mouthwash for regular use. Nevertheless, most analyses of advantages and safety have focused on short-term outcomes. Joshipura et al. (2020) reported that the use of non-recommended mouthwash among physician-diagnosed hypertension patients two times a day increased risk by 85 % more than non-users, over a 3 year follow-up study. The association of hypertension incidence and use of mouthwash in this study were reported independent of other risk factors such as lifestyle, dietary patterns and smoking habits. Mouthwash use is for maintaining oral hygiene and improving breath; however, almost all mouthwash brands contain antibacterial components which have detrimental effects on NO bioavailability and nitrate reduction, possibly leading to hypertension incidence. Interestingly, meta-analysis conducted by Farook et al. (2024) indicated that mouthwash usage may not be linked to significant increases in SBP and DBP. However, the authors acknowledged that this conclusion may be affected by high inconsistencies of contributing studies (Farook et al., 2024).
The findings of our meta-analysis reveal a strong association between the use of antiseptic mouthwash and elevated blood pressure among adults with mild hypertension symptoms. This may support a pathogenic role of mouthwash usage in increasing the likelihood of developing high blood pressure, particularly when our assessment derives from primary studies with different study designs and population features. The increase in SBP was found to be predominant through all randomized controlled trials, cohort studies, and cross-sectional studies after daily mouthwash use. Of note, significant heterogeneity was observed between studies (I2 = 97 %), indicating variability in effects across populations and designs. This uncertainty may influence effect estimates. Subgroup analyses were not reported to explore potential sources of heterogeneity. Other limitations include a) inclusion of short-term clinical trials of the effect of mouthwash use, b) limited number of published cohort studies for pooled analysis, c) ineligibility of studies published in languages other than English, d) possibility of study-level meta-analysis rather than a patient-level meta-analysis, that would have allowed us to account for a variety of characteristics because we were unable to collect raw data. Another potential limitation is we cannot rule out the possibility of reverse causation, i.e. individuals with pre-existing hypertension and on mediation may be more likely to use mouthwash. This may indeed result in different interpretation of our results.
5 Conclusion
In conclusion, the findings revealed a slightly higher risk of hypertension among antiseptic mouthwash users who rinse their mouth daily as compared to non-users. The relationship between the use of antiseptic mouthwash and the risk of hypertension is significantly independent of other factors and potential cofounders, but more clinical trials are required to prove the recent study's hypothesis. According to our study's findings, those who used mouthwash twice or more per day had a much-increased chance of developing hypertension than those who used it less frequently or never. Significant risk factors for high blood pressure and a number of other potential variables are not associated with this link; nonetheless, further extensive long-term randomized, and blinded clinical trials are required to determine the causative relationship.
CRediT authorship contribution statement
Hala Abubaker Bagabir: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Rgad Bagabir: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ayman K. Johargy: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Hani Faidah: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ahmad O. Babalghith: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Farkad Bantun: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Faraz Ahmad: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Darin Mansor Mathkor: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Shafiul Haque: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Acknowledgements
The authors extend their appreciation to the Deputyship for Research & Innovation, Ministry of Education in Saudi Arabia for funding this research work through the Project Number ISP23-101.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Antibacterial mouthwash blunts Oral nitrate reduction and increases blood pressure in treated hypertensive men and women. Am. J. Hypertens.. 2015;28:572-575.
- [CrossRef] [Google Scholar]
- Centers for Disease Control and Prevention, 2023. National Health and Nutrition Examination Survey.
- Salt-responsive metabolite, β-hydroxybutyrate. Attenuates Hypertension. Cell Rep.. 2018;25:677-689.e4.
- [CrossRef] [Google Scholar]
- The use of ‘PICO for synthesis’ and methods for synthesis without meta-analysis: protocol for a survey of current practice in systematic reviews of health interventions. F1000Research. 2021;9:678.
- [CrossRef] [Google Scholar]
- Home oral hygiene is associated with blood pressure profiles: results of a nationwide survey in italian pharmacies. J. Clin. Periodontol.. 2022;49:1234-1243.
- [CrossRef] [Google Scholar]
- Association between mouth rinse use and changes in blood pressure: a systematic review and meta-analysis with trial sequential analysis. Int. J. Dent. Hyg.. 2024;22:65-77.
- [CrossRef] [Google Scholar]
- How to do a meta-analysis. Br. J. Math. Stat. Psychol.. 2010;63:665-694.
- [CrossRef] [Google Scholar]
- Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm hg, 1990–2015. JAMA. 2017;317:165-182.
- [CrossRef] [Google Scholar]
- The increase in plasma nitrite after a dietary nitrate load is markedly attenuated by an antibacterial mouthwash. Nitric Oxide. 2008;19:333-337.
- [CrossRef] [Google Scholar]
- Microbiological and clinical effects of an oral hygiene regimen. Contemp. Clin. Trials Commun.. 2017;8:85-89.
- [CrossRef] [Google Scholar]
- The oral microbiome and nitric oxide homoeostasis. Oral Dis.. 2015;21:7-16.
- [CrossRef] [Google Scholar]
- Oral hygiene, mouthwash usage and cardiovascular mortality during 18.8 years of follow-up. Br. Dent. J. Online Ahe 2023:1-6.
- [CrossRef] [Google Scholar]
- Over-the-counter mouthwash use and risk of pre-diabetes/diabetes. Nitric Oxide. 2017;71:14-20.
- [CrossRef] [Google Scholar]
- Over-the-counter mouthwash use, nitric oxide and hypertension risk. Blood Press.. 2020;29:103-112.
- [CrossRef] [Google Scholar]
- Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radic. Biol. Med.. 2013;55:93-100.
- [CrossRef] [Google Scholar]
- Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217-223.
- [CrossRef] [Google Scholar]
- Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of the Obesity Society and the American Society of Hypertension. J. Clin. Hypertens. (greenwich). 2013;15:14-33.
- [CrossRef] [Google Scholar]
- A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet (london, England). 2012;380:2224-2260.
- [CrossRef] [Google Scholar]
- Efficacy of chlorhexidine, xylitol, and chlorhexidine + xylitol against dental plaque, gingivitis, and Salivary Streptococcus mutans load: a randomised controlled trial. Oral Health Prev. Dent.. 2017;15:529-536.
- [CrossRef] [Google Scholar]
- The effects of chronic nitrate supplementation and the use of strong and weak antibacterial agents on plasma nitrite concentration and Exercise blood pressure. Int. J. Sports Med.. 2015;36:1177-1185.
- [CrossRef] [Google Scholar]
- Global Disparities of hypertension prevalence and control. Circulation. 2016;134:441-450.
- [CrossRef] [Google Scholar]
- Association between periodontitis and blood pressure highlighted in systemically healthy individuals. Hypertension. 2021;77:1765-1774.
- [CrossRef] [Google Scholar]
- Diagnosis and management of hypertension in obesity. Obes. Rev.. 2006;7:155-162.
- [CrossRef] [Google Scholar]
- Working group on blood pressure monitoring of the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press. Monit.. 2002;7:3-17.
- [CrossRef] [Google Scholar]
- The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg.. 2021;88:105906
- [CrossRef] [Google Scholar]
- Gastroprotective and blood pressure lowering effects of dietary nitrate are abolished by an antiseptic mouthwash. Free Radic. Biol. Med.. 2009;46:1068-1075.
- [CrossRef] [Google Scholar]
- Impact of salt intake on the pathogenesis and treatment of hypertension. Advances in Experimental Medicine and Biology. 2017;956:61-84.
- [CrossRef] [Google Scholar]
- Shaw, K.A., 2019. The Effects of Antiseptic Mouthwash Use and Sodium Intake on Systemic Blood Pressure Regulation and Salivary Nitrate Levels: A Randomized Controlled Crossover Trial.
- The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review) Vascul. Pharmacol.. 2015;71:40-56.
- [CrossRef] [Google Scholar]
- Statista Research Department, 2022a. U.S. population: Usage of mouthwash / dental rinse from 2011 to 2024 [WWW Document]. Statista.
- Statista Research Department, 2022b. U.S. population: Number of uses of mouthwash / dental rinse within 7 days from 2011 to 2020 [WWW Document]. Statista.
- Listerine® products: an update on the efficacy and safety. Phyther. Res.. 2016;30:367-373.
- [CrossRef] [Google Scholar]
- The role of dietary salt and alcohol use reduction in the management of hypertension. Expert Rev. Cardiovasc. Ther.. 2021;19:27-40.
- [CrossRef] [Google Scholar]
- Recommended software/packages for meta-analysis of diagnostic accuracy. J. Lab. Precis. Med.. 2019;4:22.
- [CrossRef] [Google Scholar]
- 2018 ESC/ESH guidelines for the management of arterial hypertension. J. Hypertens.. 2018;36:1953-2041.
- [CrossRef] [Google Scholar]
- A stepwise reduction in plasma and salivary nitrite with increasing strengths of mouthwash following a dietary nitrate load. Nitric Oxide. 2016;54:1-7.
- [CrossRef] [Google Scholar]







